Preconceptional health behavior change in women with overweight and obesity: prototype for SMART strong healthy women intervention
Introduction
Over 50% of pregnancies in the United States are affected by obesity and its comorbidities (1-3). The average maternal weight entering into a first pregnancy has increased over 20% in the past three decades, with at least 25% of women weighing 200 pounds or more at the time of the first prenatal visit (4). Maternal obesity is associated with many complications including hypertensive disorders of pregnancy, gestational diabetes mellitus, sleep apnea, labor and delivery issues, birth complications, fetal macrosomia, and the development of childhood obesity in offspring (1-5). Given that obesity is a major public health concern, effective and acceptable efforts for improving overweight and obesity outcomes in the context of pregnancy are needed. Some obesity prevention advocates have argued that early intervention during the prenatal period (i.e., the period after conception and before birth) is warranted because mothers are particularly focused on their and their baby’s health (6,7). Others suggest that the preconceptional period (i.e., the time before conception) is the optimal time in women’s lives to focus on making health improvements (e.g., losing weight) because they are not yet experiencing the unique barriers of pregnancy and the early infancy periods (i.e., women are better equipped to make behavioral changes as they have fewer barriers, can focus more on personal needs, and likely have more available time to dedicate to change) (8,9).
One study that targeted multiple preconceptional risk factors, Strong Healthy Women (SHW), was delivered to 692 pre- and interconceptional women across 12 weeks via six face-to-face sessions (10,11). The sessions were held at community locations in low income and rural communities via a partnership with Family Health Council of Central Pennsylvania. The intervention group (compared to controls) had better pre-post intervention outcomes related to nutrition, physical activity, and stress management (11). At the 12-month follow-up, the intervention group had reduced weight (mean group difference of 4.33 pounds) and body mass index (BMI; mean difference of 0.75). Among the 45 women that became pregnant during the 12-month follow-up period, the intervention group had significantly lower gestational weight gain than controls (mean difference of 17.95 pounds) (12). SHW’s promising results for improving pre- and interconceptional weight gain make it a valuable program for promoting women’s health before and between pregnancies, however, the SHW study team and community implementers noted that delivering all of the intervention components, activities, and content in face-to-face sessions was resource-intensive and expensive, and the time investment required for participation was burdensome for some women (11).
Exploring strategies to improve delivery of the SHW program, particularly among women with overweight and obesity, may enhance effectiveness for improving health before pregnancy. The goal of the present study was to revise SHW into SMART SHW, a version of the intervention that can be delivered to women via methods that will: (I) increase reach and delivery; (II) limit face-to-face session costs and resources; and (III) maintain participant acceptability of the intervention through decreasing participation burden (e.g., in-person time commitment). One strategy is to use mobile health (i.e., mHealth) technology to deliver some of the intervention content. Smartphones provide a unique platform for delivering health behavior change programs (13-15). Due to their increased adoption and availability in recent years, integrating smartphones into behavioral interventions to improve delivery has received increased attention because these devices can provide a multifaceted platform to present information and produce immediate feedback [e.g., via mobile web, online videos, text messaging, applications (i.e., apps)] (16).
There is precedent for using mobile technology, such as smartphones, to deliver mHealth interventions in the context of pregnancy (17). However, research harnessing smartphones to improve women’s pre- and interconceptional health outcomes specifically is limited. Only one intervention (‘Smarter Pregnancy’) (18,19) of which we are aware has utilized mHealth components to address preconceptional health needs, however, this protocol is being implemented in the Netherlands where preconceptional healthcare is more readily available as compared to the U.S. Researchers have also documented that preconceptional women hold generally positive opinions about using mobile technology for promoting health (20). One study examined beliefs about using a smartphone device for engaging in a health behavior change program in women with overweight/obesity. Women reported smartphones to be convenient tools with great utility for health promotion and expressed high levels of acceptability for using a smartphone for this purpose (21).
Our focus is on redeveloping the SHW intervention to be delivered via smartphone (i.e., SMART SHW). The SHW intervention framework offers an evidence-based approach for improving women’s health outcomes before and between pregnancy, and research suggests harnessing mobile technology can increase the program’s reach, and decrease cost and burden, while maintaining (or enhancing) participant acceptability (17,20,21). To successfully construct SMART SHW’s prototype, an imperative first step entails eliciting feedback from the target population about which aspects of the intervention they would prefer to engage with by smartphone. This affords the opportunity to develop SMART SHW in a fashion that is tailored to women with overweight/obesity to improve health before pregnancy. We conducted formative community-engaged research to elicit and characterize pre- and interconceptional overweight/obese women’s preferences for the type of SHW components, activities, and content (e.g., education materials, motivational support, self-regulation tools) they would like to receive via smartphone in SMART SHW to decrease face-to-face participation burden while preserving acceptability. A secondary study purpose was to use these data to assess the feasibility of adapting components of the original SHW intervention for mobile delivery, and to develop and disseminate an evidence-informed prototype of SMART SHW.
