
Assessing the utility of an IoS application in the perioperative care of spine surgery patients: the NeuroPath Pilot study
Introduction
Two converging crises in healthcare are approaching; escalating costs of care (1,2) and a US opioid epidemic (3). Tools available to the clinician to optimize outcome, thereby reducing costs of interventions, narcotic usage and need assessment subsequent to surgical intervention are lacking in current practice. Therefore, there is a need for a low-cost tool that helps the clinician optimize outcome while more closely monitoring surgical recovery and opioid usage.
Goals to improving care, including increasing quality and decreasing cost, are often competing and challenging to fulfill. A potential opportunity to achieve these goals is to align care in a central location that empowers action by patients and providers. Having had success previously in building a tool to enhance to enhance the EHR (the NQII EpiLog project) (4-10), we leveraged that experience to build a patient and provider facing streamlined instrument. The platform supports the goals of opioid monitoring and reductions, wound care, enhanced activity after surgery, and enhanced recovery after surgery (ERAS).
ERAS is a multidisciplinary approach to surgical care involving surgeons, anesthetists, an ERAS coordinator, and additional staff involved in patient care (11). This approach has been utilized within our department and shown promising results to date (12). Departments that have implemented ERAS protocols have seen encouraging results: shortened length of stay, reduction in costs, readmissions, complications, and decreased postoperative pain (11,13-15). Finding protocols that can limit postoperative pain is of the utmost importance, as the opioid epidemic continues to rise in the US. The origin of this epidemic is often credited to the shift in pain management toward regarding pain as the fifth vital sign, which was followed by a sharp increase in narcotic prescriptions from 1999–2010 (3,16). Applying ERAS to reduce post-operative opioid use was found to be effective in a previous pilot study by Rojas et al., eliminating narcotic prescription completely following lumpectomy (15).
Aside from ERAS, novel attempts to improve healthcare delivery are being devised to a large extent through the development of mobile health (mHealth) applications. Health mobile applications have inundated the marketplace over the last decade, covering a vast array of health and wellness topics. With this emerging area of care, extensive research has been done to evaluate the efficacy of mHealth apps. The benefit of these apps is well documented in improving patient feeling of participation in their care, sense of security, self-confidence and well-being, including increasing physical activity (17-19). Applications have been studied for utility in postoperative care, allowing patients to be followed from home rather than staying in the hospital (20).
The literature supports the concept that self-management applications should provide education, treatment organization, communication with the care team, ways of tracking progress, and simple graphics (17,21-24). Further, a recent report by Nathan et al. found that 76% of patients undergoing spine surgery at one academic medical center were interested in using a mobile app to track postoperative progress and communicate with their surgeon (25). Using these principles, with the ultimate goal of improving care while decreasing costs and postoperative pain, our department developed a novel mobile health application, NeuroPath, designed for patients scheduled to undergo surgical intervention. The objective of this innovative app is to integrate ERAS principles, patient education, and real-time pain and activity monitoring in a home setting.
With the support of the Department of Neurosurgery, the NQII EpiLog project and Health System IS support, we developed an IOS app and piloted use in thirty consecutive spinal surgery patients, to assess the efficacy of our mHealth application to achieve the aforementioned goals.
Methods
The NeuroPath application was built over 18 months, with support from Apple and the Department of Neurosurgery at our institution. Target areas addressed by NeuroPath include patient prep for surgery, perioperative risk mitigation, activity monitoring, wound care, and opioid use management. These target areas are monitored through a provider app, which is downloaded to the care providers IPad Mini. The provider app permits real time viewing of wound healing, activity levels, and pain levels. Patients have activity levels tracked through their IPhone health app, which automatically uploads data to NeuroPath.
Participants are given a daily To-Do list, via the Care Card section of the interface. The To-Do list presents the patient with specific tasks for exercise (i.e., Go for a walk twice today for 5 minutes), instructions to wash the incision area (with video example), pre-operative instructions, and directions for discussing medication with care team (i.e., Discuss holding NSAIDs, Coumadin), among other suggestions dependent on time since surgery. The Care Card also offers recommendations, such as increase activity from prior day and eat a regular diet. Additionally, included in the Care Card section is an assessment tab, where patients are encouraged to report symptoms daily. Once all items from the To-Do list are completed and symptoms are reported, the Care Card section is considered 100% complete and denoted with a star on the patients’ calendar.
