mHealth based interventions for the assessment and treatment of psychotic disorders: a systematic review
Introduction
Globally, the relative burden of mental health disorders is on the rise in terms of prevalence, disability and mortality (1), with limited controlled data available to guide treatment choices for clinicians worldwide. Since the 1990s, electronic service delivery within healthcare has expanded significantly (2). This mode of service delivery initially received a number of titles such as ‘Telemedicine’, ‘Telehealth’ and ‘Telecare’. However, with the merging of different technologies, the whole area is becoming more encompassing and the term ‘eHealth’ has emerged.
One particular form of eHealth is mHealth (mobile Health), the Global Observatory for eHealth (GOe) defines mHealth or mobile health as ‘medical and public health practice supported by mobile devices, such as mobile phones, patient monitoring devices, personal digital assistants (PDAs), and other wireless devices’ (3). mHealth technologies utilise components and functionalities of mobile devices such as Short Messaging Service (SMS), General Packet Radio Service (GPRS), Bluetooth, Global Positioning Systems (GPS) and mobile connectivity (3 and 4 g) and smartphone applications more commonly known as mobile Apps. mHealth has been successfully used in delivering treatment modalities in a variety of settings, predominantly in High Income Countries (HICs). In recent years, there have been studies on the successful use of a variety of mHealth interventions for Severe Mental Illness (SMI). More recently, a number of apps for psychosis have been launched e.g.; TechCare, Actisist and ClinTouch (4-6).
Mental, Neurological, Substance use (MNS) disorders constitute 14% of the global burden of disease (7). Low resourced countries face greater challenges to overcoming this burden due to lack of resources and limited availability and access to mental health care (8). The treatment gap for MNS disorders is estimated to be over 75% in many LMICs, due to the inequitable and insufficient usage of resources (1). mHealth technologies may be a potentially beneficial avenue to bridging this large treatment gap, through improved access to self-management and self-help interventions utilising digital clinical technologies, which may also significantly assist in recovery from SMI such as psychosis.
Individuals with a diagnosis of psychosis may experience a number of symptoms, such as auditory hallucinations and delusional ideation (9). Research has suggested the prevalence of psychosis to be roughly 1% globally (10). Psychotic illnesses are usually preceded by a prodrome which can last anywhere from one to three years (11), with individuals experiencing a wide range of non-specific behavioural and psychological symptoms, and a deterioration in functioning (12). Interventions that prevent or delay transition to psychosis from the prodromal phase, may be clinically and economically important (13).
mHealth interventions have been used in the assessment and treatment of psychosis. A recent review by Alvarez-Jimenez et al. (14) highlighted a number of mobile interventions for psychosis. However the focus of the paper was in relation to web based and social media interventions and did not take into account mobile devices as defined above. Another review conducted by Kasckow et al. (15) also reported the feasibility of telephone, the internet and videoconferencing interventions. However, these reviews focused more on eHealth interventions which are in most cases dependant on an internet connection. Globally only 34.3% (16) of the global population have access to the internet whereas the International Telecommunication Union (ITU) estimates roughly 7 billion mobile phone subscriptions being held worldwide, with an estimated penetration of 96% of individuals having access to mobile phones globally (17). It can therefore be seen that mobile devices could be a potentially effective modality in providing health interventions, by bridging the gap for those individuals who do not have access to the internet in low resourced settings.
The aim of this review is to search the literature systematically for studies utilising different mHealth interventions for psychosis; to assess what kind of interventions have been used globally. We believe a synthesis of available information could lead to a better understanding of the feasibility and effectiveness of these techniques in the treatment and assessment of psychotic illnesses. The results may help develop similar approaches for use in other mental illnesses, to reduce the burden of mental health disorders globally.
Methods
Inclusion and exclusion criteria
We followed the Cochrane collaboration guidelines on conducting systematic reviews (18). The inclusion criteria for studies was based on the following criteria: (I) described the use of a mobile device intervention in patients who were suffering from psychosis (II) at least one outcome measure was the assessment and treatment of psychosis (III) was a controlled trial (randomised or quasi-randomised). Studies were excluded if they used internet or other technologies without utilising mobile devices such as smartphones and tablets.