Methods
Study procedures
The Pennsylvania State University Institutional Review Board approved this study. With the consent of the community providers, women were recruited through community YMCAs and Family Health Council of Central Pennsylvania sites. Recruitment materials [e.g., informational forms, folio cards in Women, Infants, and Children (WIC) envelopes, pull tab flyers], as well as study endorsement from the staff, were used at the sites to encourage recruitment. Interested women were screened for eligibility by study staff over the telephone. Eligibility criteria were age 18–35 years, English-speaking, BMI greater than 25, currently not pregnant, and still capable of becoming pregnant in the future (e.g., no hysterectomy or health condition preventing pregnancy). One hundred twenty-five women were interested in participating in the study, from which 32% (N=40) participated. Reasons for not participating among the other 68% included not eligible (29%), not interested (13%), no response (12%), no time to participate (10%), and 4% contacted us after recruitment ended. Interested and eligible women were asked to attend an interview at which time written informed consent and self-reported demographic information (i.e., age, education, race/ethnicity, family income, pregnancy status, height, weight) was obtained. Thirty-nine women participated in small group interviews (ranging from 2–5 women). One woman completed an individual interview due to a schedule conflict.
Semi-structured focus group interviews
A trained moderator explained the study goal and facilitated the interviews. Women were asked to envision a scenario in which they were participating in a health behavior change program and asked to identify which aspects of the program they would prefer to receive via smartphone. The moderator described the six session SHW intervention (10), focused on enhancing preconceptional health across four content areas: physical activity, nutrition/healthy eating, stress management, and weight management. Then, the core intervention components and activities (i.e., tracking and monitoring; homework, quizzes and surveys; prompts, reminders, and motivational messaging; education and knowledge; examples and demonstrations) were presented and explained to the participants. Women were asked to share their ideas on how a variety of smartphone-based tools (e.g., texting, mobile apps, internet, web-based videos) could be harnessed to enhance the delivery of, and engagement with, the program. Participants were also prompted to provide mobile design suggestions. It took women about 60 min to complete the review and discussion. The interviews were audio tape recorded using an Olympus DM-420 digital voice recorder and transcribed. Sample size was determined by data saturation (i.e., once no new information produced a change in the coding schemes, data saturation was reached and no further interviews were scheduled) (22).
Mobile redesign decision-making process
The study team, made up of experts from a variety of relevant fields (e.g., kinesiology, exercise and health psychology, obstetrics, prevention science) met extensively to review all SHW smartphone redevelopment and refinement preferences provided by the participants. All intervention components and activities were discussed, and relevant data from the interviews (e.g., smartphone delivery suggestions, salient themes, component and activity preferences) were examined collectively by the study team. Through this process, the researchers were able to make evidence-informed decisions regarding which aspects of the SMART SHW intervention should retain a face-to-face delivery mode, and which components and activities could be adapted for delivery via a smartphone.
Data analysis
Descriptive statistics were used to examine the types of intervention components and activities participants preferred to engage with via smartphone, as well as to determine what portion of SHW material from each content area would need to be redeveloped. Demographic data were analyzed with SPSS (v. 22). Interviews were downloaded and transcribed. Principles of thematic analysis were used to code the interviews (i.e., initial review/coding main concepts, identify coding schemes, sort notes into subcategories, adapt/finalize schemes) (23). Two co-authors independently reviewed each transcribed interview and developed categories of responses from the data; all co-authors reviewed these data categories, clarified discrepancies, and finalized the themes.