The provider app allows for care team members to give feedback to patients based on uploaded information. Active patients are sorted into pre-operative, surgery day, peri-operative, and post-operative categories. Care providers are able to view all patients in each category in a list format, showing a brief trend summary. Information included in the trend summary are patient name, gender, age, last login, surgeon, last reported narcotics usage, steps/day, last uploaded wound picture, and the number of days since the operation. Individual trends are shown graphically on both the patient and provider app. This approach affords the patient and provider real-time updates of recovery, with the opportunity for communication between both parties.
The goal of this pilot study was to enroll 30 patients and evaluate the NeuroPath app for accessibility, ease of use, ease of implementation (regarding patient education, workflow), and receiving patient feedback. Only patients scheduled for elective spine surgery were enrolled in this study, during the history and physical portion of their pre-operative visit. Enrolled patients were required to have an Apple ID and were sent an invitation to download the app via the scheduling nurse. Feedback from study participants was received by telephone interview within months of study completion. This study was considered a quality improvement effort by our university’s Institutional Review Board (IRB), thus not requiring patient consent.
Results
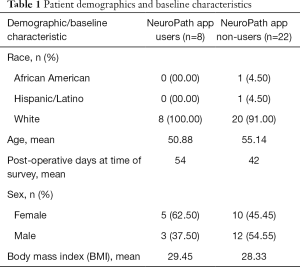
Of the 30 patients enrolled in the pilot study, there was a range of activity on the app. The patients who participated in the pilot study all underwent a follow-up survey, within 90 days post-op, regarding their experience with the app. Demographic data for these patients was collected (Table 1). Patients were grouped into two cohorts for the survey; users and non-users. Non-users were grouped as participants that logged one or two days of incomplete information pre-operatively, with no post-operative data input. Users were considered as patients with high involvement in the app, having logged in nearly every day from a week pre-op to >45 days post-op.
Full table
Survey results
After grouping patients into two cohorts, 8 (26.7%) were considered users and 22 (73.3%) were considered non-users. When evaluating why the non-user group (n=22) chose not to use the app, 6 (27.3%) felt the app would not be helpful upon hearing the initial description and 8 (36.4%) had difficulty with registering. When asked the primary reason for not using the app, 8 (36.4%) reported they did not remember to use it, 6 (27.3%) did not feel it was helpful, 4 (18.2%) could not figure out how to use the app, and 4 (18.2%) could not figure out how to use the app. When asked what they would change about the app, 5 (22.7%) respondents would have liked more instructions in the app, 4 (18.2%) wanted improved registration, 4 (18.2%) would have liked a better description of the app during their initial visit, and 9 (40.9%) respondents requested a change other than these options. When asked about their readiness to adapt new technologies, 14 (63.6%) members of this cohort stated that they wait before trying a new technology and 6 (27.3%) of these respondents were concerned about data security.
When evaluating feedback from the user group (n=8), 0 had difficulty with registering. When asked which component of the app they found most helpful, 5 (62.50%) respondents chose the daily reminders and 3 (37.50%) selected the graphical representation of their trends (step count, pain level, flights of stairs climbed). The cohort was asked about whether or not they found specific components of the app helpful. Eight (100.00%) responded yes for the daily to-do list, 4 (50.00%) responded yes for the wound pictures, 6 (75.00%) replied yes for the walking measures, 5 (62.50%) responded yes for the pain level tracking and 1 (12.50%) replied yes for communication with the care team. Five (62.50%) members of this cohort always try a new technology, while 3 (37.50%) wait prior to adapting new technology and 1 (12.50%) of these respondents were concerned about data security.
Discussion
To our knowledge, the NeuroPath pilot is the first prospective analysis of Mobile Health technology in patients undergoing spine surgery. Our study demonstrates that the NeuroPath app, through the integration of ERAS principles, communication, education, daily monitoring and patient-involvement strategies, exhibited the potential to reduce opioid use, improve knowledge, and enhance quality of life, as evidenced by reduced pain and increased ambulation.
Previous studies have shown that mHealth apps are an effective approach to ensure continuity of care and patient self-monitoring (17,18,20). With the development of improved mobile technology, smartphones and mobile apps have become increasingly popular healthcare tools. Recent studies have shown the potential benefits of using mobile apps as either self-management tools or in combination with interventions. Fukuoka et al. found that a mobile app was cost-effective and convenient to deliver proven weight-loss interventions, including increased physical activity, to patients with type 2 diabetes mellitus (19). Wang et al. tested a mobile app for follow-up care of patients discharged with a stoma, which resulted in improvement of psychosocial adjustment level and self-efficacy (20). Armstrong et al. showed that follow-up care management could be delivered via mHealth app, rather than during in-person follow-up visits, over the first 30 days following breast reconstruction surgery (26).
