
African American women’s relationship with their mobile phone, and what they want in a mobile delivered physical activity intervention: guidance for intervention development
Introduction
Regular physical activity (PA) engagement, defined as 150 minutes per week of moderate-to-vigorous PA (MVPA), is central in both prevention and management of many chronic disease conditions, including type 2 diabetes and coronary heart disease (1). The most recent CDC report on PA patterns among American adults indicates that only 36% of African American (AA) women are meeting the recommended guidelines for regular PA (2). AA women are burdened by numerous chronic conditions (e.g., type 2 diabetes, obesity, and coronary heart disease) that can be prevented with a healthy lifestyle that includes regular PA (2-5). While numerous PA interventions with AA women have been developed, many are ineffective and/or unsustainable (6-11). Low level of participant engagement and low retention are common challenges in many of these studies (10,11). Intervention approaches that reduce participation burden and reach this group in their daily environment are likely to increase engagement and eventual behavior change (7,12,13).
Mobile phone technology, including text-messaging is part of the broader technological toolkit recommended by Healthy People 2020 to enhance behavioral health interventions intended to decrease risks for chronic disease conditions impacting the US population, and particularly those affecting disadvantaged groups (4). Mobile phone text messaging delivered interventions have shown promising results across a variety of health behaviors, including PA (14-16). The appeal of this technology is that it facilitates the development of scalable interventions that can be delivered in real time and reach people in their natural day-to-day environment (14,15). Moreover, text messaging requires minimal effort from the recipient other than opening the text message to engage with the intervention (16-18). Mobile phone text messaging has shown to be an effective modality to promote sustainability of various health behaviors, including PA (16-19). A meta-analysis of mobile phone text messaging delivered PA studies showed a mean effect for these interventions in the moderate range (g =0.54; 95% CI, 0.17 to 0.92, P=0.01) (20). A recent survey shows that AA women are among the largest consumers (92%) of this technology, thus providing researchers with an important opportunity to reach a large segment of this population and promote regular PA (21). Despite the prevalence of this technology among AA women, mobile phone interventions with this group are in a nascent stage. Three known pilot PA controlled trials utilizing text-messaging approaches have been conducted to date and, overall, they do show evidence of preliminary efficacy (22-24). However, their effects sizes are small, indicating the need for more research on mHealth strategies that effectively assess barriers and facilitators of PA in this group (22-24).
Data on how AA women use their phones as part of their daily routine may provide essential information about the mHealth components that are most relevant to help them adopt and maintain regular PA. There is research to indicate that an individual’s daily pattern of mobile use as well as how frequently they carry this device with them may impact their receptivity to, and engagement with, interventions delivered through the mobile phone (25,26). As mentioned, there is limited research on the nature of the relationship that AA women have with the mobile phone. Moreover, more research on the assessment of mobile text messaging as an acceptable medium to deliver health communication strategies is needed.
A recent study suggested that social demographics, such as age, education and employment status were associated with mobile phone use patterns among different racial, ethnic and gender subgroups (27). For example, individuals with higher levels of education and income tend to use this technology more commonly compared to individuals with less education and lower household incomes (28,29). Age differences in the usage of this technology show younger adults (e.g., aged 18–29) as having higher mobile phone use patterns than then their older counterparts (28,29). Furthermore, individuals who are single report using their phone more continuously throughout the day compared to married adults (30). It is unknown if these social demographic variables influence attitudes and cognitions related to mobile phone use among AA women.
In addition to quantitative assessment of the nature of the relationship that AA women have with their mobile phone, qualitative interviewing methods (31,32) may be particularly helpful in gathering in-depth assessments of AA women’s opinions and level of interest in participating in a PA intervention that is delivered through the mobile phone. Specifically, a standardized open-ended interview approach is recommended to explore stakeholders’ views of a proposed intervention, their suggestions for refining prescribed approaches, and to identify other important strategies that should be incorporated into the final program to increase behavior change (32-34). Accordingly, this methodological approach can also help determine the perceived importance of text messaging and other mobile phone applications among AA women, and how that can be leveraged to address their needs for PA.
This exploratory study uses both a self-report survey and a standardized open-ended qualitative interview to assess, respectively, mobile phone use patterns among AA women and their views of text messaging-based interventions as adequate in helping them acquire regular PA. Moreover, this study also examines whether mobile use patterns are associated with social demographic variables such as level of education, age, and marital status among AA women. The information obtained from this study could potentially inform the development of mHealth PA interventions tailored specifically for AA women.
