Behavioral health characteristics of a technology-enabled sample of Alzheimer’s caregivers with high caregiver burden
Introduction
A 2016 report from the Alzheimer’s Association indicated that 15 million Americans provide unpaid care for people with Alzheimer’s disease (AD). In 2015, these caregivers provided 18.1 billion hours of care valued at $221.3 billion (1). The amount of AD care provided by the informal sector will continue to increase with the aging of the population. About one-third of AD caregivers are themselves over the age of 65, and two-thirds live with the care recipient (1). Like the people they support, AD caregivers are often physically and emotionally vulnerable (2,3). If not properly supported, informal caregivers often burn out (4), leading the way for a shift in service provision to the formal healthcare sector. This shift has far-reaching implications for policy makers and other stakeholders because of the tremendous costs that are associated with receipt of formal health care services. In 2016, total payments for AD for people over the age of 65 were estimated at $236 billion (1).
Among the recommendations in a 2017 report from the National Alliance for Caregiving was a call to expand dementia caregiver access to long-term supports and services (5). It is against this backdrop that technological advances that have led to the development of technology-enhanced AD caregiver supports can be understood. These new technologies could eventually become part of a technology-enabled, caregiver-focused toolbox that addresses the widely-recogfnized need for more and better long-term supports for AD caregivers.
Telehealth, the provision of healthcare using telecommunications technology, is one such strategy that could help caregivers to remain healthy and viable in their caregiving roles. As part of a larger research program focusing on caregiver characteristics and home-based telemedical supports (6,7), this report focuses on a necessary first step in pursuit of this strategy: determining (I) whether a sample of technology-enabled caregivers can be identified and (II), if so, whether this sample shares the risk profiles characteristic of the broader caregiving population. We recruited a sample of AD caregivers and administered surveys that assessed caregiver burden, mental health, and sleep quality. This paper explores the demographic characteristics of this technology-enabled AD caregiver sample, as well as cross-sectional relationships among caregiver burden and several mental health measures. Our results provide insight into the feasibility of identifying caregivers who are in need of support, quantifying their level of caregiver burden, and identifying the types of supports they may need. This work also highlights the potentially-far reaching benefits of delivering tailored caregiver supports via mobile technology, a strategy that has been recognized and strongly supported by caregiver advocates (8).
Methods
The Health-eBrain Study is an ongoing effort focused on evaluating the impact of an AD caregiver support protocol delivered via smart phone on several outcomes including cognition, caregiver burden, anxiety, and depression1. The current study enrolled AD caregivers between the ages of 45–75 years who reported using a smart phone, the ability to speak and read English, and who had Internet access. AD caregivers were recruited through the outreach of partner organizations (Bright Focus Foundation, Geoffrey Beene Foundation Alzheimer’s Initiative, Us Against Alzheimer’s, and PCORI AD-PCPRN2) as well as the Health-eBrain study website. Once potential participants were directed to the study website, they were provided with a consent form which they signed electronically before moving onto data collection. The study protocol (#091614A) was approved by the AnthroTronix Institutional Review Board. This report focuses on cross-sectional data that were collected at the point of enrollment from all eligible AD caregivers.
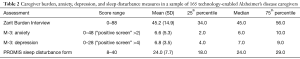
Demographic information, including age, gender, ethnicity, and education were collected. A series of variables describing caregiving history and patterns were also collected. These included how long the caregiver had been providing care, when the care recipient was diagnosed with AD, hours per week of care provision, relationship between the care provider and care recipient, whether the care provider lives with the care recipient and whether the care provider is also employed for wages outside of his/her caregiving role. Several instruments were then administered to caregivers to assess caregiver burden, sleep quality, depression and anxiety. The Zarit Burden Interview (ZBI) is a 22-item measure of caregiver burden that was developed for caregivers of dementia patients. It measures subjective burden associated with functional/behavioral impairments and the home care situation, and is scored on a scale from zero to 88 (9). The raw scores from this measure can be analyzed as a numeric variable, and they can also be categorized into four groups that reflect increasing caregiver burden (0–20: little or no burden; 21–40: mild to moderate burden; 41–60: moderate to severe burden, and 61–88: severe burden). The PROMIS Sleep Disturbance Short Form 8a assesses perception of sleep quality, sleep depth, and restoration associated with sleep via a normed score distribution with no established clinical categories (10). Instead, raw scores are converted to T-scores, with a raw score of 20 corresponding roughly to the population average. For this measure, we will analyze raw scores. The M3 collects information on symptoms of major depressive disorder, generalized anxiety disorder, panic disorder, social anxiety disorder, PTSD, OCD, and functional impairment (11). The instrument consists of eight questions, each with responses that are scored from zero (“not at all”) to four (“most of the time”). This instrument is used to screen for several mental health conditions, and is therefore highly relevant for use in mobile assessment of AD caregivers as an initial means to identify specific supports that may benefit these individuals.
