
m-Health views and perception among Malaysian: findings from a survey among individuals living in Selangor
Introduction
Health literacy is defined as the cognitive and social skills which determines the motivation and ability of individuals to gain access, understand and use information needed to promote, maintain and improve health (1,2). Research have shown that individuals with low health literacy have poorer engagement with health care services as well as lower knowledge of chronic disease process leading to higher hospitalization rates (2-4). A low level of health literacy was also commonly found in many low income countries as well as ethnic minorities; and is thought to explain some of the inequities in the uptake and use of health care services in many parts of the world (5).
Information and communication technologies (ICTs) are now increasingly being used in various aspects of healthcare, including management of patients with chronic diseases such as diabetes and hypertension; during routine interactions with healthcare systems such as making appointments; as well as medication refills. ICT is also used by healthcare professionals to distribute information or expertise necessary to geographically separated individuals such as patients or other consulting physicians (6-10), and has been advocated as a cost-effective solution for patients, healthcare professionals, healthcare providers, as well as health authorities in helping to address contemporary global health problems (11).
This innovation in healthcare can reduce health disparities, as it can lower health literacy demand through the use audio graphics and multiple languages to expand the capacity and reach of healthcare system. It is however unclear what are the utilization rates and role of the internet and in particular mobile health (m-health) apps in supporting the health among the general public here in Malaysia. Similarly, there is very little information on the usage of internet or m-health to perform any health related task online among individuals with limited health literacy. In this study, we explored the users’ technology literacy and internet usage among individuals, in order to have a better understanding of issues related to m-health in different segments of the population.
Methods
Respondents
This was a nested study (12,13) using convenience sampling where respondents were randomly recruited from public areas (e.g., shopping malls, parks, government hospitals, primary care clinics as well as public and private universities) in the Klang and Petaling district in the state of Selangor from November 2015 to January 2017. Inclusion criteria of respondents were: aged 18 years and older; able to speak and read English, Mandarin or Malay language and were able to provide informed consent. To ensure we are able to recruit a representative demographic profile of respondents, we approached individuals of all ages and gender.
Ethical approval
No compensation was provided for study participation. The study protocol was reviewed and approved by the Medical Research and Ethics Committee, Malaysia (NMRR-14–1453-22963) and Monash University Human Research Ethics Committee (CF14/1977–201456345463). All respondents provided written informed consent. All methods were performed in accordance with the relevant national and international guidelines and regulations.
Survey instrument
Respondents were asked to complete a battery of self-administered questionnaire. The questionnaire was developed and adopted from reviewing existing literature and previous studies that have examined on the use of m-health and mobile health devices for health literacy (14-19). The questionnaire comprised of three sections: (I) respondent demographics such as age, gender, ethnicity, employment and marital relationship and education; (II) baseline health status including self-reported diseases (e.g., diabetes, cardiovascular diseases, cancer) as well as health behaviors (smoking and alcohol consumption frequency) and; (III) use of ICTs to seek for health related information to assessing cellphone/smartphone ownership, access and usage of internet, and internet/apps to obtain health information. In the latter component of the questionnaire, respondents were asked to rate on a 5-point Likert scale about their preference regarding their ability to understand health information, attitudes towards heath, and access to healthcare information.
The questionnaire was subsequently piloted among a convenience sampling of 50 individuals, and was found to have an acceptable validity and reliability (data presented separately). The questionnaire was also translated into Bahasa Malaysia (the local language) and Mandarin to suit respondents whom the English language was not their first language using forward and backward translation by three independent reviewers whose Bahasa Malaysia and Mandarin were their first language. The final translated instrument was used in this study.
Use of mobile health devices and m-health apps
To determine the acceptance of m-health among individuals, we use the following question: "Have you used any mobile health devices or m-health for managing your health?” Specifically, participants were provided with examples of a mobile health device such as diabetes telemonitoring device, as well as teleconsultation devices. Examples of m-health apps include health monitoring app to encourage exercise, weight loss or track personal health information. Respondents were coded as willing to accept if they reported agree or strongly agree while respondents who disagree or strongly disagree were coded as not willing. We also examined factors which may affect health information seeking behavior, as previous studies have suggested that mobile device ownership are related to the availability of Internet access.
Statistical analysis
All categorical variables were described with frequencies and percentages. All continuous variables were summarized using mean and standard deviations (SD) for normally distributed data or median and interquartile range if data were skewed. To investigate the factors affecting respondent’s ICT use and acceptance of m-health, chi-square tests and Pearson’s correlation was used.