Literature search
We searched the following databases; Embase, Medline, PsychINFO and Evidence Based Medicine Reviews. A number of keywords were searched in each of the databases from inception to May 2016; the search criteria was initially configured and deployed in Medline and the same search criteria was then extrapolated to other databases. The key words that were searched included; ‘mHealth’ ‘Mobile Health’ or ‘SMI’ or ‘Schizophrenia’ or ‘Schizo-Affective Disorder’ or ‘Intervention’ or ‘Assessment’ or ‘Treatment’. (Please see Supplementary for full search strategy). We also searched for relevant systematic reviews in the Cochrane Database of Systematic Reviews and the Cochrane Database of Abstracts of Reviews of Effects (DARE) and randomised controlled trials were searched in the Cochrane Central Trials Register (CENTRAL).
Assessment of methodological quality
The methodological quality of the included randomised controlled trials and clinical controlled trials were assessed using the list from the Cochrane Risk of Bias Tool (19), which included 4 domains comprising of 11 criteria which assess internal validity of the selected studies. The 4 domains that were examined and the criteria used are as follows: (I) selection bias; this domain looked at whether an adequate randomisation procedure was used, similarity in baseline data on the primary indicator and whether treatment allocation was concealed; (II) performance bias; this included blinding of patients to the intervention, whether intervention compliance was adequate, and whether health professionals/therapists were blinded to intervention groups (IG); (III) attrition bias; this domain looked at whether the study included an intention to treat analysis and whether the study had an acceptable level of dropout rate at baseline; (IV) detection bias this domain examined whether the study used similar or the same outcome measures across the study groups, and whether the outcome assessor was blinded to the study groups. Overall, the studies were scored independently by two of the researchers (NG & PSK) across each of the 4 domains, the studies were scored either with a ‘Yes’, ‘No’ or ‘Unclear’. Studies which scored more than 6 across each of the 4 domains were classed as high quality otherwise the remaining studies were classed as low quality. Any disagreements were discussed with senior researchers (SF, NH & JD) until a consensus was reached.
Data synthesis
The data was extracted from the databases and all abstracts were read by two of the research associates (NG & PSK). Those studies which met the inclusion criteria were then extracted by the reviewers using a standardised data extraction sheet. The following variables were extracted from the included studies; mobile Intervention used, type of study, outcome measures, duration, diagnostic criteria and results. Any disagreements were resolved through discussion with two investigators, (SF & NH) until consensus was gained. We had plans to conduct a meta-analysis, but in view of the nature of studies (see below), no meta-analysis was conducted.
Results
Characteristics of the included studies
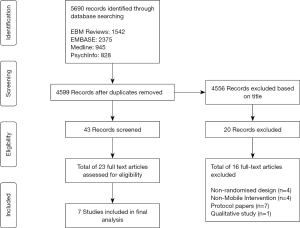
We found a total of 5,690 titles across the databases we searched, using our search strategy, from these, 43 studies were selected based on the title and abstract for further scrutiny. We selected 23 studies which were read full text, with sixteen studies being excluded (see Figure 1). Out of the excluded studies, four studies were excluded as they did not include a randomised controlled design, these included a study by Pijnenborg et al. (20) which investigated an SMS text message intervention for cognitive rehabilitation in schizophrenia. A study by Depp et al. (21) which looked at the mobile assessment of psychotic symptoms coupled with a low intensity intervention and Ben-Zeev et al. (22) who looked at retrospective multiple real-time/real-place assessments using a dual methods design, in individuals with schizophrenia and a non-clinical group. Another excluded study by Palmier-Claus et al. (5) investigated ambulatory assessment of psychotic symptoms. Other reasons for excluded studies are given in Figure 1.
The 7 included studies examined different parameters, one of the studies used an Experiential Sampling Methodology (ESM) which looked at monitoring symptoms real-time, one looked at medication adherence, two looked at cognitive impairments, one looked at social functioning, one looked at suicidal ideation in veterans with schizophrenia, one looked at mobile phone text message reminders and one examined relapse prevention and early warning signs. In view of the widely different interventions and outcome measures it was not possible to conduct a meta-analysis. Therefore we decided to give a descriptive account of the results.