Our analyses focused on understanding demographic characteristics of high-need, technology-enabled AD caregivers, cross-sectional associations between caregiver burden and specific aspects of caregiving history and patterns, as well as mental health as measured by the M3. To achieve these goals, we examined descriptive statistics of caregivers’ demographic profiles, including age, gender, ethnicity, education, and their relationship to the care recipient. We also examined hours of caregiving and duration of care provision. Finally, we conducted a series of correlation analyses to assess relationships between caregiver burden and depression, anxiety, and sleep disturbance.
Results
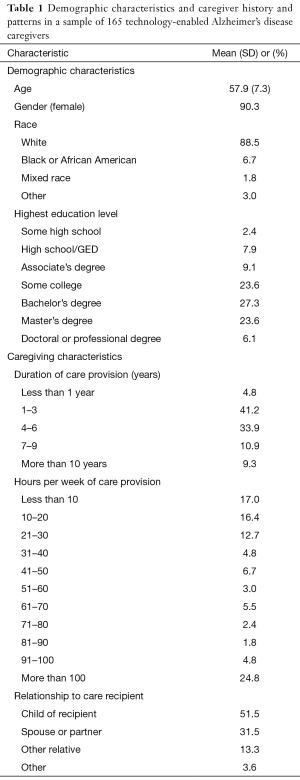
A total of 165 eligible caregivers registered on the Health-eBrain Study web portal and indicated that they provided care for someone with AD and owned a smart phone. The mean age of the sample was 57.9 years, and it consisted of predominantly female, White, English-speaking caregivers, half of whom had a college degree. About a third of the sample reported providing care for 4–6 years, 4.8% had been providing care for less than a year, and 9.3% had been caregivers for 10 years or more. There was also wide variation in the amount of time each week that care was provided. While 17% of the sample reported providing less than 10 hours of care each week, almost 25% reported providing more than 100 hours of weekly care. As expected, most caregivers in the sample described themselves as the adult child or spouse of the care recipient (Table 1).
Full table
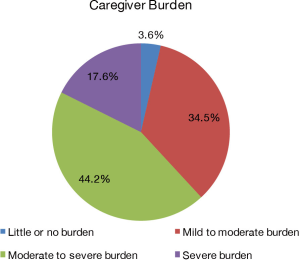
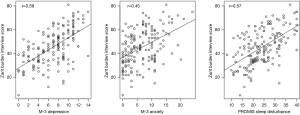
Table 2 provides descriptive statistics for scores on the ZBI, M3 depression and anxiety subscales, and the PROMIS sleep disturbance form. Examining these scores in terms of clinical categories, 64% of caregivers in the sample screened positive for both anxiety and depression on the M3 subscales, and more than 60% of the sample had either moderate or severe caregiver burden based on the ZBI (Figure 1). While no clinical categories for the PROMIS sleep disturbance form are established, approximately 25% of our sample scored greater than one standard deviation above the population average, suggesting relatively poor sleep quality. Figure 2 shows scatterplots (with trend lines fit by regression) illustrating the correlation between ZBI scores and depression (r=0.59, P<0.001) and anxiety scores (r=0.45, P<0.001) as measured by the M-3 and sleep disturbance (r=0.57, P<0.001) as measured by the PROMIS form. We present three separate analyses for ease of interpretation, but a full model of population behavior would likely need to account for the complex interdependencies between these behavioral outcomes [e.g., by modeling the mediating effect of mood disorders on sleep quality (12)].