Results
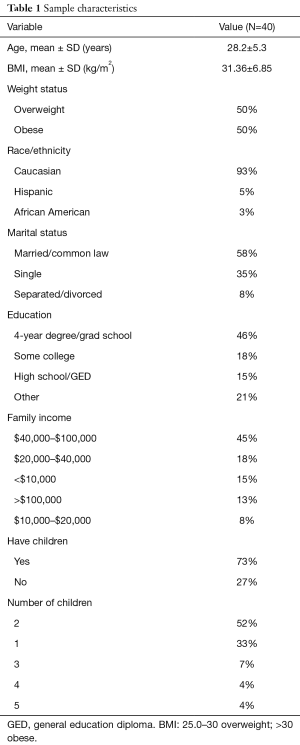
Participants and device ownership
A sample of 40 community women with overweight/obesity, ages 18–35, was recruited (see Table 1). The mean age at enrollment was 28.2 years (SD =5.3), and the mean BMI of the sample was 31.4 (SD =6.85). All participants were residents of counties in Central Pennsylvania, the majority of which are rural and low-income. The majority of the women in the sample was Caucasian (93%), had at least some college education (64%), were married (58%), and had a household income <$40,000 (54%). All participants owned a cell phone (100%), and the majority (85%) had a smartphone device.
Full table
Mobile design suggestions
All participants, regardless of smartphone versus basic cell phone ownership, exhibited familiarity with the different capabilities and tools available via smartphone device (e.g., apps, video, mobile web). Women uniformly noted the utility of the smartphone for enhancing program delivery, but also stressed that SMART SHW should not lose all face-to-face sessions and engagements (see Table 2). A variety of salient themes emerged related to overall mobile intervention design. Many similar suggestions appeared across focus groups, and participants also shared ideas on specific delivery tools and mechanisms that could be harnessed.

Full table
One of the most salient emergent themes was that the smartphone is advantageous for streamlining the amount of information (e.g., program communications, educational handouts) associated with the program, making it all accessible on the same platform, and displayed in a concise manner. Women also noted the utility of mobile devices for tracking goals and monitoring their progress, and offered suggestions of apps they are already familiar with to enhance tracking (e.g., MyFitnessPal, social media applications). It was suggested that surveys and assessments could be provided via smartphone, as long as they were simple to respond to (e.g., tapping a button to indicate an answer as opposed to typing out a response). Women also gave support for harnessing a phone’s ability for streaming audio/video to supplement curricular content that may have otherwise been provided face-to-face. Women supported the ability of the phone to push prompts and reminders about program progress or weekly goals, and suggested methods for delivery (e.g., pop-ups). They also noted this was a useful way to extend the reach of the program. Platforms that women noted for streamlining all of these digital capabilities on the smartphone included utilizing apps, text messaging, email, and/or a mobile compatible program website. Participants indicated that burden and barriers when using a smartphone as part of the intervention (e.g., data usage costs, technical help) should be considered when redeveloping SHW to harness mobile devices.
Intervention element delivery and acceptability preferences
All of the components, activities, and content from the six-session, 12-week SHW program were presented and explained to participants. During the interviews, women described their preferences for which intervention elements could be received on a mobile device. In the original SHW intervention (10), during in-person sessions, participants took part in six types of curricular components, including: (I) tracking/monitoring progress; (II) homework, quizzes, and surveys; (III) reminders and motivational messages; (IV) receiving psychoeducational materials; (V) seeing examples and demonstrations by group leaders; and (VI) receiving paper handouts with information. Table 3 provides an overview of women’s feedback on how material from the four content areas (weight management, stress management, nutrition, and physical activity) could be adapted for mobile administration in each of the six types of curricular components. Women’s feedback fell into two overarching categories: suggestions related to content, and suggestions related to process.
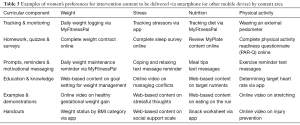
Full table
Figure 1 presents the percentages of content women prefer to be delivered via smartphone by content area and curricular component (excluding handouts, as they are a delivery method used across multiple curricular components). All face-to-face content was presented to all participants, and they indicated which particular components and activities they prefer to engage with via smartphone instead of in-person. This serves as an indicator of the amount of SHW content that will need to be redeveloped to go mobile in SMART SHW, in turn informing an estimate of the amount of resources (e.g., computer programming, time) that prototype development will require. Overall, women most strongly preferred converting curricular elements related to education and knowledge to mobile, followed by homework, quizzes and surveys; tracking and monitoring; examples and demonstrations; and prompts, reminders, and motivational messaging.

Incorporating participant mobile redesign preferences
Upon reviewing focus group data, the study team noted 31 higher order mobile redesign preferences that emerged from the interviews that met criteria for additional discussion (e.g., brainstorming of how a particular activity could be delivered via smartphone; study team member opinion differed strongly from participant preference; mobile redesign preference has not previously been attempted via smartphone). After discussing the feasibility of converting related SHW elements for access via smartphone, the team supported 27 of these particular participant suggestions, thus, 87% of participants’ mobile redesign preferences and suggestions were incorporated into the final SMART SHW prototype.
