Pilot study of a smartphone application designed to socially motivate cardiovascular disease patients to improve medication adherence
Introduction
Despite the effectiveness of pharmacotherapy in combating chronic illnesses, in particular cardiovascular disease (CVD), it is estimated that 50% or more of patients are non-adherent to their medications (1). Medication non-adherence leads to poor achievement of treatment goals, increased patient morbidity and mortality, and costs an estimated $300 billion annually in U.S. healthcare expenditures (2). Since measurements of abnormal blood pressure and lipids can be used to objectively approximate adherence, a plethora of data is available regarding medication adherence in CVD patients.
In its 2003 report, the World Health Organization identified five dimensions of medication non-adherence, stressing the multifactorial nature of the problem (3). Simple “forgetfulness” does not explain the majority of non-adherent behavior. It is a much more complex problem involving low patient self-efficacy, ambivalence or resistance to changing health behaviors, and conscious decision-making whereby the cons of taking medications (drug expenses, adverse side effects, etc.) outweigh the pros (enjoying positive health outcomes). There is a need to shift approaches from “blaming” the patient to “supporting” the patient to improve adherence.
One key topic studied extensively in health psychology and behavioral medicine is social support. Studies have shown strong associations between familial support and glycemic control in diabetic patients (4), and that heart failure patients with lower perceived social support (PSS) scores have a 3.5 higher risk of cardiac events than those who have higher PSS (5). Moreover, Miller & DiMatteo’s research highlights the mediating effect of adherence on social support and health outcomes—greater support by family and friends promotes patient adherence by encouraging optimism, altering negative health behaviors, and buffering the stress of being ill, thereby creating better outcomes (6).
Additionally, verification of proper patient usage of prescribed medications is important for clinicians to assess whether the treatment is working. In most outpatient settings, clinicians rely upon the patient’s self-report (7). However, multiple studies have shown that this is not reliable, as patient recall for medical information is poor and patients generally over-report adherence to please the clinician (8). Suboptimal assessment of patient adherence may lead to medication errors, such as over-prescription and dosing errors, compounding medical costs and also increasing the risk of harmful drug interactions and adverse side effects, further compromising treatment efficacy.
The number of apps aimed at helping patients organize and track medication-intake is increasing in various smartphone platforms (9). For example, eMocha uses a video directly observed therapy (DOT) where patients record themselves taking their medication, and providers verify each dose. MediSafe is an advanced medication managing app that works as a virtual pill-box, and includes features such as trend dashboards, medication videos, and the “Medfriend” caregiver support. CeyHello also focuses on patient engagement through the “Care Circle” feature where family members can send patients motivating icons called “moticons”. None of these solutions, however, takes medical social networking to the level at which PillPal does, while also providing adherence verification to clinicians.
Currently, there is no reliable way to motivate patients to take their medications while also accurately verifying appropriate medication adherence to clinicians. Based on a separate interview of over 300 patients, we observed that many older patients identified loneliness as a common daily attribute, and often welcome the opportunity to interact with friends and family. The current study aimed to develop and pilot test PillPal, a newly developed smartphone app that socially connects patients by video chat to promote medication adherence.
Methods
App development
We identified two must-have features for the app: a mode of connecting patients with family members, friends, or with other patients and an effective display of adherence data to clinicians. Because medication-taking behavior is extremely complex and individual, we targeted a solution that can improve adherence in patients universally—that is, to internally motivate patients to engage in treatment. PillPal makes patients look forward to taking their medications by making it an act to be performed together with another individual, fostering new relationships and building a community through the shared experience. In addition to motivating the patient, it is important to display useful adherence data to clinicians. We envision a calendar format that can be used during the clinic visit. Adherence percentage is calculated as the number of pills taken divided by the number of pills prescribed by the physician:
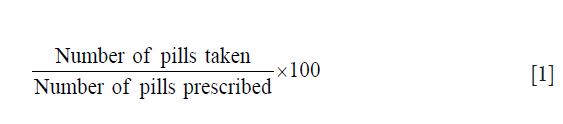
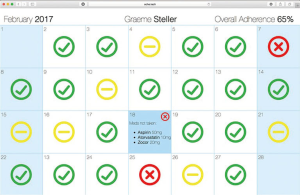
Figure 1 and Figure 2 show current prototypes of the PillPal app and Physician Calendar, respectively.