Main findings
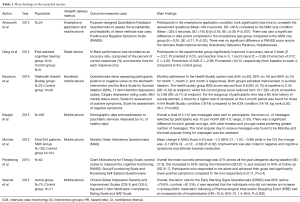
The characteristics of included studies are given in Table 1. The majority of studies were conducted across Europe and the United Sates with one in China; one was conducted in the UK, two in Spain, one in Finland, one in the Netherlands, one in China and one in the United States. Four of the studies were conducted in outpatient psychiatric settings, and three studies in an inpatient psychiatric unit. The total population across all studies was 1,105 (Mean =158, SD =197.20), with 637 males (Mean =91, SD =92.58) and 468 females (Mean =67, SD =107.27), the mean age of participants was 35.35 (SD =8.73). Five studies used a randomised controlled trial design, one used a prospective randomised open-label controlled trial and one was quasi-randomised. (Please see Table 1 for the main findings of the included studies).
Full table
mHealth interventions
The included studies used a number of differing delivery platforms. Ainsworth et al. (23) aimed to compare two differing mediums of receiving assessment notifications on a mobile phone device. The smartphone was loaded with a software application which provided questions to assess symptoms of psychosis. The system either utilised SMS text messages or smartphone based application to deliver the assessment questions. The study used a repeated measures crossover design which assigned the 24 study participants to either undergo the SMS condition first and then the smartphone application condition or vice versa. Both conditions used the same assessment questions which were based on the Positive and Negative Syndrome Scale (PANSS).
Another included study conducted by Dang et al. (24) examined the effects of an iPad assisted cognitive training programme on working memory in a group of male first-episode (FEP) schizophrenia patients. The training programme included user-friendly iPad games such as “Shanghai Mahjong”, “Little Ace and the Ten Commandments”, “Math vs. Brains” and “Brain Teaser Extreme. Participants engaged in the cognitive training for 60 minutes a day, 5 days a week. Assessments of working memory was conducted at baseline and follow up (week 4) through the N-Back task.
In addition, a total of four studies used a SMS based system as a delivery platform for the intervention (25-28). Pijnenborg et al. (25) investigated the efficacy of SMS messages to provide prompts to participants to achieve goals in their daily lives. These goals included, medication adherence, appointments, activities, attending training sessions and inhibition of undesired behaviours. Achievement of goals was based on an observer filling in a score sheet which indicated whether the goal had been achieved or not. The information technology aided relapse prevention in schizophrenia (ITAREPS) (26) used a multicentre randomised controlled trial design to examine the detection of early warning signs, through the use of SMS based alerts delivered using a mobile phone. The clinicians were provided alerts to increase pharmacological intervention if there was an increase in scores on the early warning signs questionnaire (EWSQ).
Kauppi et al. (27) utilised SMS based user defined prompts, relating to medication, follow up appointments and daily issues such as hygiene, physical exercise, symptom management and other supporting messages during discharge from a psychiatric inpatient setting. The frequency and timing of the SMS prompts were also defined by the user. A total of 562 participants enrolled in the study with participants’ receiving a mean total of 10 messages a month (SD 4.0; range, 2–25) over the 12-month study period. Montes et al. (28) used an SMS based mHealth delivery modality for medication adherence, a total of 254 participants took part in the study. Similarly, Montes et al. (28) used an SMS based mHealth delivery modality for medication adherence. In this study participant in the IG condition received daily reminders to take their medication.
In contrast, Kasckow et al. (29) assessed the feasibility of a telehealth monitoring intervention known as ‘Health Buddy’ for suicidal behaviour in a population of recently admitted inpatient US veterans aged 18 to 64, diagnosed with schizophrenia or schizoaffective disorder and recent suicidal ideation. The Health Buddy was a daily use system that facilitated symptom assessment and patient-staff communication during weekly visits for veterans following an intensive case monitoring (ICM) program. The study assessed, whether augmentation of ICM with the Health Buddy system would result in a significant reduction in suicidal ideation comparative to an ICM only group. This was reviewed using the beck scale for suicidal ideation (BSS).