Discussion
Study goals
In an effort to limit implementation costs and barriers, decrease participant burden, and enhance participant acceptability for the SHW intervention (10,11), this study attempted to synthesize pre- and interconceptional overweight and obese women’s preferences for which aspects of SHW could be adapted for delivery via a smartphone device. Semi-structured focus group interviews provided women with an opportunity to examine SHW components and activities across all sessions and content areas. Descriptive statistics and thematic analyses of the transcribed interviews were used to examine participants’ perceptions of how smartphone-based mediums (e.g., texting, apps) could be harnessed to refine intervention delivery, increase reach, decrease burden, and enhance acceptability. Participant ideas regarding the feasibility of engaging with a smartphone for different aspects of the SHW program, as well as initial design suggestions, were provided. Salient themes relevant to the delivery of a redeveloped program were identified. The study also sought to utilize the interview data to develop a prototype for the redesigned SMART SHW intervention.
This new iteration of the evidence-based SHW program aims to utilize multiple smartphone capabilities to enhance the accessibility and availability of the intervention, while decreasing financial and other barriers related to extensive face-to-face implementation and facilitate ongoing participant engagement. Smartphone delivery offers a mode through which SMART SHW content can potentially be easily accessed, allowing for broader dissemination of the program. Employing smartphones to provide some intervention components also decreases the time needed for face-to-face engagements, minimizing delivery costs. Reducing in-person obligations lessens engagement burden, which may increase the acceptability of taking part in the program among pre- and interconceptional women.
Key findings
Women examined all SHW intervention content, and provided feedback for which portions of the SHW curriculum they would like to receive via smartphone. These preferences were examined for each of the curricular content areas (i.e., weight, stress, nutrition, physical activity), and across all types of curricular components (e.g., handouts, homework, tracking). Mobile design suggestions were also provided, affording the study team valuable data on women’s preferences for how they would like to engage with curricular components on a mobile device. Women prefer texting, mobile websites, and an app for receiving SMART SHW surveys, communications, and educational materials. For tracking nutrition and activity, women preferred to use MyFitnessPal and a wearable pedometer. Design themes that emerged in the interviews included using pop-up prompts for reminders, web-based video supplements, and displaying on-screen information in a concise format. Related to intervention delivery, findings suggested that women in the study had a strong desire to retain certain aspects of each of the six face-to-face sessions. Guided by accepted principles for conducting formative community-based research (24) and established standards from information science and human-centered design (25), the study team integrated and examined all collected data.
Proposed SMART SHW prototype
Through a comprehensive evidence-informed decision-making process, the study team developed a prototype for the newly proposed SMART SHW intervention that accounted for both the mobile and face-to-face delivery preferences of women. Although every effort was made to accommodate specific mobile redesign suggestions made by participants (overall incorporation of participant preferences =87.1%), for some decision points it was necessary for the study team to carefully consider participant preferences against: (I) feasibility for converting a particular component or activity to a mobile format; and (II) researcher expertise and experience in previous intervention design and deployment. For example, during the program, participants learn how to determine their target heart rate, a vital competency for achieving physical activity behavior change through the intervention. Although participants reported they would be comfortable learning this skill via a smartphone app, the study team felt that—due to the importance of this task (and need that it be performed correctly and accurately)—this content should be covered during a face-to-face session. In some instances where researcher expertise did not align with participant preferences, curricular activities could be offered in a hybrid fashion, with some of the engagement occurring on the smartphone device, but follow-up would be conducted face-to-face.
In the newly proposed SMART SHW prototype, women’s preferences for attending six face-to-face sessions across twelve weeks have been retained, however the time and resources needed for the face-to-face portion of the intervention have been drastically reduced by introducing six highly acceptable smartphone-based intervention delivery and assessment modes that compliment face-to-face meetings: online/web-based content; online videos; mobile apps; text messages; MyFitnessPal; and a wearable pedometer. Participants interact with the majority of the intervention’s components and activities, across all content areas (i.e., weight, stress, nutrition, physical activity), via smartphone. Figure 2 presents an infographic summarizing the SMART SHW prototype design.
