Characteristics of mobile phone access and usage in rural and urban Guatemala: assessing feasibility of text message reminders to increase childhood immunizations
Introduction
Mobile health (mHealth) technologies that use mobile phones for health-related purposes, such as Short Message Service (SMS) texts, have tremendous and untapped potential for disease management (1,2), especially in low- and middle-income countries (LMICs) where mobile penetration is high and wireless technology is often less expensive and more accessible than wired technology (3,4). One important example of this involves improving the childhood vaccination series. Immunization is one of the most successful and cost-effective public health interventions, saving millions of lives every year. Despite considerable effort to promote vaccine coverage in LMICs, the World Health Organization goal to reach more than 90% of children under the age of one worldwide has remained a significant challenge with nearly 20 million infants under-immunized and even more children receiving delayed vaccinations, placing them at risk for unnecessary morbidity and mortality (5-7). Completion rates for the primary vaccination series in Guatemala remain below this goal with some rural areas having less than 70% coverage (8).
A major barrier to delivering primary healthcare services, such as childhood vaccines, in LMICs is the lack of a functioning preventive health system and the difficulty providers have in communicating with parents the importance and timeliness of these vaccines. Patient reminder systems (including postcards, letters, e-mails, and telephone or auto dialer calls) are an important mechanism for improving childhood vaccination coverage (9,10) and can be easily adapted to SMS platforms (11-16). Several pilot feasibility and acceptability studies using SMS reminders have shown promising results in LMICs (17-21). While there is growing evidence to support SMS applications for health promotion, most research has been done in high-income countries, studies have focused on small-scale implementation and pilot projects, and the evaluation of these interventions in LMICs has been inconsistent (22-25). We lack an understanding of the barriers and facilitators to program design, implementation, and scale in LMICs where potential for impact is high. Understanding the real-world context in which interventions are implemented is imperative for successful mHealth program adoption, replication, and widespread dissemination.
Our study team conducted an initial pilot study in collaboration with the Ministry of Health of Guatemala and the Pan American Health Organization demonstrating that a novel application of SMS technology to provide patient reminders for childhood immunizations in an urban setting of an LMIC was able to reach parents with great consumer satisfaction (19). We are now conducting a randomized controlled trial to optimize, implement, and evaluate this system in both a rural and urban setting of Guatemala. The current study analyzed data from the baseline demographic survey of this trial with the objective to identify factors related to mobile phone accessibility and usage that contribute to the feasibility of an SMS-based vaccination reminder system that aims to improve completion of the infant primary immunization series in Guatemala.
Methods
We analyzed demographic survey data completed at the enrollment visit from a randomized controlled trial. Randomization occurred after this initial enrollment visit, and therefore, is not described in this manuscript. The study was conducted at four public health clinics. The government clinics serve a low-income population with two of the clinics located in the urban setting of Guatemala City and two in the rural southwest Trifinio region of Guatemala. Enrollment occurred between March to November 2016. Participation was voluntary and patients were not given any incentives. The Colorado Multiple Institutional Review Board, the Universidad del Valle Ethics Committee, and the Guatemala National Ethics Committee of the Ministry of Public Health and Social Assistance reviewed and approved the research. Written informed consent was obtained from all parents or guardians (henceforth referred to as parent).
Participants
Eligible participants included infants between the ages of 6 weeks to 6 months who were medically cleared to receive the first dose of the 3-dose infant primary immunization series. Participants were excluded if the study clinic was not the patient’s primary clinic, the consenting parent was under 18 years of age, or the parent did not speak Spanish. At least one parent needed to own an active mobile phone capable of receiving SMS messages, be able to use SMS text messaging, and be literate and able to decipher the messages for themselves or by a surrogate in the household. Equal numbers of rural and urban participants were enrolled at the four clinic sites.
