Listening with text
An experienced clinician listens to the patient. This is what every doctor is taught in medical school—you can get 85% of the way toward your assessment and plan of care just by listening to the patient speak. This is one of the fundamental principles taught by Dr. William Ossler, widely described as the founder of modern medicine and professor at both Oxford and Johns Hopkins in the early 20th century. Dr. Ossler used to teach his residents: “Listen to your patient, they’re telling you the diagnosis.”
In a diffuse patient base that needs 24/7 care but may not be available the moment a doctor picks up the phone, how can you listen to the patient?
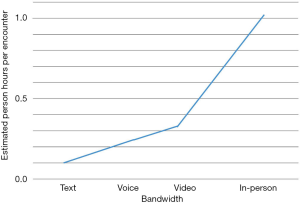
The answer—or a big part of it—is asynchronous communication. It sounds contradictory, to use text to listen, but the first step is opening up the channel, providing that first, “low touch” level of access, with the appropriate follow-up services ready to go (Figure 1).
The first step is to be available.
A patient’s ability to easily access a physician to make near-term decisions, combined with follow-on access for the physician to continue managing a patient’s care are two critical components to delivering care remotely. A lot can be determined before a patient shows up at what for many is the first touch-point, the emergency room. The ER is often the only known choice for patients to receive 24/7 diagnostic and therapeutic decision-making, at a high cost to both the patient and the payer. In reality all that’s needed, in many cases, is quick feedback from physicians experienced in clinical work.
If a patient describes certain symptoms to an experienced clinician they can use their deep understanding of medicine to determine what needs to happen next. The patient may have a quick question, or less often, need an in-person visit to get a referral to a specialist, for labs or X-rays. In the ideal healthcare system—the one we’re working towards at CirrusMD—those services will be available to a physician who can make the first, critical assessment without requiring the patient or the physician to pass through the brick and mortar clinic.
In fact, it’s already happening in large numbers. Physicians have done initial assessments for friends and family via text messaging for years. The asynchronous and remote nature of text allows an astute physician to “listen” to the patient with early 20th-century style quality of relationship over 21st-century technology. The right way to start a patient dialogue is to begin with low bandwidth and low cost (which can scale) and move progressively toward higher bandwidth communications. The progression should be “light touch” asynchronous text first, synchronous video as needed, in-person if necessary.
The benefits of providing care in this way are impressive. We get high utilization with no co-pays on a technology with which individuals are already familiar. In addition, we get high re-engagement from patients who have great experiences with the doctor, and great compliance with only a fraction of encounters leading to in-person care, an overall savings of about $900 per encounter.
We’re getting results with patients in Colorado and Texas along five key measures: utilization, re-engagement, compliance, response time, and overall savings.
- In Texas we achieved 11.6% utilization of our services within just 3 months of launching within a scaled population, after 6 months we passed 15% utilization. That rapid uptake is being driven by our services not involving a co-pay while providing continual access to a doctor. Most large telemedicine services get less than 3% utilization even after years in the marketplace.
- As a result of providing a closed-loop offering where we can provide follow-on care as needed and create great user experiences, 22% of our users re-engaged with our service within 3 months.
- Our data shows that 96% of users don’t end up in urgent care or the ED after a virtual encounter. The other 4% are referred in; these people said they would have gone to the ER or urgent care anyway.
- As a result of our asynchronous communications, our average response times are less than 2 minutes. Around 85% of our encounters are text-only; 99% include text as a component. This is unique, as other major telemedicine providers see more than 95% of their encounters take place by phone only, creating continuity issues and making them expensive and difficult to scale.
- By asking our patients what they would have done without access to the service and taking a weighted average of diversion from various points of care against our physicians’ opinions on whether the patient would have come to an on-site visit and what it would have cost, we are able to determine a savings of roughly $900 per encounter.
It may seem like having physicians on call is expensive and difficult to scale. That would be true if communications are exclusively one-on-one via phone or video. But by using an asynchronous text messaging-first workflow, we can have doctors ready to care for as many as five patients at a time. Layering in the ability for the doctor to receive pictures and initiate a video chat at any time adds dimensionality and expands the information available to the doctor so they can effectively get to the right decision sooner, delivering care while realizing savings by removing the intermediaries. That means better experiences for patients and, we believe, better outcomes overall—the key consideration in providing value-based care. The goal is long-term outcomes, so it only makes sense to lower near-term costs if we can provide more immediate care from people trained to make the best possible near-term decisions.
Observing a patient through high-quality video or text messaging can be the same as pulling back the curtain in the emergency room. Let’s say we have a patient telling a doctor over text messaging that for the past day and a half they’ve experienced burning with urination, just like when they had a UTI last year. This is a young, healthy, non-pregnant woman with no other medical issues who is pretty sure she has a UTI. Evidence-based medicine says a physician can listen to that story and it can only be one thing, a UTI. The right thing to do is to provide a short course of a non-allergic antibiotic for the patient and to provide her with a way to reach back to the doctor if she gets worse.
We can enable a future where incentives are designed so the overall costs of treating a patient longitudinally can be minimized while the health of the patient is maximized. The continuum of care is managed using the technology our patients carry in their pockets and keep in their bedrooms. That same technology allows healthcare systems to record the data being created when a patient and physician engage in conversation or diagnosis over these platforms. Just imagine being free from billing in-person encounters for more than 80% of cases. It’s already being done, and being done well.
Acknowledgements
Thanks goes to Leonard Kish and Rebecca Sunshine for their editing and proofreading support of this manuscript.
Footnote
Conflicts of Interest: The submitting authors are both co-founders of CirrusMD—a telemedicine solution for value-based healthcare organizations. Patients can be treated virtually through secure text messaging, image sharing and video visits. All patient encounter data can be integrated into the patient’s primary medical record, and doctors staffing the service also have access to the medical record for both physical and virtual encounters.
Cite this article as: Altorfer A, McKinney B. Listening with text. mHealth 2016;2:15.