Methods
Procedures
Recruitment was primarily from a national Listserv of predominantly AA members called BeautyLynk. The majority of participants (90%) reside in the New England area. BeautyLynk is an online beauty salon that provides hair and makeup services to members at their preferred locations (e.g., in their home). Members received an electronic copy of the study flyer from the owner of the Listserv that included the eligibility criteria for participation. Eligible individuals had to identify as AA, female and be aged 18 or older. Seventy individuals contacted the study staff via email or telephone over the course of two weeks. Eventually, 50 people completed a telephone screen that consisted of demographic questions about their race, age and gender to determine their eligibility to participate in the study. Eligible individuals received the study documents via post mail consisting of: two consent forms (a copy for participant to keep), demographic questionnaire, survey on mobile phone use pattern and an “availability form” for reporting the days and times they would be available to complete the single telephone interview. Participants also received a prepaid envelope to return the signed consent form, surveys, and the availability form. Forty-two participants completed the survey. After receiving the completed study documents, a research staff member contacted the participant to confirm the day and time of the single qualitative interview. Based on participants’ reports, the survey took an average of 20 minutes to complete. The interview ranged from 15 to 40 minutes. Participants received gift cards in the amount of $30 and $20, respectively, for completing the survey and the interview. Informed consent and other human subject protocols were approved by the Institutional Review Board at The Miriam Hospital.
Measures
Demographics
Participants provided demographic information about their race, gender, age, marital status, level of education, income and employment status.
Mobile Phone Affinity Scale (MPAS)
The MPAS is a psychometrically supported measure that consists of six constructs representing both positive and negative cognitions and behaviors related to mobile phone use (25,26). The three positive subscales are Connectedness, Productivity and Empowerment/Safety, and respectively, they measure individuals’ use of this technology to: (I) remain connected with friends and family (e.g., “My phone helps me stay close to family and friends”); (II) organize work/school schedule and/or related tasks (e.g., “My phone helps me stay up-to-date with work/school activities”); and (III) the ability to access help when in an unsafe situation (e.g., “Having my phone with me makes it easier to leave a risky situation”) (25).
The subscales that assess negative constructs related to mobile phone use are Anxious Attachment (e.g., “I feel anxious if I don’t have my phone with me”), Addiction (e.g., “I find myself occupied on my phone even when I’m with other people”) and Continuous Use (e.g., “I use my phone all day”). Participants reported how true each statement was for them using a 5-point Likert-type scale, ranging from 1= “not all true” to 5= “extremely true” (11). Psychometric evaluations of the MPAS shows each subscale to have very good internal consistency reliability, with a Cronbach’s alpha range of 0.76–0.88 (25). High level of endorsement of the MPAS constructs can be used as a proxy measure for estimating a high likelihood that individuals will be receptive to a mobile phone delivered intervention (mHealth) (25,26,35). Moreover, information from these subscales could inform various intervention components that may increase behavior change for the particular group (25,35).
Qualitative interview approach
A standardized open-ended interview approach was used to explore AA women’s views of mobile phone text messaging as a potentially viable platform to deliver health communication messages and adopt and maintain regular PA. This methodological approach of qualitative interviewing is recommended for conducting formative research; it facilitates the nuanced assessment of participants’ feelings and opinions toward the particular intervention approach as acceptable or unacceptable by the target group (31,32). Each participant was asked the following question: “What do you think about a program that is developed to help you start and maintain regular physical activity that is delivered through your mobile phone in the form of daily short text motivational messages?”. The following probes were used as appropriate to facilitate deeper insight of participants’ responses: (I) “tell me how this program would meet or not meet your needs in helping to become physically active,” and/or (II) “what other things would make this type of physical activity program interesting to you?”. Twenty participants out of the total sample (N=42) completed the interview.
Qualitative paradigm
A pragmatic foundation paradigm (34,36) was used to explore participants’ responses to how text messaging is adequate to help become physically active. From a formative research perspective, this paradigm facilitates a deeper assessment of AA women’s needs for PA as well as the relevance of text messaging approaches to promote behavior change. According to Johnson and Onwegbuzie (36), this approach facilitates the collection of data that will provide a clear foundation on how intervention approaches should be developed and/or refined to adequately address the needs of the individuals as well as the overall group.