Data collection
At the enrollment visit, all parents completed a baseline demographic survey. Surveys were pretested by our study group in Guatemala prior to the study commencement. A study nurse assigned to each clinic administered the surveys in a quiet and confidential location during the immunization visit. Nurses collected data on a tablet device. Study data were collected and managed using Research Electronic Data Capture (REDCap) electronic data capture tools hosted at the University of Colorado Denver (26). REDCap is a secure, web-based application designed to support data capture for research studies, providing: (I) an intuitive interface for validated data entry; (II) audit trails for tracking data manipulation and export procedures; (III) automated export procedures for seamless data downloads to common statistical packages; and (IV) procedures for importing data from external sources.
Statistical analysis
Chi-square or Fisher’s exact and Student’s t-test were used to assess significance levels in demographic differences to describe factors, such as mobile phone accessibility and usage, that contribute to the feasibility of using SMS to increase vaccine compliance in this setting. All statistical tests were considered to be significant at a two-tailed P value less than 0.05. All analyses were conducted using SAS (SAS 9.4, SAS Institute, Cary, NC, USA).
Results
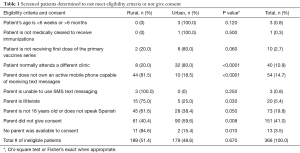
Of 1,088 families approached for enrollment, 871 were eligible and 720 (82.7%) participated with an equal number of urban and rural children enrolled (Table 1). Of all patients screened for eligibility, only 54 (5.0%) parents did not own a mobile phone with SMS capability, 3 (0.3%) parents could not use SMS, and 20 parents (1.8%) were illiterate and unable to decipher SMS messages. Of the ineligible patients, more parents in the rural clinics did not own a mobile phone with SMS capabilities compared to the urban clinics (81.5% vs. 18.5%, P<0.0001), and more rural parents were illiterate and unable to decipher SMS texts (75.0% vs. 25.0%, P=0.030).
Full table
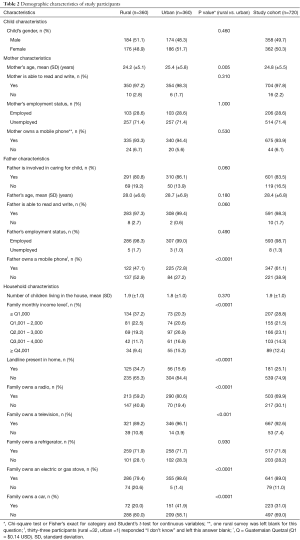
Mothers had an average age of 24.8 [standard deviation (SD) ±5.5] years, 97.8% (n=704) were literate, and 28.6% (n=206) employed. Most families (n=601, 83.5%) had a father involved. Fathers had an average age of 28.4 (SD ±6.8) years, 98.3% (n=591) were literate, and 98.7% (n=593) employed. Interestingly, there was no significant difference between urban and rural maternal mobile phone ownership (94.4% vs. 93.3%, P=0.530), but more urban fathers owned mobile phones compared to rural fathers (72.8% vs. 47.1%, P<0.0001). Additionally, overall, more mothers compared to fathers owned mobile phones (93.9% vs. 61.1%, P<0.0001). Urban participants reported a significantly higher trend in monthly income (P<0.0001) and more ownership of radios (P<0.0001), televisions (P<0.001), stoves (P<0.0001), and cars (P<0.0001), but rural participants reported more telephone landlines (P<0.0001). Table 2 summarizes the demographic characteristics of the study participants.
Full table
Families chose to have reminders sent to the mother (n=651, 90.4%), father (n=67, 9.3%), or a guardian (n=2, 0.3%). Most families (n=480, 66.7%) had at least two active mobile phones present in the home, with urban families owning more mobile phones (P<0.0001). Most participants reported a daily average of fewer than or equal to 5 telephone calls made (n=629, 87.4%), fewer than or equal to 10 texts sent (n= 655, 91.0%), and fewer than or equal to 10 texts received (n=647, 89.9%), with urban families reporting significantly greater telephone usage (P=0.006, P<0.001, and P<0.001, respectively). Parents generally preferred to make calls over sending texts (74.7% vs. 25.3%, P<0.0001), with more urban families preferring text messaging (31.9% vs. 18.6%, P<0.0001). Over one-half (n=419, 58.2%) of participants had their current mobile phone for at least 1 year, with urban participants having their phones longer (P<0.0001). Participants spent an average of $9.50 USD per month for mobile phone services. Table 3 summarizes the mobile phone characteristics of the participants.