Medication adherence
A total of 4 studies looked at medication adherence, with a combined sample size of n=921 participants, although the study by Kasckow et al. (29) investigated suicidal ideation in veterans with schizophrenia using the Health Buddy system. The daily monitoring of participants using the Health Buddy system included queries about medication adherence, which was described by participants as being effective in improving their medication adherence. In addition, the study by Pijnenborg et al. (25), reported that participants who responded to the alerts and achieved their goals had significantly lower positive symptoms compared to the non-responders (t=2.11, P=0.04). It was found that participants showed an increase in leisure activities and keeping to appointments with their health professionals. However, this was not the case for medication adherence and attendance at training sessions. These results differed from the study by Kauppi et al. (27), Kasckow et al. (29) and Montes et al. (28), who found improvements in medication adherence.
Kauppi et al. (27) utilised SMS based user defined prompts, relating to medication, follow up appointments and daily issues such as hygiene, physical exercise, symptom management and other supporting messages during discharge from a psychiatric inpatient setting. The frequency and timing of the SMS prompts were also defined by the user. A total of 562 participants enrolled in the study with participants’ receiving a mean total of 10 messages a month (SD 4.0; range, 2–25) over the 12-month study period. The results showed that the most preferable timing for the selected messages was at the beginning of the week, with participants less likely to prefer receiving messages on a weekend. The most selected messages related to medication (175 participants), follow up appointments (149 participants) and physical exercise (82 participants). Furthermore, In the Montes et al. (28) study participants who were in the IG condition significantly improved in medication adherence compared to those in the control group (CG) Mean change in score in IG was −1.0 (95% CI: −1.02, −0.98) while in the CG the change was −0.7 (95% CI: −0.72, −0.68) (P=0.02). In addition, the Montes et al. (28) reported that participants in the intervention group held more positive views about medications.
ESM
Only one of the studies utilised an ESM based methodology (23). The system would use randomly selected data points to obtain participant’s symptoms through either; smartphone notifications or SMS. This in effect constructed a daily record of the participant’s symptoms, enabling them to produce a day-to-day symptom profile. Participants in the smartphone application condition took significantly less time to complete the assessment questions (Mean =68.4 seconds, SD =39.5) compared to the SMS condition (Mean =325.5 seconds, SD =145.6) (β=0.78, SE =0.09, P<0.001). It was also reported that individuals completed significantly more notifications in the smartphone condition compared to the SMS only condition. There was also a significant difference (β=−0.25, SE =0.11, P=0.02) in data points completed in the smartphone application condition compared to the SMS group with smartphone application group completing 69% of entries, (mean =16.5), compared to the SMS condition (56% of entries, mean =13.5). There was no significant difference in PANSS scores across the domains, hallucinations anxiety, grandiosity, delusions, paranoia and hopelessness.
Cognitive functioning
The study by Dang et al. (24) examined cognitive functioning and used the N-Back task to assess cognitive functioning. In addition, the Wechsler Memory Scale-Revised (WMS-R) and full versions of the Wechsler Adult Intelligence Scale-Revised (WAIS-R) were used to assess participants at baseline. The results suggested that participants in the experimental group significantly improved in accuracy rate at 2-back (Z =−3.27, Pcorrected b 0.01), and reaction time in 0, 1 and 2-back (Z =−2.89, Pcorrected =0.012; Z =−2.60, Pcorrected =0.048; Z =−2.98, Pcorrected =0.012, respectively) from baseline to week 4, compared to those in the CG. In addition, Montes et al. (28) also looked at cognitive functioning and reported improvements in negative symptoms (Baseline =3.3 vs. 3 months =3.5) and cognitive symptoms (Baseline=3.3 vs. 3 months =3.5) P<0.05, in the IG compared to the CG group on the Severity of illness subscale of the Clinical Global Impression-Schizophrenia Scale (CGI-SCH-SI).