We conducted several logistic regression analyses to determine the relationship between use of m-health and ICT with respondent demographics. Firstly, we hypothesized that there were generational differences in ICT use between millennial (aged 39 and below) and baby boomers (aged 50 and above). We calculated the relationship using multiple logistic regression analysis using a hierarchical model. All multivariate model included the use of m-health and ICT use as the dependent variables, while respondent demographics, socioeconomic status, and baseline health measures were independent models. In secondary analyses we tested for differences in the association between ICT use by age, gender, education, or existing chronic disease by adding interaction terms into separate regression models. Significance level for all statistical analysis was P<0.05. All analyses were performed using Statistical Package for Social Sciences (SPSS) software version 22 (Armonk, NY, IBM Corp.).
Results
Socio-demographic characteristics of respondents
A total of 4,504 respondents responded to our study during this period, with an almost equal number of males and females (ratio 1:1.17). Most of the respondents were married (74.2%), with a median age between 41–50 years, and had had some form of formal education (92.3%). The respondents were ethnically diverse, which included Malays (42.2%), Chinese (24.7%), Indian (27.4%) and other ethnic groups (5.7%) and usually lived with their family members (Table 1). The demographics of participants are generally representative of the population in Malaysia, although a higher number of Indians were recruited in this study.

Full table
Electronic device ownership
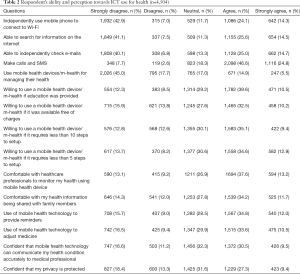
All respondents reported that they owned at least one electronic device (63.6%), the most common being either a mobile or smartphone. The device was mostly used to make telephone calls and deliver text messages. However, up to 44% of respondents reported that they required some assistance from friends and family to use the device. The most common issues respondents needed help with were: connecting their device to a wireless network (49.9%), searching for information on the Internet (48.6%), and checking emails (46.9%; Table 2).
Full table
Ability for self-care
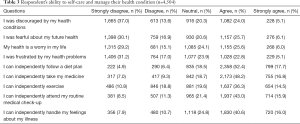
Most respondents reported that they were positive with their current and future health state. However, nearly half of respondents (48.2%) surveyed expressed concern about their health and were frustrated by their health problems. Most respondents reported that they were able to follow a healthy diet (70.1%), take their medications independently (65.0%) as well as perform routine exercise (57.2%, Table 3).
Full table
Respondents reported that they did not feel they had received adequate support from their friends and family in various aspects of their health such as maintaining a healthy diet, taking their medication, exercising regularly, attending routine medical check-ups, or handling their emotional needs in relation to their illness. A large proportion of respondents also reported poor compliance to following instructions of their healthcare providers, with 30.3% of respondents reported stopping their medication when they feel better while 24.5% respondents stopped their medication when it made them feel worse.
Perception of m-health
Only one in every five respondents in the survey reported that they had used some health related application/mobile health device. The most commonly used device were adherence aids, or an application that was pre-installed with their glucose meters for self-efficacy (e.g., receiving information, lifestyle advice). Most respondents also reported that they had limited knowledge regarding m-health or mobile health devices but were willing to use these devices if it were provided at no cost to respondents (42.7%). Interestingly, there was very little benefits of making the device more user friendly as respondents reported that it will not increase their willingness to utilize the device.
Nearly one in every two respondents also reported they were comfortable to share their health information with their healthcare professional or family members. Although respondents were optimistic about the benefits of mobile technology (e.g., receiving doctor’s instructions and consultations), some expressed concerns on the accuracy of the data as well as their own personal privacy (Table 2).
Generational differences in healthcare preference
We stratified our analysis to determine if there were generational differences in healthcare preference between millennial and baby boomers. We found that most millennial owned two or more devices compared to baby boomers (61.1% vs. 9.4%, P<0.01). Baby boomers were also less inclined to use m-health as a health management strategy. Providing this group with additional support (e.g., additional education, creating simple video instructions) did not alter their opinion and intent about m-health. Conversely, millennials were more inclined to use m-health for consultation, medication management (e.g., reminders, blood glucose recording), lifestyle education and receive reminders on their appointments. They were also more likely to obtain and share health related advice online with their family and friends. However, both groups expressed concerns on privacy protections especially with the use of m-health.
Predictors of m-health app usage
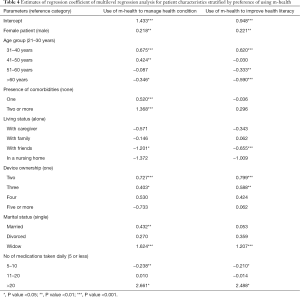
Younger females especially those who own 2 or more electronic devices, those with higher education levels, were widows, and taking more than 20 medicines were more likely to embrace technology and use m-health to obtain health related information. We also noted that those who were married or had medical illnesses were more likely to use m-health to manage their health condition (Table 4).