Full table
Discussion
Results from our study show that almost all parents in both the urban and rural low-resource settings studied in Guatemala had access to a mobile phone with SMS capability and were able to use SMS technology. Furthermore, our results provide important insight into mobile phone access, usage, and preferences for voice and text communication across urban and rural populations of an LMIC that may be used in similar global settings to inform future mHealth interventions. Overall, we suggest that using SMS in combination with voice calls in LMICs can be a feasible and effective tool to reach parents and remind them of future healthcare visits for their child. Our work emphasizes the importance of assessing parent preference for communication via text or phone and that structuring messaging based on preference can help increase compliance with primary care services such as timing and completion of the childhood vaccine schedule.
Although calls for improved translation of research findings to clinical practice have accompanied a growth in translational research in the U.S., we are only recently seeing research in LMICs focused on dissemination and scale. One of the primary reasons to support mHealth is the potential for technology to reach many more people than traditional interventions, but despite the positive results of many mHealth research studies, the translation of research findings to clinical practice and policy for mHealth in particular remains poor (27-29). Furthermore, there appears to be an attitude in the field that ever greater technological complexity is representative of innovation, while in fact, this seduction by technology is concomitant with tens of thousands of mHealth applications (apps) and solutions languishing with few users and, therefore, no impact (30). There remains little understanding of the barriers and facilitators to program adoption and more widespread dissemination in either a local or global context. A salient example is the failed replication of a mobile phone text message platform for improving adherence to antiretroviral therapy. This intervention was shown to be effective in two Kenyan studies but did not show a significant effect when replicated in a third trial in Cameroon (31). This highlights the fact that understanding the real-world context in which interventions are implemented is imperative for successful program adoption, replication, and scale-up. Understanding barriers and benefits to intervention adoption among both individuals and systems is a major gap in overall program dissemination and implementation potential.
Our study results explore some of these important barriers and facilitators related to mobile phone access and usage that impact using SMS technology for interventions such as vaccine reminders for childhood immunizations. The results suggest that SMS may currently be a better mode of reminder in the urban population compared to our rural setting given the differing degrees of mobile phone ownership, turnover, and usage within these populations. Using landlines or making mobile phone calls may be more effective at reminding rural families about healthcare visits in many LMIC settings. It is important to remember that the primary innovation of an mHealth reminder system is in its reach or the ability of using such technology, in all its forms, to facilitate universal access to care. While more traditional technologies, such as telephone landlines or making mobile phone calls, may be viewed by some as antiquated and less innovative, we submit that this view will limit a pragmatic and logical approach combining both SMS texts and traditional voice communication that can offer increased access to care. We should offer reminder delivery modalities based on client preference, and this work suggests that text messaging in additional to other more traditional communication methods is appropriate to maximize reaching our target population. If the evidence does not support people embracing a more advanced or sophisticated technology, then we would be remiss to advocate solely for such interventions. When a new technology becomes available, research has shown that it often raises awareness and appreciation for other preexisting technologies as well (32). In the case of mHealth platforms, it will be important to monitor trends in mobile phone access and usage over time and to remain flexible in adapting interventions to fit the population’s ability and desire for Information and Communication Technology (ICT), which in LMICs will likely include using a combination of more traditional communication methods with newer, modern technologies. Community input and collaboration will be necessary to consider the local context of global mHealth interventions (33), especially related to immunization services (34).
Another important finding in our study is the high ownership of mobile phones among both urban and rural mothers and the significantly greater ownership of mobile phones among mothers compared to fathers. We found that over 90% of both rural and urban mothers owned a mobile phone, which is substantially greater than the 25–50% ownership rates among women found in other similar studies (17,20). Additionally, while few gender ICT statistics are available, studies have repeatedly suggested a gender digital gap by showing that the usage of ICT is lower among women than men, especially in LMICs (35). It is interesting that our study found mothers to have significantly greater ownership of mobile phones compared to fathers and that at least 90% of rural and urban families preferred to have the reminder messages sent to the mother’s phone (even when the father also owned a mobile phone). These findings suggest that targeting mothers for mobile phone interventions will likely provide the greatest benefit in our study population and potentially in similar LMIC settings.