In contrast, the study by Pijnenborg et al. (25) looked at the efficacy of SMS based prompts to compensate for cognitive impairments in schizophrenia. This was done through SMS based prompts aimed at improving their everyday functioning through setting goals. Pijnenborg et al. (25) reported that the mean success percentage was 47% across all the goal categories during baseline (SD 27.9), this increased to 62% during the intervention (SD 20.1), and reduced to 40% at follow-up (SD 31.7).
Engagement with mHealth technology
The Kasckow et al. (29) study looked at monthly adherence to the Health Buddy system which was reported to be 83% (n=20), 92% (n=19) and 89% (n=15) for month 1, month 2, and month 3 respectively. Monthly adherence rates were calculated, by adding the number of days participants completed the questions divided by the number of days the participants were in the study that month. Both groups were reported to have shown improvement in suicidal ideation. The health buddy group BSS score reduced from 9.8 (SD =6.15) at baseline to 2.44 (SD =5.52) at endpoint, whilst the CG score reduced from 10.7 (SD =8.24) at baseline to 2.88 (SD =6.71) at endpoint. No difference in groups was found when examining duration to remission (defined as having a BSS score =0), however for the subgroup of participants with a life time history of suicide attempt, a trend for a higher rate of remission at 3 months was reported for those in the Health Buddy condition (16/18), compared to those in the ICM condition (14/19; log rank=2.82; df=1; P=0.093). No significant differences were detected between groups in scores on Calgary Depression Rating Scale, Hamilton Depression Rating Scale and Scale for Positive Symptoms and Scale for Negative Symptoms were included. However, in contrast Spaniel et al. (26) reported, that despite the fact that over the study period 17,082 SMS messages were sent by participants, it was reported that the study was largely unsuccessful, due to poor adherence by investigators to the protocol. They reported that only 39% of participants received an increase in antipsychotic medication in response to increased scores of the EWSQ.
Feasibility and acceptability
One of the main results of the included studies was the feasibility and acceptability of the mHealth interventions. Montes et al. (28) concluded that due to the ease of implementation, using mobile phones to prompt medication was feasible and acceptable. In addition, the Ainsworth et al. (23) study reported that mobile phones and smartphones were acceptable forms of technology. However there was shown to be a greater preference by participants to a smartphone application compared to a mobile phone. It was reported that participants took longer to complete each entry in the SMS condition (325.5 seconds, SD 145.6) compared to the smartphone application condition (68.4 seconds, SD 39.5). Overall 67% of participants preferred using the smartphone application compared to 13% who preferred SMS, 21% of individuals had no preference on the delivery method. Furthermore, it was reported that 71% of participants found using the smartphone application easier than the SMS delivery modality, 17% found the SMS condition to be easier and 13% had no preference (23).
The studies that used mobile phones were primarily used for the sending and receiving of SMS messages, these mobile devices had basic functionality such as voice calling, gaming, alarm, SMS and vibrate alerts (25,26,28). These studies also reported positive evaluations of using mobile phone based interventions. Pijnenborg et al. (25), found that the 70% of participants viewed the SMS intervention as positive, 20% were neutral and 10% held negative views. In addition, Pijnenborg et al. (25) reported that 41% of the participants found the intervention effective, 33% were neutral and 26% evaluated the intervention as ineffective. However, in contrast, Spaniel et al. (26) reported that feasibility could only be gauged once there had been acceptance of computerised methods and a change in clinical thinking.
In addition, feasibility of the Health Buddy system was examined over a 3-month period, with 20 of the 25 participants able to set up the Health Buddy system. Kasckow et al. (29). Of the 25 participants, it was reported that 4 individuals required some assistance to help with setting up the health buddy system. A number of reasons were reported for the 5 participants who did not set up the device, such as permission from landlord, substance misuse, cognitive impairment, phone company debt and transportation problems. In addition, Kauppi et al. (27) reported that participants preferred messages at the beginning of the week. It was suggested that individuals preferred messages early in the morning and in accordance to a working week format, running through Monday to Friday.