Full table
Discussion
This study was designed to elucidate and assess the Malaysians’ ICT use in order to learn whether patients were interested in using m-health for chronic disease management. We found that younger individuals aged 39 and below, those with higher educational status and those who owned 2 or more mobile devices were more interested in adopting and using m-health and health related applications in their daily lives. The most common health services/application which they would use are the medication reminder, telemonitoring and teleconsultation services. Result of this study concurs with previous studies that have shown that the younger generation who grew up with technology was more inclined to adopt technology in managing their health issues (20-22). Furthermore, as younger respondents were more technology savvy compared to their older peers, this allows for an easier adoption of technology among the younger population whenever new technologies are introduced. Results of this study also concur with a previous study conducted in Malaysia, which showed that Malaysians were receptive to use technology to seek for health related information, including obtaining information about the health condition, its symptoms and treatment options available (23-26).
The use of m-health can be a useful strategy to expand health care and empower individuals to monitor their own health and potentially reduce the cost of medical care (11). Malaysia as a developing country with a robust technology economy can be expected to benefit from the use of m-health services due to its high Internet and broadband penetration rates as well as high mobile penetration at 144.8%, indicating that most Malaysians currently own more than one mobile device (24). However, there is little research on how much interest in m-health exists among the Malaysian public. The feasibility of implementation of m-health in a primary care setting remains unclear. Results of this study suggest that m-health can be a feasible modality to assist Malaysians in taking charge of their own chronic condition. However, results from this study also suggest that most respondents were somewhat interested in using technology to manage their health. This result was similar to other studies performed to date (16,22,27). In a study by Samiei et al., the authors reported that only 56.1% of respondents in Malaysia were interested in using Internet-based self-management program (28). This could be due to several reasons, including participants preference for face-to-face communication with their healthcare providers (29,30), limited understanding of the various functions of a smartphone as well as issues with the cost of embracing such technology (9).
The success and implementation of any m-health program depends upon the acceptance of users and healthcare professionals. A study by Ibrahim et al. reported that healthcare professionals were positive in their views about m-health (20). However, many of them still value face-to-face communication with their patients and consider direct communication with patients as important, especially prior to performing any procedure on a patient (25,26). The authors also reported that in order to improve users’ acceptance of m-health, there is a need for additional education and training. This concurs with results of this study, where respondents reported that they were more willing to use a mobile health device if education was provided and if the procedure of using a mobile health device was simple.
Overall, results from this study showed that although respondents were optimistic about their current and future health, many individuals still require support in various lifestyle-related activities such as engaging in regular exercise, and emotional support. Due to the increasing innovation in medical devices and application such as wearables, remote monitoring, on-call doctors, online support groups, and various other technological innovation coupled with the increased connectivity in Malaysia, respondents had access to services that were specifically tailored to their needs. Unfortunately, as many as 62% of respondents had no knowledge that such m-health services existed. Similarly, less than half of the respondents viewed that m-health was beneficial in managing their health. This could have led to the lack of interest of respondents to use health management technologies. Additionally, slow connectivity, incompatibility of software and hardware, insufficient understanding of the benefits of m-health could be a possible reason for the low interest in utilizing m-health. Privacy of data and sharing of information with family members is another concern among respondents (29-31). As such, education initiatives are required to inform the Malaysian public on the benefits of m-health in managing their health as well as promote self-care management. This needs to go hand in hand with government policies to further promote the use of m-health.
Although results of this survey showed that millennial were more inclined to use m-health and mobile health applications compared to baby boomers’, the adoption of m-health was not encouraging as only half of the millennial were willing to use m-health to manage their health. As this generation is usually younger and healthier, these factors could possibly explain the lack of urgency to maintain their health leading to the lackluster uptake of m-health. A low inclination on the use m-health amongst baby boomers was expected as respondents’ view that the use of technology was unable to improve their health compared to conventional methods. Furthermore, these respondents reportedly showed a lack of interest to adopt and learn newer technologies such as m-health to care for their health. Therefore, this needs to be taken into consideration in any future policy implementation since most respondents felt that the current conventional monitoring methods were the best solution for them.