Our study has important limitations. We did not explore several mediums of ICT that would be useful to look at in future studies, including computer, Internet, and smartphone access or usage. Certain mediums may be more effective for specific disease prevention and health promotion and future interventions may include more advanced mHealth applications (36), making this an important area for further study. For example, smartphones could be used to send graphical messages via SMS or applications such as WhatsApp Messenger to remind illiterate parents about appointments. Additionally, we did not explore the important concept of shared mobile telephones. Studies have suggested that phone sharing among family members may be common in LMICs, although the prevalence is largely unknown (23). While at least one-half of both the rural and urban families in our study reported having more than one mobile phone present in the household, we do not know if these phones were shared among multiple users. This will be an important area for future exploration since phone sharing could have significant implications for SMS interventions and whether the text messages are reaching the intended recipients. We also do not know why nearly 14% of patients screened for participation did not consent to receiving SMS messages. The rationale for refusing SMS reminders and study participation will be important to investigate further.
Our study is particularly innovative because it is one of the first large trials to explore mobile phone access and usage in both a rural and urban setting of an LMIC. While there is a general lack of evidence to inform large-scale planning and national policy development for mHealth interventions (23), this study provides an innovative partnership with the Ministry of Health of Guatemala that could provide the unprecedented opportunity for national scalability and be a future platform for the delivery of other clinical preventive services. Importantly, our study identifies current trends and barriers in mobile phone usage among rural and urban populations that can help guide future mHealth interventions and can ultimately contribute to our knowledge of vaccine delivery and the rapidly growing field of mHealth.
Conclusions
Researchers consider the burgeoning field of mHealth to have the potential to attain widespread dissemination of public health programs that would be impossible with traditional interventions. However, to date, we have yet to see mHealth interventions widely disseminated and scaled due to only limited empirical evidence of effectiveness. There is a need for a greater number of studies evaluating SMS interventions with sound methodology, adequate sample sizes, and an understanding of the barriers and facilitators of dissemination and implementation, especially based in resource-limited settings. Our study results provide important insight into mobile phone access and usage within rural and urban low-resource settings of an LMIC that can be used to inform future mHealth interventions. Our findings suggest that offering a combination of more traditional communication methods (such as using landlines or making mobile phone calls) with newer, modern technologies (such as SMS texting) may be more effective at reminding families about vaccination visits, particularly for our rural population. We also found that mothers in our LMIC setting had high ownership of mobile phones and preferred to have the reminder messages sent to them, which suggests that targeting mothers for mHealth interventions will likely provide the greatest benefit. Overall, our study suggests that using SMS reminders in conjunction with other more traditional reminder methods in LMICs can be a feasible tool for public health interventions both now and in the future, especially as mobile telecommunication infrastructure and uptake is likely to continue expanding on a global scale.
Acknowledgements
We thank the parents and children who participated in our study. We also thank our data manager Jose Rivera, our project administrators Mirsa Ariano and Michelle Shiver, and our study nurses.