Full table
Conclusions
Our results show that a sample of AD caregivers with Internet and smartphone access can be identified and enrolled online for research focused on delivery of caregiver supports using mobile technology. Further, the demographic and behavioral health characteristics align closely with those observed in the broader caregiving population. Consistent with previous findings, our caregiver sample was overwhelmingly female, and consisted mostly of the spouses and adult children of the person receiving care (1). However, previous work has suggested that 40% of caregivers have a college degree or higher level of education (13), while in our sample, 57% of caregivers had a bachelor’s degree or higher level of education. It is possible that because selection criteria for our study stipulated that caregivers needed to use both the Internet and smartphones, our sample was somewhat more highly educated than caregivers as a whole. However, differences in level of education between our sample and national statistics are more likely to be related to the relatively low age of our sample, and secular trends in educational attainment (14).
Fifty-one percent of the caregivers in our sample were providing care for a parent, a finding that is consistent with another sample in which 55% of caregivers were adult children caring for a parent (15). In our sample, more than 90% of caregivers were women, a proportion that is considerably higher than the two-thirds that has been reported elsewhere (1). It is possible that the higher proportion of women in our sample can be explained in part by a greater likelihood for women to seek novel approaches to securing caregiver support (such as the Health eBrain study protocol) in a manner that is consistent with women’s higher use of health care services compared to men (16). However, a meta-analysis of 229 studies of gender differences among caregivers found no differences between men and women in the use of either formal or informal supports (17).
A key goal of this report was to examine underlying assumptions concerning the feasibility of identifying and engaging AD caregivers in a manner that could lead to way to delivering tailored caregiver supports to this vulnerable population. Our results show that caregivers were willing to engage with an online platform that was linked to delivery of caregiver support to their mobile devices. This suggests that caregivers recognize the value of mobile devices as a potential source of support, a finding that is consistent with the agenda of advocacy organizations that encourage development and adoption of new technologies to ease caregiving burdens (8). Beyond the observation that caregivers were willing to engage in a protocol involving delivery of supports to their mobile devices, it is worth emphasizing that the data that were collected in our study allowed us to “risk stratify” caregivers in a manner that, in practice, could assist providers in tailoring services and supports to meet the needs of individual caregivers. We collected data on caregiver burden and observed that more than 60% of our sample had moderate or severe burden. The clinical relevance of this observation is linked to our screening data on depression, anxiety, and sleep patterns, all actionable mental health and behavioral conditions that require different interventions. Not unexpectedly, our data show that caregiver burden was significantly correlated with screening measures for anxiety and depression, indicating that tailored interventions that target individual caregiver needs could be developed and delivered to mobile devices based on this information.
Identifying AD caregivers with unmet needs, and collecting information that is needed to deliver tailored services and supports are among the first steps in demonstrating that mobile technology can be used to ease caregiver burden. As the size of the aging population continues to increase, so too does the cost of providing formal care for this growing segment of the population. Provision of informal care by family and other caregivers represents cost savings to both public and private insurers, and the economic value of informal caregiving will only continue to increase. Although the economic implications of informal caregiving are unambiguous, the most common reason–65%–that informal caregivers report that they provide this support is their desire to keep the care recipient at home (13). Thus, fully leveraging mobile technology as a means to deliver caregiver support is not only prudent from an economic point of view, it also helps caregivers achieve the primary goal that they have defined for themselves in their caregiving roles.
Acknowledgements
We are grateful to Rita Shewbridge and Marissa Lee for the provision of administrative support and data collection efforts.
Funding for this study (title: Health eBrain Study: Addressing Depression and Cognitive Function in Dementia Caregivers) was provided by the Bright Focus Foundation and the Geoffrey Beene Foundation Alzheimer’s Initiative.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study protocol (#091614A) was approved by the AnthroTronix Institutional Review Board. Once potential participants were directed to the study website, they were provided with a consent form which they signed electronically before moving onto data collection.
1The Health-eBrain Study is indexed on clinicaltrials.gov, and more information can be accessed at http://health-ebrainstudy.org.