This study has several limitations which need to be taken into context. Firstly, results of this study are limited by the sampling method used. While we attempted to recruit as many and representative sample as possible using proportionate sampling, this was not feasible the limited resources we had. We were only able to compare the demographics between our cohort versus the general population in several parameters, namely gender, ethnic and age groups only. This was because these were the only data publically available and our attempt to have access to other data was not granted. However, the demographic profile of our respondents is generally similar to Malaysians in general, albeit higher proportion of Indian recruited in the sample (32), lending credibility to the findings. In addition, we had not examined the test-retest reliability of the questionnaire due to the cross-sectional design of the study. The samples were recruited from two districts which were semi-urban and urban setting and thus may not represent the opinion of those living in rural settings or other regions of the country. Finally, our questionnaire had examined limited domains to examine the reasons behind different reasons and preference for m-Health adoptions among participants. Nevertheless, we plan to explore the reasons for these differences in our qualitative research in the future.
In summary, m-health has the potential to bring about pragmatic changes to healthcare. Results of this study suggest that respondents were receptive to use m-health if sufficient training and education were provided. While resistance towards adopting new technology is common, a holistic approach involving the participation of various stakeholders such as academics, industry players, healthcare professionals and early adopters are required for the effective implementation of m-health.
Acknowledgments
The authors acknowledge the support from respondents, clinics, hospitals as well as shopping malls in ensuring the success of this study.
Funding: This study was funded by an unrestricted grant from the e-Science fund from the Ministry of Science, Technology and Innovation, Malaysia [03-02-10-SF0238 (MOSTI)].
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study protocol was reviewed and approved by the Medical Research and Ethics Committee, Malaysia (NMRR-14–1453-22963) and Monash University Human Research Ethics Committee (CF14/1977–201456345463). All respondents provided written informed consent. All methods were performed in accordance with the relevant national and international guidelines and regulations.
References
- World health Organization, editor. Track 2: Health literacy and health behaviour. 7th Global Conference on Health Promotion; 2009; Nairobi, Kenya.
- Institute of Medicine (US) Committee on Health Literacy. What Is Health Literacy? In: Nielsen-Bohlman L, Panzer AM, Kindig DA, editors. Health Literacy: A Prescription to End Confusion. Washington (DC): National Academies Press (US), 2004.
- Gazmararian JA, Williams MV, Peel J, et al. Health literacy and knowledge of chronic disease. Patient Educ Couns 2003;51:267-75. [Crossref] [PubMed]
- Berkman ND, Sheridan SL, Donahue KE, et al. Low health literacy and health outcomes: an updated systematic review. Ann Intern Med 2011;155:97-107. [Crossref] [PubMed]
- United Nations Economic and Social Council (ECOSOC). Health literacy and the Millennium Development Goals. J Health Commun 2010;15 Suppl 2:211-23. [Crossref] [PubMed]
- Martin Morales A, Hatzichristou D, et al. Community pharmacy detection of erectile dysfunction in men with risk factors or who seek treatment or advice but lack a valid prescription. J Sex Med 2013;10:2303-11. [Crossref] [PubMed]
- Institute of Medicine Committee on Evaluating Clinical Applications of Telemedicine. The National Academies Collection: Reports funded by National Institutes of Health. In: Field MJ, editor. Telemedicine: A Guide to Assessing Telecommunications in Health Care. Washington (DC): National Academies Press (US), National Academy of Sciences, 1996.
- Masys DR. Telemedicine: A Guide to Assessing Telecommunications in Health Care. J Am Med Inform Assoc 1997;4:136-7. [Crossref]
- Lee SWH, Chan CKY, Chua SS, et al. Comparative effectiveness of telemedicine strategies on type 2 diabetes management: A systematic review and network meta-analysis. Sci Rep 2017;7:12680. [Crossref] [PubMed]
- Lee SWH, Ooi L, Lai YK. Telemedicine for the management of glycemic control and clinical outcomes of type 1 diabetes mellitus: A systematic review and meta-analysis of randomized controlled studies. Front Pharmacol 2017;8:330. [Crossref] [PubMed]