Patient interviews
We conducted an Institutional Review Board (IRB) approved pilot study of the PillPal app on patients with CVD. The in-person interview followed 3 phases: (I) the patient answered 5 questions regarding their demographics (age, gender, number of daily medications, adherence level to medications, and PSS); (II) the patient used PillPal with a study member, going through all of the actions that are intended to be performed; (III) the patient answered 5 questions soliciting specific feedback on PillPal.
The procedure consisted of steps:
- Study team members visited each of the following recruitment sites: Johns Hopkins Outpatient Center Cardiology/Lipid Clinic and Johns Hopkins Hospital (JHH) Inpatient Cardiology service;
- Seth Martin, MD, MHS asked the patient whether he/she is willing to participate in the study;
- After obtaining permission, patients were consented per the oral consent script. The participation request and oral consenting took place in-person upon investigator(s) visit to each recruitment site;
- Team members conducted the study based on the following design.
Study design:
- Part A: preliminary survey.
- Ask the patient the following questions:
- “What is your age and gender?”
- “What medical condition are you at this hospital for?”
- “How many medications do you take daily?”
- “Have you ever forgotten to take your medication in the last month?”
- “On a scale of 1 to 10, how much do you feel socially supported?” (1= extremely lonely, 10= extremely supported by friends and family).
- Part B: direct observation of patient using ‘PillPal’.
- The patient is handed an iPhone with ‘PillPal’ downloaded;
- The patient is asked to set up a video chat with a second interviewer;
- During the chat, the patient is asked to pretend to take pills (make a hand motion of taking pills without actually ingesting anything). When that is done, the interviewer pretends to take pills and patient is asked to verify on the app that the interviewer took the pill;
- The interviewer and patient continue to have a conversation through the video chat (limited to 5 min).
- Part C: main survey questions for feedback on app.
- Ask the patient the following questions:
- “On a scale of 1 to 10 how would this app affect your motivation level to engage in treatment?” (1= less motivated, 5= no change, 10= more motivated);
- “On a scale of 1 to 10 how easy was it to use the app?” (1= hard to use, 10 = very easy);
- “On a scale of 1 to 10 how comfortable were you video-chatting while taking your pills?” (1= not comfortable, 10= very comfortable);
- “What features do you like about the app?”
- “Do you have suggestions for improvement?”
- “Any general comments?”
Results
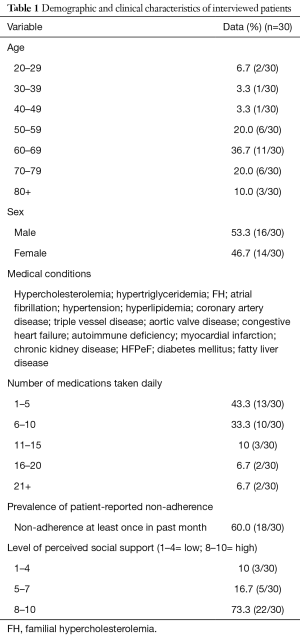
The analytic sample for this study was 30 patients. Inclusion criteria were patients with CVD, currently taking multiple medications, and able to use an iPhone following simple instructions. Exclusion criteria were the inability to use an iPhone following instruction from study member. Participants covered a wide spectrum of cardiac disease, the mean age was 62.7, mean number of daily medications was 8.7, 60% reported at least one episode of non-adherence in the past month, and 27% had a low or moderate level of PSS (Table 1).