Funding: This work was supported by the Eunice Kennedy Shriver National Institute of Child Health & Human Development at the National Institutes of Health (grant number 1R21HD084115-01); and the Thrasher Research Fund Early Career Award Program (award number 12797). REDCap was supported by the National Institutes of Health and National Center for Research Resources Colorado CTSI (grant number UL1 RR025780).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The Colorado Multiple Institutional Review Board (protocol 14-2170), the Universidad del Valle Ethics Committee (protocol 113-01-2015), and the Guatemala National Ethics Committee of the Ministry of Public Health and Social Assistance (protocol 11-2015) reviewed and approved the research. Written informed consent was obtained from all parents or guardians
References
- Head KJ, Noar SM, Iannarino NT, et al. Efficacy of text messaging-based interventions for health promotion: A meta-analysis. Soc Sci Med 2013;97:41-8. [Crossref] [PubMed]
- Wei J, Hollin I, Kachnowski S. A review of the use of mobile phone text messaging in clinical and healthy behavior interventions. J Telemed Telecare 2011;17:41-8. [Crossref] [PubMed]
- Déglise C, Suggs LS, Odermatt P. Short message service (SMS) applications for disease prevention in developing countries. J Med Internet Res 2012;14:e3. [Crossref] [PubMed]
- Bull S, Domek GJ, Thomas D. eHealth and Global Health Promotion. In: Zimmerman RS, DiClemente RJ, Andrus JK, et al. editors. Introduction to Global Health Promotion. San Francisco: Jossey-Bass, 2016:145-72.
- World Health Organization. Global Vaccine Action Plan: 2011-2020. Geneva, Switzerland, 2013. Available online: http://www.who.int/immunization/global_vaccine_action_plan/GVAP_doc_2011_2020/en/
- Luman ET, Barker LE, Shaw KM, et al. Timeliness of childhood vaccinations in the United States: Days undervaccinated and number of vaccines delayed. JAMA 2005;293:1204-11. [Crossref] [PubMed]
- Vasudevan L, Labrique AB, Mehra S, et al. Maternal determinants of timely vaccination coverage among infants in rural Bangladesh. Vaccine 2014;32:5514-9. [Crossref] [PubMed]
- VI Encuesta Nacional de Salud Materno Infantil ENSMI 2014-2015. Informe de Indicadores Básicos. Guatemala, 2015. Available online: http://www.osarguatemala.org/osartemporal/Archivos/PDF/201603/259_4.pdf
- Szilagyi PG, Bordley C, Vann JC, et al. Effect of patient reminder/recall interventions on immunization rates: A review. JAMA 2000;284:1820-7. [Crossref] [PubMed]
- Jacobson Vann JC, Szilagyi P. Patient reminder and patient recall systems to improve immunization rates. Cochrane Database Syst Rev 2005.CD003941. [PubMed]
- Kharbanda EO, Stockwell MS, Fox HW, et al. Text message reminders to promote human papillomavirus vaccination. Vaccine 2011;29:2537-41. [Crossref] [PubMed]
- Stockwell MS, Kharbanda EO, Martinez RA, et al. Effect of a text messaging intervention on influenza vaccination in an urban, low-income pediatric and adolescent population. JAMA 2012;307:1702-8. [Crossref] [PubMed]
- Stockwell MS, Kharbanda EO, Martinez RA, et al. Text4Health: Impact of text message reminder-recalls for pediatric and adolescent immunizations. Am J Public Health 2012;102:e15-21. [Crossref] [PubMed]
- Ahlers-Schmidt CR, Chesser AK, Nguyen T, et al. Feasibility of a randomized controlled trial to evaluate Text Reminders for Immunization Compliance in Kids (TRICKs). Vaccine 2012;30:5305-9. [Crossref] [PubMed]
- Stockwell MS, Hofstetter AM, DuRivage N, et al. Text message reminders for second dose of influenza vaccine: A randomized controlled trial. Pediatrics 2015;135:e83-91. [Crossref] [PubMed]
- Hofstetter AM, DuRivage N, Vargas CY, et al. Text message reminders for timely routine MMR vaccination: A randomized controlled trial. Vaccine 2015;33:5741-6. [Crossref] [PubMed]
- Wakadha H, Chandir S, Were EV, et al. The feasibility of using mobile-phone based SMS reminders and conditional cash transfers to improve timely immunization in rural Kenya. Vaccine 2013;31:987-93. [Crossref] [PubMed]