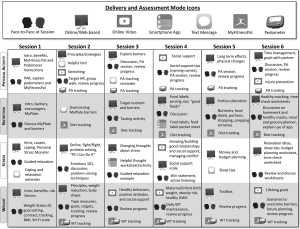
Establishing the SMART SHW prototype is just the beginning of the ongoing intervention development process. For example, face-to-face curricular content across the six sessions must be streamlined, and must also provide instruction for engagement with the newly established smartphone components. Final SMART SHW development will require working with appropriate technology experts for converting content to mobile formats. Learning designers will need to provide input on developing informative online videos and web-based material. Computer programmers will need to be recruited to develop usable mobile app content and monitoring tools. Throughout the process, consideration to information security and the assurance of participant anonymity and data encryption is essential.
Study limitations
Although the sample size was adequate as determined from data saturation, only a small group of mostly Caucasian women residing in communities in rural Pennsylvania participated. Additional adaptations to the intervention may be necessary to appropriately tailor it for other demographic groups (e.g., racial minorities, those residing in other geographic areas—such as urban settings). The women who participated were between the ages of 18–35; preferences of pre- and interconceptional women outside this age range (both younger and older) are not represented in this study. The work was cross-sectional in nature, so data regarding how these women’s perceptions may change over time were not captured. All women were familiar with the smartphone device and its capabilities, so differences in mobile design suggestions between women who owned basic cell phones (15%) vs. smartphones (85%) were not examined. Finally, participants were presented with SHW session content before providing smartphone delivery preferences, which may have introduced self-report and ordering bias. A separate paper (21) addresses women’s general preferences (outside the context of the SHW intervention) for using smartphones as tools for preconceptional health behavior change.
Conclusions
In summary, the SMART SHW intervention’s purpose is to help address a strong public health call for improving pregnancy and early life outcomes for both mother and child, especially those related to maternal obesity (1-5,26). The preconceptional period may be a particularly important and advantageous time to provide women with evidence-based programming aimed at fostering healthy behavior change, while also reducing future adverse pregnancy outcomes (8,26). Through a redevelopment of the empirically supported and effective SHW intervention (11,12) to be extended to harness mHealth technology, the proposed SMART SHW prototype has the potential to expand intervention reach and delivery, limit implementation costs, and reduce participant burden. Moreover, our end-user design input approach helps ensure that the tailoring of mobile intervention components and activities will facilitate participant acceptability. These results demonstrate that pre- and interconceptional overweight and obese women report this mobile intervention approach to be feasible, and are open to receiving SMART SHW content via smartphone—particularly in conjunction with in-person sessions. Next steps are to move forward with platform development and testing, followed by a randomized controlled clinical trial of the intervention’s efficacy for improving a variety of biobehavioral health outcomes related to obesity and pregnancy.
Acknowledgements
Funding: This project was supported by the Penn State CTSI Community Engagement and Research Core through National Center for Research Resources and the National Center for Advancing Translational Sciences. FT Materia was supported in part by the National Center for Advancing Translational Sciences of the National Institutes of Health Award Number TL1TR002016.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to report.
Ethical Statement: The study was approved by the Institutional Review Board of The Pennsylvania State University (IRB approval #42308). Informed consent was obtained from all participants before enrollment into the study.
References
- Institute of Medicine (US) and National Research Council (US) Committee to Reexamine IOM Pregnancy Weight Guidelines; Rasmussen KM, Yaktine AL. editors. Weight Gain During Pregnancy: Reexamining the Guidelines. Washington (DC): National Academies Press (US); 2009.
- Dalenius K, Brindley P, Smith B, et al. Pregnancy Nutrition Surveillance 2010 Report. Atlanta: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention; 2012.