Qualitative analytic approach
The research team developed the preliminary coding scheme based on the research question of whether AA women view text messaging technology to be an acceptable and attractive platform to enhance intervention approaches to PA promotion. The final code model was completed over the course of several meetings. A double coding approach (37) was used for analysis. Two research team members independently reviewed and coded all of the transcripts; the passages coded were compared, discrepancies were noted, and a consensus on the appropriate coding for both transcripts was reached. The Nvivo 10 software was used to complete the analysis (38).
Quantitative analyses
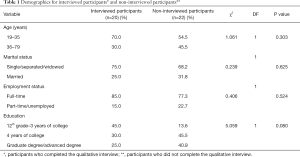
Characteristic differences for interview completers and interview non-completers
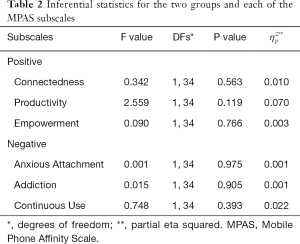
Chi square analyses were conducted and assessed proportional differences for demographic variables age, education, employment and marital status between the sample of participants who completed (interview completers, n=20) and did not complete the qualitative interview (interview non-completers, n=22). There were no significant differences in proportion for these four demographics between the groups (P>0.05). Detailed results are provided in Table 1. Income was not added to the model since only 24 participants (overall equal numbers from both groups) did not report their household income. Moreover, multivariate analyses were used to explore mean differences between two groups for each of the six MPAS subspaces. No statistically significant differences were noted (P>0.05). Detailed results are provided in Table 2.
Full table
Full table
Demographic results for total sample
Frequency statistics were used to explore the distribution of the sample (N=42; mean age =35, SD =10.25). Detailed demographics are found in Table 1. The age variable was coded into two groups, ages 19–35 (n=27; 65.85%) and ages 36–79 (n=14; 34.15%). The age range for participants was 19 to 79 years old. Participants’ responses for the education variable were coded into three groups: 12th grade–3 years of college (n=8; 19%), bachelor’s degree (n=16; 38.1%), and graduate or advanced degree (n=18; 42.9%). The marital status variable was divided in two groups, “single/divorced/widowed” (n=30; 71.43%) and “married” (n=12; 28.57%). The majority of the participants were employed full-time (n=35; 83.33%). Income was obtained for 24 participants of the total sample (N=42), with the median annual income being $48,000. Lastly, the majority of participants (n=39; 93%) were not meeting recommendation guidelines of 150 minutes of moderate-to-vigorous level of PA per week (1). Initial mean results showed somewhat higher mean scores for the positive subscales, Connectedness (mean =13.29; SD =4.49), Productivity (mean =14.00, SD =3.75), Empowerment/Safety (mean =12.00, SD =4.75) in comparison to the negative subscales, Anxious Attachment (mean = 10.69; SD =4.67), Addiction (mean =11.26; SD =4.06), and Continuous Use (mean =11.29; SD =4.86).
Demographic differences in the MPAS
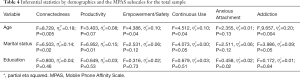
Analysis of variance tests (ANOVAs) were conducted to determine potential demographic differences of age, education, and marital status on AA women’s relationship with the mobile phone, as measured by the MPAS subscales.
Age
A statistically significant difference was noted between the two age groups (ages 19–35 vs. ages 36–79) for four of the MPAS subscales: Connectedness (F1, 40=8.729, partial eta square ( ) =0.18; P=0.005), Empowerment/Safety (F1, 39=4.386,
) =0.18; P=0.005), Empowerment/Safety (F1, 39=4.386,  =0.10; P=0.04), Continuous Use (F1, 39=4.512,
=0.10; P=0.04), Continuous Use (F1, 39=4.512,  =0.10; P=0.04), and Addiction (F1, 39=9.657,
=0.10; P=0.04), and Addiction (F1, 39=9.657,  =0.20; P=0.004). The group aged 19–35 years old had higher mean scores on all four measures compared to their older counterparts. See Table 3.
=0.20; P=0.004). The group aged 19–35 years old had higher mean scores on all four measures compared to their older counterparts. See Table 3.

Full table
Marital status
A statistically significant difference for marital status was observed for the Connectedness (F1, 41=6.503,  =0.14; P=0.02) and Productivity (F1, 41=6.952,
=0.14; P=0.02) and Productivity (F1, 41=6.952,  =0.15; P=0.01) subscales. Participants who were single reported higher mean scores on these measures than married participants. A trend toward significance was also noted for Addiction (F1, 40=3.986,
=0.15; P=0.01) subscales. Participants who were single reported higher mean scores on these measures than married participants. A trend toward significance was also noted for Addiction (F1, 40=3.986,  =0.09; P=0.05) and Continuous Use (F1, 40=4.073,
=0.09; P=0.05) and Continuous Use (F1, 40=4.073,  =0.09; P=0.05). The single group had higher scores, on average, on these subscales than their married counterparts. Statistically significant differences were not found between married and single women on the Empowerment/Safety or Anxious Attachment subscales (P>0.05) (Table 4).