Our pilot study of the NeuroPath app supports previous work in the literature showing there is utility for mHealth apps, with regard to patient monitoring, in an outpatient setting. This study is the first time that a mobile app has been used as the platform for post-operative treatment and monitoring amongst spine surgery patients. Utilization of the home care mobile app was a new modality for monitoring progression of pain, wound healing, physical activity, and two-way communication, ultimately assisting in self-management. Results were positive for patients who were active users of the app. Thus, future studies should focus on improving upon the percentage of patients that maximized their use of the app, predominantly through enhanced explanation of the app during the patients’ initial visit and building additional daily reminders in to the app.
The NeuroPath mobile app examined in this study is currently only available to registered iPad users who underwent spine surgery at our institution. The practice of using smartphone apps as a tool to improve patient care is still in its infancy. Nevertheless, this study builds upon prior work that shows spine surgery patients are a welcoming population for this technology (25). Thus, future studies are necessary to optimize the potential of mHealth apps to improve patient care while reducing costs and postoperative pain. We believe that this app, which makes use of previously validated ERAS principles and daily monitoring, necessitates further study in a larger spine surgery patient population.
Limitations
There are a number of limitations in this study. This was a sample size of convenience, sourced from one academic medical center, thus selection bias could exist. Moreover, the population receiving spine surgery tends to be of advanced age, potentially confounding upon issues of adaptation of the NeuroPath app. Finally, the impact on clinical outcomes of the NeuroPath app needs to be established in a larger cohort of patients or in a long-term prospective study with clinical outcome data. This was not the goal of the present study, as the focus was to identify if there was potential utility for the NeuroPath app and what barriers to adaptation would arise. Despite these limitations, the present study shows that for the cohort who were active on the app, patients' involvement in self-care afforded the opportunity for enhanced recovery and a positive post-operative experience, highlighting an effective support management strategy in spine surgery patients.
Conclusions
The pilot NeuroPath trial is the first prospective analysis of Mobile Health technology in patients undergoing spine surgery, demonstrating that an approach integrating ERAS principles, communication, education, daily monitoring, and patient-involvement strategies has the potential to translate to reduced opioid use, improved knowledge and enhanced quality of life.
Acknowledgments
The Bernadette and Kevin McKenna Family Research Fund.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: This study was approved by the IRB at the Hospital of the University of Pennsylvania and considered exempt from full review. All ethical guidelines and rules were followed to protect patient privacy. The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
References
- Morgan L. US Healthcare Annual Spending Estimated to Rise by 5.8% on Average Through 2024. Am Health Drug Benefits 2015;8:272. [PubMed]
- Levine DM, Ouchi K, Blanchfield B, et al. Hospital-Level Care at Home for Acutely Ill Adults: a Pilot Randomized Controlled Trial. J Gen Intern Med 2018;33:729-36. [Crossref] [PubMed]
- Ostling PS, Davidson KS, Anyama BO, et al. America's Opioid Epidemic: a Comprehensive Review and Look into the Rising Crisis. Curr Pain Headache Rep 2018;22:32. [Crossref] [PubMed]
- Gawande AA. Why Doctors Hate Their Computers. The New Yorker 2018 (November 12, 2018).
- Agarwal P, Ramayya AG, Osiemo B, et al. Association of Overlapping Neurosurgery with Patient Outcomes at a Large Academic Medical Center. Neurosurgery 2019. [Epub ahead of print]. [Crossref] [PubMed]
- Glauser G, Agarwal P, Ramayya AG, et al. Association of Surgical Overlap During Wound Closure with Patient Outcomes Amongst Neurological Surgery Patients at a Large Academic Medical Center. Neurosurgery 2019. [Epub ahead of print]. [Crossref] [PubMed]
