Operating room turnover time autocorrelation while using mobile applications
We would like to thank Drs. Dexter and Epstein for their well thought-out comments to our recent article about the use of an Android app to record the OR turnover times. In their letter, they raised several important questions and asked for clarifications which we now provide. At the time we performed our experiments, Greenville Memorial Hospital did not have sensor data to track OR turnover times. This is still the case as of today. The response to the inquiry related to turnover time autocorrelation is provided in the following.
Mobile applications can improve the performance of operating room turnover (1,2) as well as perioperative services (3). These applications serve as both visual management tools and data collection tools. Uddin et al. (1) found that a higher percentage of cases met their target turnover time when the mobile app (ORTimer) was used. Uddin et al. (2) reported that cases that used the ORTimer app had a lower turnover time compared to those cases that did not use the ORTimer app. In the aforementioned two studies, hypothesis testing was performed to test whether there is any difference between the turnover time when a mobile application was used and when it was not used. The hypothesis testing performed assumed that the turnover times are independent and identically distributed (iid).
As indicated by Dexter and Epstein (4), the iid assumption for turnover times could be unreliable due to the presence of autocorrelation (5-7). Dexter et al. (5) found that there was significant positive autocorrelation from one turnover time to the next and from one daily turnover time average to the next daily average. When averaged over a month, there was no autocorrelation in turnover times (5). Austin et al. (6) reported a similar finding; that is, there was significant positive autocorrelation from one turnover time to the next. Again, when the turnover times are averaged over a month, there was no autocorrelation (6).
As suggested by Dexter and Epstein (4), a runs test can be used to determine whether autocorrelation is present in turnover times. We performed the Wald-Wolfowitz runs test for all four groups analyzed in Uddin et al. (1): GI-Lab ORTimer, GI-Lab No ORTimer, D-Core ORTimer, and D-Core No ORTimer. The test results indicate that there is significant autocorrelation from one turnover time to the next for GI-Lab ORTimer (P value <0.001) and GI-Lab No ORTimer (P value =0.044) groups. However, there was no autocorrelation in turnover times for the D-Core ORTimer (P value =0.792) and D-Core No ORTimer (P value =0.411) groups. Following the same procedure used by Dexter et al. (5), we then calculated the average turnover time for each workday for both GI-Lab groups. We then performed a runs test using the daily average. We found that there was no autocorrelation in turnover times for both GI-Lab ORTimer (P value =0.359) and GI-Lab No ORTimer (P value =0.470) groups.
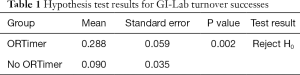
Given that there is significant autocorrelation in turnover times for GI-Lab ORTimer and GI-Lab No ORTimer, the results from the hypothesis test need to be updated. These updated test results are presented in Table 1. The null hypothesis (H0) in Table 1 is that there is no difference between the two turnover groups and the alternative hypothesis (H1) is that the “GI-Lab ORTimer” turnover success rate is greater than that of “GI-Lab No ORTimer.” As stated in Uddin et al. (1), a turnover is successful if the actual time taken was less than or equal to the allotted turnover time. As shown in Table 1, the means of success rates for both GI-Lab ORTimer and GI-Lab No ORTimer groups are lower than stated in Uddin et al. (1): 0.288 vs. 0.380 and 0.090 vs. 0.278, respectively, and the standard error for both groups are higher: 0.059 vs. 0.019 and 0.035 vs. 0.013, respectively. The proportionality test yields a P value of 0.002. Thus, the null hypothesis can be rejected at the 95% confidence level. Therefore, we can conclude that the use of the ORTimer app was effective in improving OR turnover time.
Full table
In summary, autocorrelation was present in GI-Lab but not in D-Core. The autocorrelation in GI-Lab did affect the success rate. However, when the turnover times are averaged for a day, week, or month, no autocorrelation was found (5,6). The findings reported in (1,2) remain true; that is, there is a significant improvement in turnover time success rate when the ORTimer app was used.
Acknowledgements
The authors would like to acknowledge the Perioperative Services Department at Greenville Health System for their continued support of the research. In addition, the authors appreciate the time and energy spent by participating CRNA staff (D-Core) and nursing staff (Memorial Medical Office Building GI-Lab) during the research period.
Funding: Research reported in this manuscript was supported by the National Science Foundation under grant IIS-1237080.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Disclaimer: The authors are solely responsible for the content and views expressed in this manuscript.
References
- Uddin M, Allen R, Huynh N, et al. Assessing operating room turnover time via the use of mobile application. Mhealth 2018;4:12. [Crossref] [PubMed]
- Uddin M, Allen R, Huynh N, et al. Effectiveness of a countdown timer in reducing OR turnover time. J Mob Technol Med 2017;6:25-33. [Crossref]
- Uddin MM, Huynh N, Vidal JM, et al. Evaluation of Google’s voice recognition and sentence classification for health care applications. Eng Manag J 2015;27:152-62. [Crossref]
- Dexter F, Epstein RH. Treating surgical turnover times as statistically independent events when testing interventions and mobile applications. Mhealth 2018;4:23. [Crossref] [PubMed]
- Dexter F, Epstein RH, Marcon E, et al. Estimating the incidence of prolonged turnover times and delays by time of day. Anesthesiology 2005;102:1242-8; discussion 6A.
- Austin TM, Lam HV, Shin NS, et al. Elective change of surgeon during the OR day has an operationally negligible impact on turnover time. J Clin Anesth 2014;26:343-9. [Crossref] [PubMed]
- Dexter F. High-quality operating room management research. J Clin Anesth 2014;26:341-2. [Crossref] [PubMed]
Cite this article as: Uddin M, Allen R, Huynh N, Vidal JM, Taaffe KM, Fredendall LD, Greenstein JS. Operating room turnover time autocorrelation while using mobile applications. mHealth 2018;4:38.