=0.09; P=0.05). The single group had higher scores, on average, on these subscales than their married counterparts. Statistically significant differences were not found between married and single women on the Empowerment/Safety or Anxious Attachment subscales (P>0.05) (Table 4).
Full table
Education
There was no statistically significant difference for the three education groups and the six MPAS subscales (P>0.05). Detailed results are provided in Table 3. All analyses were performed using statistical package for the Social Sciences (SPSS; IBM Corp) (39).
Results
The study results were determined by analyzing verbatim responses of participants. The research question was whether mobile phone text messaging technology is a viable platform in PA promotion among AA women. Responses were organized into three primary categories or nodes: (I) acceptability of a text messaging-based PA intervention; (II) limitation of the text messaging-based approach; and (III) suggestions for increasing the appeal of mHealth PA approaches.
Acceptability of a text messaging-based PA intervention
Nineteen of the 20 participants (95%) who completed the interview mentioned they would participate in a text messaging delivered PA program. Thirteen participants described this potential text messaging delivered PA program as potentially “convenient,” “motivating” and “beneficial.” Moreover, five participants noted that daily motivational messages would serve as a “remind[er]” to exercise. Two of those response exemplars are:
“I think it would be beneficial. It sounds like sort of like a coaching type of thing where you meet—well, you check in with a coach every day, and they help keep you motivated and help keep you sticking to your goals. Yeah, I definitely think that’s a great source of motivation” (ID: 1010).
“It would be interesting to me, cuz it’ll keep me—I’ll be expecting it, or if I’m not expecting it, I forget about it. I get that message. It’ll remind me that I have something else to do. That is something that will benefit me” (ID: 1022).
Only one participant mentioned that she would not be interested in a text messaging-based PA intervention. She stated the following reason:
“I don’t think it would meet my needs. I’m not a big telephone person. I try to use it as sparing as I can.” (ID: 1031).
Limitations of a text messaging-based approach
Nine of the nineteen participants (47.4%) who said they would be interested in participating in a text messaging PA intervention also expressed some concerns about the limitation of daily short text messages alone to increase their level of motivation to maintain regular PA over time. One of the participants suggests that encouraging reminder text-messages would be helpful:
“I don’t know, just like a message that is a recorded message, and it’s sent to your phone and you can play it like hey you’re doing great… continue on. You did this much movement, and you need to do this much more, or you’re—whatever percent. I’m closer to reaching my goal, something like that” (ID: 1016).
Other participants identified the lack of accountability inherent in an intervention solely based on mobile phone text messaging applications as a limitation. As one person explains, “I guess a text message could be ignored, right? Who’s gonna hold me accountable really?” (ID: 1028).
“I would say cons would be it’s just suggestions, and there’s not really a way to track my progress” (ID: 1019).
Other participant concerns included the ability of researchers to personalize intervention messages to increase appeal. Two of those responses were:
“My only thing would be, maybe, making it personal, as opposed to, if I feel I’m getting mass texts or emails, it might not be as impactful” (ID: 1025).
“I think that initial part of it would really have to feel custom[ized]. I know the programs that are out there, they say they’ll make a customized thing, but you’re really taking from a template of ten different things that are out there” (ID: 1011).
Increasing appeal of mHealth approaches
Thirteen participants (68%) provided suggestions on ways to modify mobile phone technology to enhance PA intervention approaches to meet their needs:
“[with text message]… there’s not really a way to track my progress. Okay, I look at it, but if there was something for me to press and it’s like, start work-out, I feel like that holds me more accountable than, okay, I just look at it and not do anything” (ID: 1029).
“In an app format, I think it would be easier, because then it’s something that pops up on my phone. It’d be great if it had a little message that was like, for example, “Today is 60 degrees. Why don’t you walk? Great day to walk to work,” or something like that” (ID: 1014).
“Along with the text message, I’d probably need something visual. [Also] Give me some health—I have to be scared straight all over” (ID: 1018).
Additionally, six participants (32%) provided suggestions that indicate that interacting with the researcher to set exercise goals as well as having a social support component would increase their motivation for PA.