- Berger I, Piazza M, Sharma N, et al. Evaluation of the Risk Assessment and Prediction Tool for Post-Operative Disposition Needs After Cervical Spine Surgery. Neurosurgery 2019. [Epub ahead of print]. [Crossref] [PubMed]
- Caplan I, Sinha S, Schuster J, et al. The Utility of Cervical Spine Bracing as a Postoperative Adjunct to Single-Level Anterior Cervical Spine Surgery. Asian J Neurosurg 2019;14:461-6. [Crossref] [PubMed]
- Piazza M, Sharma N, Osiemo B, et al. Initial Assessment of the Risk Assessment and Prediction Tool in a Heterogeneous Neurosurgical Patient Population. Neurosurgery 2019;85:50-7. [Crossref] [PubMed]
- Malhotra NR, Piazza M, Demoor R, et al. Impact of Reduced Preincision Antibiotic Infusion Time on Surgical Site Infection Rates: A Retrospective Cohort Study. Ann Surg 2018. [Epub ahead of print]. [Crossref] [PubMed]
- Ljungqvist O, Scott M, Fearon KC. Enhanced Recovery After Surgery: A Review. JAMA Surg 2017;152:292-8. [Crossref] [PubMed]
- Ali ZS, Ma TS, Ozturk AK, et al. Pre-optimization of spinal surgery patients: Development of a neurosurgical enhanced recovery after surgery (ERAS) protocol. Clin Neurol Neurosurg 2018;164:142-53. [Crossref] [PubMed]
- Parrish AB, O'Neill SM, Crain SR, et al. An Enhanced Recovery After Surgery (ERAS) Protocol for Ambulatory Anorectal Surgery Reduced Postoperative Pain and Unplanned Returns to Care After Discharge. World J Surg 2018;42:1929-38. [Crossref] [PubMed]
- Sarin A, Litonius ES, Naidu R, et al. Successful implementation of an Enhanced Recovery After Surgery program shortens length of stay and improves postoperative pain, and bowel and bladder function after colorectal surgery. BMC Anesthesiol 2016;16:55. [Crossref] [PubMed]
- Rojas KE, Manasseh DM, Flom PL, et al. A pilot study of a breast surgery Enhanced Recovery After Surgery (ERAS) protocol to eliminate narcotic prescription at discharge. Breast Cancer Res Treat 2018;171:621-6. [Crossref] [PubMed]
- Shipton EA, Shipton EE, Shipton AJ. A Review of the Opioid Epidemic: What Do We Do About It? Pain Ther 2018;7:23-36. [Crossref] [PubMed]
- Göransson C, Eriksson I, Ziegert K, et al. Testing an app for reporting health concerns-Experiences from older people and home care nurses. Int J Older People Nurs 2018;13:e12181. [Crossref] [PubMed]
- Bakker D, Rickard N. Engagement in mobile phone app for self-monitoring of emotional wellbeing predicts changes in mental health: MoodPrism. J Affect Disord 2018;227:432-42. [Crossref] [PubMed]
- Fukuoka Y, Gay CL, Joiner KL, et al. A Novel Diabetes Prevention Intervention Using a Mobile App: A Randomized Controlled Trial With Overweight Adults at Risk. Am J Prev Med 2015;49:223-37. [Crossref] [PubMed]
- Wang QQ, Zhao J, Huo XR, et al. Effects of a home care mobile app on the outcomes of discharged patients with a stoma: a randomized controlled trial. J Clin Nurs 2018;27:3592-602. [Crossref] [PubMed]
- Floch J, Zettl A, Fricke L, et al. User Needs in the Development of a Health App Ecosystem for Self-Management of Cystic Fibrosis: User-Centered Development Approach. JMIR Mhealth Uhealth 2018;6:e113. [Crossref] [PubMed]
- Constantinescu G, Loewen I, King B, et al. Designing a Mobile Health App for Patients With Dysphagia Following Head and Neck Cancer: A Qualitative Study. JMIR Rehabil Assist Technol 2017;4:e3. [Crossref] [PubMed]
- Guo Y, Chen Y, Lane DA, et al. Mobile Health Technology for Atrial Fibrillation Management Integrating Decision Support, Education, and Patient Involvement: mAF App Trial. Am J Med 2017;130:1388-1396.e6. [Crossref] [PubMed]
- Kessel KA, Vogel MM, Kessel C, et al. Mobile Health in Oncology: A Patient Survey About App-Assisted Cancer Care. JMIR Mhealth Uhealth 2017;5:e81. [Crossref] [PubMed]
- Rodoni BM, Smith BW, Joseph JR, et al. Smartphone Use and Interest in a Spine Surgery Recovery Mobile Application Among Patients in a US Academic Neurosurgery Practice 2019. Oper Neurosurg (Hagerstown) 2019. [Epub ahead of print].
- Armstrong KA, Coyte PC, Brown M, et al. Effect of Home Monitoring via Mobile App on the Number of In-Person Visits Following Ambulatory Surgery: A Randomized Clinical Trial. JAMA Surg 2017;152:622-7. [Crossref] [PubMed]
Cite this article as: Glauser G, Ali ZS, Gardiner D, Ramayya AG, Pessoa R, Grady MS, Welch WC, Zager EL, Sim E, Haughey V, Wells B, Restuccia M, Tait G, Fala G, Malhotra NR. Assessing the utility of an IoS application in the perioperative care of spine surgery patients: the NeuroPath Pilot study. mHealth 2019;5:40.