- Bodnar LM, Siega-Riz AM, Simhan HN, et al. Severe obesity, gestational weight gain, and adverse birth outcomes. Am J Clin Nutr 2010;91:1642-8. [Crossref] [PubMed]
- Lu GC, Rouse DJ, DuBard M, et al. The effect of the increasing prevalence of maternal obesity on perinatal morbidity. Am J Obstet Gynecol 2001;185:845-9. [Crossref] [PubMed]
- Flegal KM, Carroll MD, Kit BK, et al. Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999-2010. JAMA 2012;307:491-7. [Crossref] [PubMed]
- Thangaratinam S, Rogozińska E, Jolly K, et al. Interventions to reduce or prevent obesity in pregnant women: a systematic review. Health Technol Assess 2012;16:iii-iv, 1-191. [Crossref] [PubMed]
- Downs DS. Obesity in Special Populations: Pregnancy. Prim Care 2016;43:109-20. ix. [Crossref] [PubMed]
- Johnson K, Posner SF, Biermann J, et al. Recommendations to improve preconception health and health care--United States. A report of the CDC/ATSDR Preconception Care Work Group and the Select Panel on Preconception Care. MMWR Recomm Rep 2006;55:1-23. [PubMed]
- Temel S, van Voorst SF, Jack BW, et al. Evidence-based preconceptional lifestyle interventions. Epidemiol Rev 2014;36:19-30. [Crossref] [PubMed]
- Downs DS, Feinberg M, Hillemeier MM, et al. Design of the Central Pennsylvania Women's Health Study (CePAWHS) strong healthy women intervention: improving preconceptional health. Matern Child Health J 2009;13:18-28. [Crossref] [PubMed]
- Hillemeier MM, Downs DS, Feinberg ME, et al. Improving women's preconceptional health: findings from a randomized trial of the Strong Healthy Women intervention in the Central Pennsylvania women's health study. Womens Health Issues 2008;18:S87-96. [Crossref] [PubMed]
- Weisman CS, Hillemeier MM, Downs DS, et al. Improving women's preconceptional health: long-term effects of the Strong Healthy Women behavior change intervention in the central Pennsylvania Women's Health Study. Womens Health Issues 2011;21:265-71. [Crossref] [PubMed]
- Luxton DD, McCann RA, Bush NE, et al. mHealth for mental health: Integrating smartphone technology in behavioral healthcare. Prof Psychol Res Pr 2011;42:505-12. [Crossref]
- Baig MM. GholamHosseini H, Connolly MJ. Mobile healthcare applications: system design review, critical issues and challenges. Australas Phys Eng Sci Med 2015;38:23-38. [Crossref] [PubMed]
- Zhao J, Freeman B, Li M. Can Mobile Phone Apps Influence People’s Health Behavior Change? An Evidence Review. J Med Internet Res 2016;18. [Crossref] [PubMed]
- Lathia N, Pejovic V, Rachuri KK, et al. Smartphones for large-scale behavior change interventions. Accessed on February 2, 2016. Available online: https://www.cl.cam.ac.uk/~cm542/papers/ieeepervasive2013.pdf
- Tamrat T, Kachnowski S. Special delivery: an analysis of mHealth in maternal and newborn health programs and their outcomes around the world. Matern Child Health J 2012;16:1092-101. [Crossref] [PubMed]
- Van Dijk MR, Huijgen NA, Willemsen SP, et al. Impact of an mHealth Platform for Pregnancy on Nutrition and Lifestyle of the Reproductive Population: A Survey. JMIR Mhealth Uhealth 2016;4:e53.[Crossref] [PubMed]
- van Dijk MR, Oostingh EC, Koster MP, et al. The use of the mHealth program Smarter Pregnancy in preconception care: rationale, study design and data collection of a randomized controlled trial. BMC Pregnancy Childbirth 2017;17:46. [Crossref] [PubMed]
- Willcox JC, van der Pligt P, Ball K, et al. Views of Women and Health Professionals on mHealth Lifestyle Interventions in Pregnancy: A Qualitative Investigation. JMIR Mhealth Uhealth 2015;3. [Crossref] [PubMed]
- Symons Downs D, Feinberg M, Heron K, et al. Women’s preferences about using smartphones in a preconceptional health intervention. Ann Behav Med 2015;49:S1.
- Guest G, Bunce A, Johnson L. How many interviews are enough? An experiment with data saturation. Field Methods 2006;18:59-82. [Crossref]
- Green J, Browne J. Analysing Qualitative Data. In: Black N, Raine R, Green J, et al. editors. Principles of Social Research. New York, NY: McGraw-Hill, 2005.
- Young DR, Johnson CC, Steckler A, et al. Data to action: using formative research to develop intervention programs to increase physical activity in adolescent girls. Health Educ Behav 2006;33:97-111. [Crossref] [PubMed]
- International Organization for Standardization. ISO 2010. Ergonomics of human-system interaction – Part 210: Human-centered design for interactive systems. Available online: [accessed 2017-12-19].https://www.iso.org/standard/52075.html
- Hanson M, Barker M, Dodd JM, et al. Interventions to prevent maternal obesity before conception, during pregnancy, and post partum. Lancet Diabetes Endocrinol 2017;5:65-76. [Crossref] [PubMed]
Cite this article as: Materia FT, Smyth JM, Heron KE, Hillemeier M, Feinberg ME, Fonzi P, Symons Downs D. Preconceptional health behavior change in women with overweight and obesity: prototype for SMART strong healthy women intervention. mHealth 2018;4:24.