“… it’s hard to really know why you’re doing it or why you’re not doing it. Be able to sit down with someone who’s spending their—that’s their job, to help me understand how I can better exercise, would be—it’d be helpful” (ID: 1025).
“It’s a support sys—built-in support system… It will be a great motivating factor because it’s something that I know daily basis I would get some type of support for me to stay on this—on routine. ‘Cause history has shown that I can’t do it by myself” (ID: 1046).
“… maybe having somebody to check in with or somebody to talk to if you felt like things were overwhelming or, “Hey, I don’t feel like working out today,” or, “Hey, my schedule just changed. I don’t know how to fit some quick exercises” (ID: 1011).
Overall, participants mentioned interest in a text messaging-based PA intervention. Additionally, they provided suggestions, including an app delivery format and meeting with the study interventionist at some point during the intervention to increase appeal.
Discussion
This study assessed AA women’s relationships with their mobile phones as well as their views of text messaging as an important platform through which to deliver health communication and promote regular PA. Thus, the overarching goal of this study is to extend current understanding of the intervention components that should be considered when developing a mobile phone delivered PA intervention (mHealth PA) that appeals to the needs of AA women. As previously mentioned, information on individuals’ mobile phone use patterns may provide insights into particular mHealth intervention components that may best appeal to the particular target group.
Our study results indicate that AA women use their phone daily to connect with family members and friends. These patterns of mobile phone use suggest that mHealth strategies that allow AA women to connect and socialize with one another for peer social support may increase motivation for PA engagement. Essentially, this approach would address some concerns among AA women regarding text messaging-based interventions being potentially insufficient in helping them to be “accountable” for their PA behaviors. Group social support has shown to be efficacious in promoting adherence to PA goals (40,41). According to Zhang and colleagues (41), the group dynamic not only allows members to encourage each other but also supports the development of “friendly competition” that serves as further motivation for achieving set goals for PA or, in some situations, even to surpass them. In a mHealth PA intervention, peer-to-peer social support could be achieved through an asynchronous chatroom where participants can talk with one another wherever they are and share strategies for overcoming barriers throughout the intervention. This approach is particularly important in interventions with AA women, given that this group often lacks physically active examples (1-3) and may feel alone in changing their behavior.
Moreover, AA women indicated that they use their phone to organize and complete various daily activities or tasks. Accordingly, intervention approaches which leverage mobile phone applications or apps that allow them to set daily goals for PA and to monitor their level of PA could be appealing. In fact, behavioral monitoring has shown to be difficult to maintain, particularly in the early stages of behavior change (42,43). Moreover, behavioral monitoring through the traditional mean of logging daily steps using paper and pencil is impractical to maintain over time (42). Our study results also show that AA women viewed their phone as a tool of empowerment and safety. In the context of health promotion, the more an individual feels empowered, the higher their priority for self-care, which may include the adoption of a healthy lifestyle. Thus, mHealth approaches that provide tailored feedback to AA women based on their level of PA and sedentariness, and are delivered in real time may empower them to engage in PA or increase their level of self-efficacy. An intervention message, for example, that encourages a participant to persist on reaching their goal for PA (e.g., “you are only 500 steps away from achieving your goal for the day”) might be viewed as empowering. The qualitative data obtained in this study provide further support for the aforementioned approach as potentially beneficial among AA women (e.g., “I think it would come to my attention and I would stick with it,” ID: 1028). Moreover, consistent with this construct, intervention approaches that provide AA women who report neighborhood safety concerns with intervention approaches that provide alternative safe options for exercise (e.g., information of safe walking and running trails near their work or their home available on their mobile devices) may promote engagement.
Our data also indicate that younger participants (ages 19–35) were more likely to report using their phone to connect with friends and family and viewed their phone as a source of empowerment compared to older participants (aged 36 and older). The effect size values for these models were in the large (=0.20) or medium (=0.10) Cohen d taxonomy for partial eta square indices (44,45), suggesting a strong association between age and the MPAS subscales. Accordingly, these results suggest that attention to age is important when developing mHealth strategies that allow AA women to connect with another for social support for PA and empowering them to engage in this behavior. Younger individuals also reported using this device continuously throughout their day, which is suggestive of an addictive relationship with this device. These results are consistent with previous research that show that younger adults tend to report a higher level of dependence on their phone to complete many tasks as well as spending a significant amount of time exploring various applications or apps (46,47). A small effect size was noted between the two variables. Nevertheless, several studies have shown evidence of excessive or abnormal mobile phone use behaviors among younger adults as well as their impact on health and mental health (45,48). The consideration for mHealth PA intervention with this group is twofold: while AA women aged 19–35 are likely to be even more receptive to mHealth approaches, their tendency to use this phone continuously throughout the day and their addictive relationship with this device suggest a lack of attention to other aspects of their life, potentially engagement in healthy behaviors. In addition, they may have so many other distractions on their phone that the intervention messages about PA might be diluted by the relative noise, or ignored in favor of other phone-based activities. Thus, intervention approaches that teach them the skills to prioritize PA into their daily routine are especially appropriate for this group.