Full table
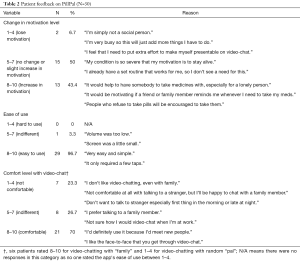
Patients were asked to use PillPal and to critique its usability and potential to motivate medication adherence. Specifically, patients were asked to rank the app regarding how it would change their motivation level for taking medications regularly and at the appropriate time, its ease of use, and their comfort level with video-chatting friends, family, or a random ‘pal’ (Table 2). 43.4% of patients commented that the app would increase their motivation level to follow their medication regimens; 96.7% said the app was easy to use; and 70% said they were comfortable with video-chatting while taking their medications. Reasons for each of the rankings are noted on the right column.
Full table
Table 3 lists key themes and quotes that arose from patient interviews. Positive reviews were centered around the uniqueness of the app in incorporating a fun element to the otherwise mundane and cumbersome task of taking medications. Patients who were open to chatting with a random ‘pal’ liked the idea of being able to make new friends and creating a supportive community. They thought this feature would also aid in the exchange of information between patients, such as experiences with specific diseases, as well as side effects of medications.
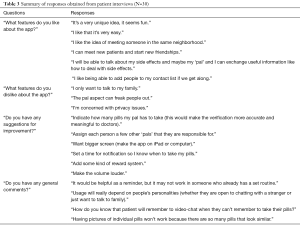
Full table
Negative reviews included hesitance to use the ‘pal’ feature due to unfamiliarity with the ‘pal’, concerns with privacy, and the difficulty of incorporating a new routine for patients with an established medication-taking routine.
Suggestions for improvement included increasing the accuracy of verification by adding the number of pills taken, having the app on devices with larger screens, having other modes of communication for situations where video-chat may be inconvenient, making the ‘pal’ feature more specific, and creating customizable notification systems.
A total of 10 cardiologists were interviewed to gain feedback on the Physician Calendar. The goal was to determine whether this would be helpful for clinicians, how it could improve patient care, and suggestions for further improvement. The list of questions asked and clinicians’ responses are presented in Table 4.

Full table
Clinicians stated that by using this calendar, they would be able to quickly detect non-adherence and immediately be able to help patients by addressing their root cause of medication non-adherence. Some clinicians noted that the calendar should display patient adherence for individual pills. This is due to the relative importance of certain medications in a patient’s regimen compared to others. For example, skipping a few doses of a blood pressure medication would rarely be fatal, but skipping a blood thinner or a diuretic for a few days could result in serious consequences. Thus, for patients with severe diseases, clinicians need to know precisely which medications the patient is non-adherent to; however, PillPal currently does not support pill-by-pill verification. Other clinicians did not see this as a fatal flaw of the app. While tracking individual pills is the most accurate, it risks making the app more cumbersome for patients to use. Instead, an overall adherence score for each patient since the last clinic visit would be useful as a jumping-off point in guiding the clinic conversation. If the adherence score is low, clinicians will know that they need to probe the patient with questions such as, “I see your score is a little low, is everything okay? Is there a specific medication you’re having trouble with? Did you experience side effects? Did you run out? Can I help clarify what your medications are for?”
Overall, the cardiologist surveys were valuable in understanding the usefulness of the calendar to clinicians and the ideal workflow when using the calendar during a patient’s clinic visit.
Discussion
This pilot study provided a proof-of-concept for leveraging social connections between patients to encourage better medication adherence. Close to half of patients stated that the social experience of video-chatting another person would increase their level of motivation in adhering to medication regimens. While the data obtained from this first prototype are promising, they elucidated many aspects of the app that can be improved.
Feedback on the ‘random pal’ versus family member connection aspect of the app were mixed, with some patients being open to video-calling new people every day, while others preferring to limit interactions within known family members or friends. This preference appeared to be highly dependent on the individual’s personality.
Some patients noted that the app was a good idea but may not work for them, as they already have a set routine for taking their medicines. Some did not see the need to make new friends as they already had a high level of social support from family members. Therefore, to gain substantial user base, it will be important to identify patients who are regularly non-adherent, who may not have a set medication routine, and are open to creating new social connections.