- Bangure D, Chirundu D, Gombe N, et al. Effectiveness of short message services reminder on childhood immunization programme in Kadoma, Zimbabwe - a randomized controlled trial, 2013. BMC Public Health 2015;15:137. [Crossref] [PubMed]
- Domek GJ, Contreras IL, O’Leary ST, et al. SMS text message reminders to improve infant vaccination coverage in Guatemala: A randomized controlled trial. Vaccine 2016;34:2437-43. [Crossref] [PubMed]
- Uddin MJ, Shamsuzzaman M, Horng L, et al. Use of mobile phones for improving vaccination coverage among children living in rural hard-to-reach areas and urban streets of Bangladesh. Vaccine 2016;34:276-83. [Crossref] [PubMed]
- Gibson DG, Kagucia EW, Ochieng B, et al. The Mobile Solutions for Immunization (M-SIMU) trial: A protocol for a cluster randomized controlled trial that assesses the impact of mobile phone delivered reminders and travel subsidies to improve childhood immunization coverage rates in western Kenya. JMIR Res Protoc 2016;5:e72. [Crossref] [PubMed]
- Cole-Lewis H, Kershaw T. Text messaging as a tool for behavior change in disease prevention and management. Epidemiol Rev 2010;32:56-69. [Crossref] [PubMed]
- The Earth Institute, Columbia University. Barriers and Gaps Affecting mHealth in Low and Middle Income Countries. Washington, DC, 2010. Available online: http://cgsd.columbia.edu/files/2012/11/mHealthBarriersWhitePaperFINAL.pdf
- Gurman TA, Rubin SE, Roess AA. Effectiveness of mHealth behavior change communication interventions in developing countries: A systematic review of the literature. J Health Commun 2012;17:82-104. [Crossref] [PubMed]
- Betjeman TJ, Soghoian SE, Foran MP. mHealth in Sub-Saharan Africa. Int J Telemed Appl 2013;2013:482324. [PubMed]
- Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (REDCap) - A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009;42:377-81. [Crossref] [PubMed]
- Bull S. Beyond acceptability and feasibility: Moving mHealth into impact. Mhealth 2016;2:45. [Crossref] [PubMed]
- Batterham PJ, Sunderland M, Calear AL, et al. Developing a roadmap for the translation of e-mental health services for depression. Aust N Z J Psychiatry 2015;49:776-84. [Crossref] [PubMed]
- Peng W, Yuan S, Holtz BE. Exploring the challenges and opportunities of health mobile apps for individuals with type 2 diabetes living in rural communities. Telemed J E Health 2016;22:733-8. [Crossref] [PubMed]
- Brahmbhatt R, Niakan S, Saha N, et al. Diabetes mHealth apps: Designing for greater uptake. Stud Health Technol Inform 2017;234:49-53. [PubMed]
- Mbuagbaw L, van der Kop ML, Lester RT, et al. Mobile phone text messages for improving adherence to antiretroviral therapy (ART): An individual patient data meta-analysis of randomised trials. BMJ Open 2013;3:e003950. [Crossref] [PubMed]
- United Nations, Department of Economic and Social Affairs, Population Division. Trends in Contraceptive Use Worldwide. New York, 2015. Available online: http://www.un.org/en/development/desa/population/publications/pdf/family/trendsContraceptiveUse2015Report.pdf
- Yamey G. Scaling up global health interventions: A proposed framework for success. PLoS Med 2011;8:e1001049. [Crossref] [PubMed]
- Crocker-Buque T, Mindra G, Duncan R, et al. Immunization, urbanization and slums - A systematic review of factors and interventions. BMC Public Health 2017;17:556. [Crossref] [PubMed]
- Hafkin N, Huyer S. Women and gender in ICT statistics and indicators for development. Information Technologies and International Development 2007;4:25-41. [Crossref]
- Chen L, Wang W, Du X, et al. Effectiveness of a smart phone app on improving immunization of children in rural Sichuan Province, China: Study protocol for a paired cluster randomized controlled trial. BMC Public Health 2014;14:262. [Crossref] [PubMed]
Cite this article as: Domek GJ, Contreras-Roldan IL, Asturias EJ, Bronsert M, Bolaños Ventura GA, O’Leary ST, Kempe A, Bull S. Characteristics of mobile phone access and usage in rural and urban Guatemala: assessing feasibility of text message reminders to increase childhood immunizations. mHealth 2018;4:9.