Moreover, marital status differences showed that single participants were higher on the Connectedness and Productivity subscales. A large effect size value (e.g.,  =0.15) was noted between this independent variable and each of the two MPAS subscales, indicating that relationship status influences the nature of the relationship that AA women have with their mobile phone based on these constructs. From an intervention development standpoint, our findings indicate that single individuals have greater interest in participating in a PA intervention that incorporates the involvement of a close friend or family member for social support. Moreover, single AA women might be particularly interested in mHealth approaches that allow them to set daily goals and monitor their PA behaviors. Somewhat paradoxically, their continuous use of this device throughout the day indicates a potential barrier to intervention engagement and efficacy of mHealth approaches (26,45). Nonetheless, despite this limitation, intervention messages that serve as prompts or reminders for PA engagement would likely benefit this group.
=0.15) was noted between this independent variable and each of the two MPAS subscales, indicating that relationship status influences the nature of the relationship that AA women have with their mobile phone based on these constructs. From an intervention development standpoint, our findings indicate that single individuals have greater interest in participating in a PA intervention that incorporates the involvement of a close friend or family member for social support. Moreover, single AA women might be particularly interested in mHealth approaches that allow them to set daily goals and monitor their PA behaviors. Somewhat paradoxically, their continuous use of this device throughout the day indicates a potential barrier to intervention engagement and efficacy of mHealth approaches (26,45). Nonetheless, despite this limitation, intervention messages that serve as prompts or reminders for PA engagement would likely benefit this group.
Strengths, limitations and future research
Despite the many strengths of the current study, there are limitations that should be noted. First, we did not assess whether the nature of the relationship that AA women have with their mobile phone influenced their level of engagement in a mHealth PA intervention. As a result, this study does not determine whether the nature of the relationship that individuals have with their mobile phones was predictive of their level of engagement with a mHealth PA intervention or its efficacy. Randomized mHealth PA clinical trials are encouraged to assess mobile phone use patterns and outcomes. Another limitation is that demographic comparisons were limited to two subgroups with respect to age and marital status, and three sub-groups for education. A larger sample of AA women is needed for various age, marital status and education subgroup comparisons. Moreover, because of the small sample size of this study, future research with large samples of AA women should further assess the level of the associations or practical significance between age and marital status and the relevant MPAS subscales. Lastly, there are some limitations to qualitative analyses more generally, as they are subjective. The researchers of this study have extensive qualitative experience and several recommended strategies to ensure that a rigorous standard of qualitative collection, analyses and interpretations were applied.
To our knowledge, this is the first study to assess AA women’s relationships with their mobile phones and as well as their views of mobile phone text messaging as a potentially promising platform to enhance health communication for PA promotion. This information fills a knowledge gap in terms of AA women’s relationship with their mobile phone and provides substantial guidance in mobile phone technology applications that will likely be beneficial in helping AA women to become and remain physically active.
Acknowledgments
Funding: Research reported in this paper was supported by the National Heart, Lung and Blood Institute (award number T32 5T32HL076134-10). While completing this paper, Dr. Sillice was supported by the Minority Supplement awarded from the National Heart, Lung and Blood Institute and the National Institutes of Health (award number 3R01HL127695). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: This study was approved by the Institutional Review Board at The Miriam Hospital (No. 857242-12). Written informed consent was obtained from from all participants.
References
- U.S. Department of Health and Human Services. Physical Activity Guidelines for Americans, 2nd edition. Washington, DC: U.S. Department of Health and Human Services, 2018.