PillPal offers a novel approach to improving medication adherence, building upon the fundamental premise that people are social beings and that behavioral changes often come from a change in internal motivation. A higher degree of social support—patient connection with family members, friends, and other patients—has consistently been shown to enhance patients’ intrinsic motivation to engage in treatment and thereby improve adherence. From this study we were able to validate the idea that a video-chatting app can increase social support and motivation in patients to improve medication adherence.
Failure modes of the app include the decreased overall technological proficiency of the elderly population. However, the share of adults age 65 and up who own smartphones has been rising rapidly, from just 18% in 2013 to 42% in 2017, and is expected to continue increasing (10). Another risk is the violation of patient privacy and lack of a method to report abusive users. We plan to mitigate this risk by implementing methods to report and block users, as well as a remote-wipe function to delete unwanted accounts. Moreover, it is easy for patients to “game” the system and generate false positives, e.g., two users both agree to verify each other when neither has taken their medications. Currently, there is no way to address this problem; however, PillPal is an app designed for patients who inherently want to adhere but lack the social support or motivation to do so, thus we do not foresee this being a major barrier for our solution.
Though the app generally received positive reviews, insight gained from this study will be used to improve the app’s usability and likelihood of adoption. In making medication-taking a social experience, there was general hesitancy in meeting strangers over video-chat. Therefore, the ‘pal’ aspect of the app may need to undergo an improvement in conceptual design to improve this core feature of the app.
Acknowledgements
This work was supported with funding by the Johns Hopkins University Department of Biomedical Engineering, Center for Bioengineering Innovation & Design (CBID) and Youseph Yazdi, PhD, the Executive Director of CBID.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by the Johns Hopkins Institutional Review Board (No. IRB00122209). Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Brown MT, Bussell JK. Medication adherence: WHO cares? Mayo Clin Proc 2011;86:304-14. [Crossref] [PubMed]
- Iuga AO, McGuire MJ. Adherence and health care costs. Risk Manag Healthc Policy 2014;7:35-44. [PubMed]
- Sabate E. Adherence to long-term therapies: evidence for action. World Health Organization 2003. Available online: http://www.who.int/chp/knowledge/publications/adherence_report/en/
- Miller TA, DiMatteo MR. Importance of family/social support and impact on adherence to diabetic therapy. Diabetes Metab Syndr Obes 2013;6:421-6. [Crossref] [PubMed]
- Wu JR, Frazier SK, Rayens MK, et al. Medication adherence, social support, and event-free survival in patients with heart failure. Health Psychol 2013;32:637-46. [Crossref] [PubMed]
- DiMatteo MR. Social support and patient adherence to medical treatment: a meta-analysis. Health Psychol 2004;23:207-18. [Crossref] [PubMed]
- Persell SD, Osborn CY, Richard R, et al. Limited health literacy is a barrier to medication reconciliation in ambulatory care. J Gen Intern Med 2007;22:1523-6. [Crossref] [PubMed]
- Stirratt MJ, Dunbar-Jacob J, Crane HM, et al. Self-report measures of medication adherence behavior: recommendations on optimal use. Transl Behav Med 2015;5:470-82. [Crossref] [PubMed]
- Dayer L, Heldenbrand S, Anderson P, et al. Smartphone medication adherence apps: Potential benefits to patients and providers. J Am Pharm Assoc (2013) 2013;53:172-81. [Crossref] [PubMed]
- Anderson M, Perrin A. Tech adoption climbs among older adults. Pew Research Center, Internet & Technology 2017. Available online: http://www.pewinternet.org/2017/05/17/tech-adoption-climbs-among-older-adults/
Cite this article as: Fujita S, Pitaktong I, Steller GV, Dadfar V, Huang Q, Banerjee S, Guo R, Nguyen HT, Allen RH, Martin SS. Pilot study of a smartphone application designed to socially motivate cardiovascular disease patients to improve medication adherence. mHealth 2018;4:1.