2The Patient-Centered Outcomes Research Institute Alzheimer’s and Dementia Patient and Caregiver Powered Research Network (PCORI AD-PCPRN) is a coalition of 43 partner institutions.
References
- Alzheimer's Association. 2016 Alzheimer's disease facts and figures. Alzheimers Dement 2016;12:459-509. [Crossref] [PubMed]
- Schulz R, Martire LM. Family caregiving of persons with dementia: prevalence, health effects, and support strategies. Am J Geriatr Psychiatry 2004;12:240-9. [Crossref] [PubMed]
- Vitaliano PP, Zhang J, Scanlan JM. Is caregiving hazardous to one's physical health? A meta-analysis. Psychol Bull 2003;129:946-72. [Crossref] [PubMed]
- Takai M, Takahashi M, Iwamitsu Y, et al. The experience of burnout among home caregivers of patients with dementia: relations to depression and quality of life. Arch Gerontol Geriatr 2009;49:e1-5. [Crossref] [PubMed]
- National Alliance for Caregiving. Dementia caregiving in the US. 2017 research report accessed February 22, 2017. Available online: http://www.caregiving.org/wp-content/uploads/2017/02/DementiaCaregivingFINAL_WEB.pdf
- Lathan CE, Coffman I, Shewbridge R, et al. A Pilot to Investigate the Feasibility of Mobile Cognitive Assessment of elderly patients and caregivers in the home. J Geriatrics Palliative Care 2016;4:6.
- Lathan C, Wallace AS, Shewbridge R, et al. Cognitive Health Assessment and Establishment of a Virtual Cohort of Dementia Caregivers. Dement Geriatr Cogn Dis Extra 2016;6:98-107. [Crossref] [PubMed]
- Adler R, Mehta R. Catalyzing technology to support family caregiving. National Alliance for Caregiving 2014:1-8.
- Hébert R, Bravo G, Préville M. Reliability, validity and reference values of the Zarit Burden Interview for assessing informal caregivers of community-dwelling older persons with dementia. Can J Aging 2000;19:494-507. [Crossref]
- Yu L, Buysse DJ, Germain A, et al. Development of short forms from the PROMIS™ sleep disturbance and Sleep-Related Impairment item banks. Behav Sleep Med 2011;10:6-24. [Crossref] [PubMed]
- Gaynes BN, DeVeaugh-Geiss J, Weir S, et al. Feasibility and diagnostic validity of the M-3 checklist: a brief, self-rated screen for depressive, bipolar, anxiety, and post-traumatic stress disorders in primary care. Ann Fam Med 2010;8:160-9. [Crossref] [PubMed]
- Brummett BH, Babyak MA, Siegler IC, et al. Associations among perceptions of social support, negative affect, and quality of sleep in caregivers and noncaregivers. Health Psychol 2006;25:220-5. [Crossref] [PubMed]
- Alzheimer's Association. 2014 Alzheimer's disease facts and figures. Alzheimers Dement 2014;10:e47-92. [Crossref] [PubMed]
- Ryan CL, Bauman K. Educational attainment in the United States: 2015. 2016; United States Census Bureau research report. Available online: https://www.census.gov/content/dam/Census/library/publications/2016/demo/p20-578.pdf
- Fisher GG, Franks MM, Plassman BL, et al. Caring for individuals with dementia and cognitive impairment, not dementia: findings from the aging, demographics, and memory study. J Am Geriatr Soc 2011;59:488-94. [Crossref] [PubMed]
- Bertakis KD, Azari R, Helms LJ, et al. Gender differences in the utilization of health care services. J Fam Pract 2000;49:147-52. [PubMed]
- Pinquart M, Sörensen S. Gender differences in caregiver stressors, social resources, and health: an updated meta-analysis. J Gerontol B Psychol Sci Soc Sci 2006;61:33-45. [Crossref] [PubMed]
Cite this article as: Coffman I, Resnick HE, Lathan CE. Behavioral health characteristics of a technology-enabled sample of Alzheimer’s caregivers with high caregiver burden. mHealth 2017;3:36.