- Benjamin EJ, Virani SS, Callaway CW, et al. Heart Disease and Stroke Statistics-2018 Update: A Report From the American Heart Association. Circulation 2018;137:e67-492. [Crossref] [PubMed]
- Mozaffarian D, Benjamin EJ, Go AS, et al. Heart disease and stroke statistics—2015 update: a report from the American Heart Association. Circulation. 2015;131:e29-322. [PubMed]
- Healthy People 2020 Nutrition, Physical Activity, and Obesity Overview & Impact. (accessed on April 29 2018). Available online: http://www.healthypeople.gov/2020/leading-health-indicators/2020-lhi-topics/Nutrition-Physical-Activity-and-Obesity
- Go AS, Mozaffarian D, Roger VL, et al. Heart disease and stroke statistics 2014 update: A report from the American Heart Association. Circulation 2014;129:e28-292. [PubMed]
- Whitt-Glover MC, Keith NR, Ceaser TG, et al. A systematic review of physical activity interventions among African American adults: evidence from 2009 to 2013. Obes Rev 2014;15:125-45. [Crossref] [PubMed]
- Whitt-Glover MC, Crespo CJ, Joe J. Recommendations for advancing opportunities to increase physical activity in racial/ethnic minority communities. Prev Med 2009;49:292-3. [Crossref] [PubMed]
- Banks-Wallace J, Conn V. Interventions to promote physical activity among African American women. Public Health Nurs 2002;19:321-35. [Crossref] [PubMed]
- Yanek LR, Becker DM, Moy TF, et al. Project Joy: faith based cardiovascular health promotion for African American women. Public Health Rep 2001;116:68-81. [Crossref] [PubMed]
- Young DR, Stewart KJ. A church-based physical activity intervention for African American women. Fam Community Health 2006;29:103-17. [Crossref] [PubMed]
- Parra-Medina D, Wilcox S, Salinas J, et al. Results of the heart healthy and ethnically relevant lifestyle trial: a cardiovascular risk reduction intervention for African American women attending community health centers. Am J Public Health 2011;101:1914-21. [Crossref] [PubMed]
- Buchholz SW, Willbur J, Schoeny ME, et al. Retention of African American women in a Lifestyle physical activity program. West J Nurs Res 2016;38:369-85. [Crossref] [PubMed]
- Thomas S, Yingling L, Adu-Brimpong J, et al. Mobile Health Technology Can Objectively Capture Physical Activity (PA) Targets Among African-American Women Within Resource-Limited Communities-the Washington, D.C. Cardiovascular Health and Needs Assessment. J Racial Ethn Health Disparities 2016. [Crossref] [PubMed]
- Gurman TA, Rubin SE, Roess AA. Effectiveness of mHealth behavior change interventions in developing countries; A systematic review of the literature. J Health Commun 2012;17:82-104. [Crossref] [PubMed]
- Siopis G, Chey T, Allman-Farinelli M. A systematic review and meta-analysis of interventions for weight management using text messaging. J Hum Nutr Diet 2015;28:1-15. [Crossref] [PubMed]
- Head KJ, Noar SM, Iannarino NT, Grant Harrington N. Efficacy of text messaging-based interventions for health promotion: A meta-analysis. Soc Sci Med 2013;97:41-8. [Crossref] [PubMed]
- Bock B, Heron KE, Jennings E, et al. A Text Message Delivered Smoking Cessation Intervention: The Initial Trial of TXT-2-Quit: Randomized Controlled Trial. JMIR Mhealth Uhealth 2013;1:e17. [Crossref] [PubMed]
- Fjeldsoe BS. Behavior change interventions delivered by mobile telephone short-message service. Am J Prev Med 2009;36:165-73. [Crossref] [PubMed]
- Bort-Roig J, Gilson ND, Puig-Ribera A, Contreras RS, Trost SG. Measuring and influencing physical activity with smartphone technology: a systematic review. Sports Med 2014;44:671-86. [Crossref] [PubMed]
- Holtz B, Lauckner C. Diabetes management via mobile phones: a systematic review. Telemed J E Health 2012;18:175-84. [Crossref] [PubMed]
- Smith A. African Americans and technology use. A demographic portrait. Available online: http://pewinternet.org/Reports/2014/African-American-Tech-Use.aspx
- Joseph RP, Keller C, Adams MA, et al. Print versus a culturally-relevant Facebook and text message delivered intervention to promote physical activity in African American women: a randomized pilot trial. BMC Womens Health 2015;15:30. [Crossref] [PubMed]