- Lee JY, Lee SWH. Telemedicine Cost-Effectiveness for Diabetes Management: A Systematic Review. Diabetes Technol Ther 2018;20:492-500. [Crossref] [PubMed]
- Lee JY, Chan CKY, Chua SS, et al. Intervention for Diabetes with Education, Advancement and Support (IDEAS) study: protocol for a cluster randomised controlled trial. BMC Health Serv Res 2016;16:524. [Crossref] [PubMed]
- Lee JY, Chan CKY, Chua SS, et al. Telemonitoring and Team-Based Management of Glycemic Control on People with Type 2 Diabetes: a Cluster-Randomized Controlled Trial. J Gen Intern Med 2019. [Epub ahead of print]. [Crossref] [PubMed]
- Jayasinghe UW, Harris MF, Parker SM, et al. The impact of health literacy and life style risk factors on health-related quality of life of Australian patients. Health Qual Life Outcomes 2016;14:68. [Crossref] [PubMed]
- Alaboudi A, Atkins A, Sharp B, et al. Barriers and challenges in adopting Saudi telemedicine network: The perceptions of decision makers of healthcare facilities in Saudi Arabia. J Infect Public Health 2016;9:725-33. [Crossref] [PubMed]
- Jung SG, Kweon HJ, Kim ET, et al. Preference and Awareness of Telemedicine in Primary Care Patients. Korean J Fam Med 2012;33:25-33. [Crossref] [PubMed]
- Rajah R, Hassali MA, Lim CJ. Health Literacy-Related Knowledge, Attitude, and Perceived Barriers: A Cross-sectional Study among Physicians, Pharmacists, and Nurses in Public Hospitals of Penang, Malaysia. Front Public Health 2017;5:281. [Crossref] [PubMed]
- Aryani FMY, Lee SWH, Chua SS, et al. Chronic care model in primary care: can it improve health-related quality of life? Integr Pharm Res Pract 2016;5:11. [PubMed]
- Chongmelaxme B, Lee S, Dhippayom T, et al. The effects of telemedicine on asthma control and patients' quality of life in adults: a systematic review and meta-analysis. J Allergy Clin Immunol Pract 2019;7:199-216.e11. [Crossref] [PubMed]
- Ibrahim MIM, Palaian S. Evaluation of knowledge and perception of Malaysian health professionals about telemedicine. J Clin Diagn Res 2010;4:2052-7.
- Feil EG, Glasgow RE, Boles S, et al. Who participates in Internet-based self-management programs? A study among novice computer users in a primary care setting. Diabetes Educ 2000;26:806-11. [Crossref] [PubMed]
- Zailani S, Gilani MS, Nikbin D, et al. Determinants of Telemedicine Acceptance in Selected Public Hospitals in Malaysia: Clinical Perspective. J Med Syst 2014;38:111. [Crossref] [PubMed]
- Malaysian Communications and Multimedia Commission. MCMC Internet User Survey 2017. Cyberjaya, Malaysia: Malaysian Communications and Multimedia Commission, 2017.
- Malaysian Digital Association 2016 Malaysia Digital Landscape: Exploring The Digital Landscape in Malaysia Boosting Growth for A Digital Economy 2016. Available online: http://www.malaysiandigitalassociation.org.my/wp-content/uploads/2016/08/Malaysia-Digital-Landscape-August-2016.pdf, accessed 14 May 2017.
- Kua KP, San Saw P, Lee SWH. Attitudes towards deprescribing among multi-ethnic community-dwelling older patients and caregivers in Malaysia: a cross-sectional questionnaire study. Int J Clin Pharm 2019;41:793-803. [Crossref] [PubMed]
- Lee JY, Chan CKY, Chua SS, et al. Using telemedicine to support care for people with type 2 diabetes mellitus: A qualitative analysis of patients' perspectives. BMJ Open 2019. [Crossref] [PubMed]
- AlDossary S, Martin-Khan MG, Bradford NK, et al. A systematic review of the methodologies used to evaluate telemedicine service initiatives in hospital facilities. Int J Med Inform 2017;97:171-94. [Crossref] [PubMed]
- Samiei V, Wan Puteh SE, Abdul Manaf MR, et al. Are Malaysian diabetic patients ready to use the new generation of health care service delivery? A telehealth interest assessment. Malays J Med Sci 2016;23:44-52. [PubMed]
- Lee JY, Wong CP, Tan CSS, et al. Telemonitoring in fasting individuals with Type 2 Diabetes Mellitus during Ramadan: A prospective, randomised controlled study. Sci Rep 2017;7:10119. [Crossref] [PubMed]
- Lee JY, Wong CP, Tan CSS, et al. Type 2 diabetes patient’s perspective on Ramadan fasting: a qualitative study. BMJ Open Diabetes Res Care 2017;5:e000365. [Crossref] [PubMed]
- Lee JY, Lee SWH, Nasir NH, et al. Diabetes telemonitoring reduces the risk of hypoglycaemia during Ramadan: a pilot randomized controlled study. Diabet Med 2015;32:1658-61. [Crossref] [PubMed]
- Department of Statistics Malaysia. Vital Statistics, Malaysia 2018. Department of Statistics, Malaysia, Putrakaya 2019. Available online: https://www.mycensus.gov.my/geostats/report.php, accessed 30 November 2018.
Cite this article as: Lee JY, Wong CP, Lee SWH. m-Health views and perception among Malaysian: findings from a survey among individuals living in Selangor. mHealth 2020;6:6.