- Gerber BS, Stolley MR, Thompson AL, et al. Mobile phone text messaging to promote healthy behaviors and weight loss maintenance: a feasibility study. Health Informatics J 2009;15:17-25. [Crossref] [PubMed]
- Kim BH, Glanz K. Text messaging to motivate walking in older African Americans: a randomized controlled trial. Am J Prev Med 2013;44:71-5. [Crossref] [PubMed]
- Bock BC, Lantini R, Thind H, et al. The Mobile Phone Affinity Scale: Enhancement and Refinement. JMIR Mhealth Uhealth 2016;4:e134. [Crossref] [PubMed]
- Sillice MA, Dunsiger S, Jennings E, et al. Differences in mobile phone affinity between demographic groups: implications for mobile phone delivered interventions and programs. mHealth 2018;4:39. [Crossref] [PubMed]
- Who is Smartphone Dependent. (Accessed 2018 March 1). Available online: http://www.pewinternet.org/fact-sheet/mobile/
- Duggan M. Cell Phone Activities 2013. Washington, DC: Pew Research Center Internet & American Life Project; 2013 (Accessed 2018 May 14). Available online: http://pewinternet.org/Reports/2013/Cell-Activities.asp
- U.S. Smartphone Use in. 2015. Available online: https://www.pewresearch.org/fact-tank/2015/04/01/6-facts-about-americans-and-their-smartphones/
- McDaniel BT, Coyne SM. “Technoference”: The interference of technology in couple relationships and implications for women’s personal and relational well-being. Psychol Pop Media Cult 2016;5:85-98. [Crossref]
- Green J, Thorogood N. Qualitative methods for health research. Sage Publications Ltd, 2013.
- Rosen RK, Kuo C, Gobin R, et al. How qualitative methods contribute to intervention adaptation: An HIV risk reduction example. Qual Psychol 2018;5:2-15. [Crossref]
- Kreuter MW, Haughton LT. Integrating culture into health information for African American women. Am Behav Sci 2006;49:794-810. [Crossref]
- Guest G, MacQueen KM, Namey EE. Applied thematic analysis. Thousand Oaks, CA: Sage Publication Inc., 2011.
- Bock BC, Thind H, Fava JL, et al. Development of the Mobile Phone Attachment Scale. Proc Annu Hawaii Int Conf Syst Sci 2016;2016:3401-7.
- Johnson RB, Onwegbuzie AJ. Mixed methods research: A research paradigm whose time has come. Edu Res 2004;3:14-26. [Crossref]
- Bazeley P, Jackson K. Qualitative analysis with Nvivo, 2nd. edition. Thousand Oaks, CA: Sage Publications Inc., 2013.
- NVivo Qualitative Data Analysis Software. QSR International Pty Ltd., 2013.
- IBM Corp. Released 2016. IBM SPSS Statistics for Windows, Version 24.0. Armonk, NY: IBM Corp.
- Foster D, Linenhan C, Kirman B, et al. Motivating physical activity at work: Using persuasive social media for competitive step counting. ACM Press, 2010:111-6.
- Zhang J, Brackbill D, Yang S, et al. Support or competition? How online social networks increase physical activity: A randomized controlled trial Prev Med Rep 2016;4:453-8. [Crossref] [PubMed]
- Kirwan M, Duncan MJ, Vandelanotte C, et al. Using smartphone technology to monitor physical activity in the 10,000 Steps Program: A Matched Case–Control Trial. J Med Internet Res 2012;14:e55. [Crossref] [PubMed]
- Yan AF, Voorhees CC, Beck KH, et al. A social ecological assessment of physical activity among urban adolescents. Am J Health Behav 2014;38:379-91. [Crossref] [PubMed]
- Masahiro T, Monden K, Kubo K, et al. Mobile phone dependence and health-related lifestyle of University students. Social Behavior and Personality 2016;34:1277-84.
- Acharya JP, Acharya I, Waghrey D. A Study on some of the common health effects of cell-phones amongst college students. J Community Med Health Educ 2013;3:214. [Crossref]
- Cohen J. Statistical Power Analysis for the Behavioral Sciences, 2nd edition. Hillsdale, New Jersey: Lawrence Erlbaum Associates, 1988.
- Cohen J. Quantitative method in psychology: A power primer. Psycholog Bull 1992;112:155-9. [Crossref]
- Kuss DJ, Griffiths MD. OOnline social networking and addiction--a review of the psychological literature. Int J Environ Res Public Health 2011;8:3528-52. [Crossref] [PubMed]
Cite this article as: Sillice MA, Jennings E, Uebelacker LA, Abrantes AM, Holland CC, O’Keeffe B, Bock BC. African American women’s relationship with their mobile phone, and what they want in a mobile delivered physical activity intervention: guidance for intervention development. mHealth 2019;5:18.