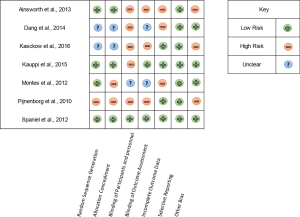
Risk of bias assessment
We used the Cochrane collaboration risk of bias instrument (19) to measure the risk of bias in the assessment of quality of trial reports, which is shown in Figure 2. Only one study had low risk of bias (26). All studies included were randomised trials however one was a qausi-randomised trial (25). Three of the studies described an appropriate method to generate the sequence of randomisation or gave the details, however the method used in the Pijnenborg et al. (25) was scored as high risk. All studies gave the details of withdrawal and drop outs. Ainsworth et al. (23) did not report the PANSS outcome measures highlighting a risk of bias when reporting data on outcomes used in their trial. The study by Dang et al. (24) indicated that the methods of the study were described in an earlier paper Lu et al. (30), however it was unclear as to what methods of randomisation and allocation to treatment arm were employed highlighting a risk of bias.
Discussion
The present systematic review is the first to look at mobile device interventions for the treatment and assessment of psychosis, with a focus on how future research can inform the use of mHealth technologies to increase access to treatments for SMI such as psychosis globally. Previous reviews have focused on telehealth, web based and internet interventions (14,15). However, these reviews investigated an array of differing delivery modalities such as the internet and telephone based land lines. Considering the increasing access to mobile devices globally, mHealth may potentially increase access to appropriate mental health care.
In view of the limited literature on the subject, the findings of this review can only help to comment on feasibility and acceptability of the mHealth interventions. Most studies found that mobile based interventions were feasible. Overall, it appears that the strongest evidence found, was related to mHealth technologies for medication adherence. Kauppi et al. (27) and Montes et al. (28) found that using mobile phones to prompt medication was feasible and acceptable. Similarly, Kasckow et al. (29) reported no significant difference in the clinical measures between the groups, however qualitative analysis of end-point surveys revealed a mainly positive response from participants in the Health Buddy condition with participants describing the program as effective in relation to improvement in medication adherence, and reduction in symptoms of anxiety and depression
The included studies reported a variety of outcomes. These included treatment adherence (28), social functioning (25), mobile text message preferences for people on antipsychotics (27), experiential sampling (23), cognitive impairment (24) relapse prevention (26) and suicidal ideation (29). This combined with limited literature on the subject means that it is not possible to have any definitive findings on the effectiveness of mHealth based interventions in improving these outcomes. There was an increase in medication adherence; Montes et al. (28) and Pijnenborg et al. (25) reported improvement in social functioning. This is consistent with literature in other branches of medicine (31), where mobile devices have successfully been used to improve adherence.
The mobile phones were primarily used for the sending and receiving of SMS messages. (25,26,28). These studies also reported positive evaluations of using mobile phone based interventions. Pijnenborg et al. (25), found that the 70% of participants viewed the SMS intervention as positive and only 10% held negative views Pijnenborg et al. (25). These findings are important and demonstrate that even the simple mobile devices can be used for interventions using functions such as SMS alerts, voice calling or alarms. This is relevant for low resourced settings, where large populations may have access to mobile devices with basic functionality.
However, it must be noted that, delivery of assessment questions in the Ainsworth et al. (23) study utilised either a mobile App or SMS text messages. It was reported that participants took longer to complete each entry in the SMS condition compared to the smartphone application condition. Overall 67% of participants preferred using the smartphone application compared to 13% who preferred SMS. This may suggest factors such as usability and user experience may be key factors in ensuring a user-friendly medium to deliver mHealth intervention, which goes beyond basic SMS messaging.
An innovative use of mHealth is the real-time assessment psychosis using an ESM methodology which was conducted by Ainsworth et al. (23). The study was based on the mHealth interventions engaging with participants in real-time. Research, in the real-time assessment of psychosis has been conducted by Myin-Germeys et al. (32) who described the method as ESM. The method looks at the differing moods, thoughts and psychotic symptoms of individuals which occur in their day to day lives. The method is used to construct an understanding of individual’s psychotic symptoms with a view to understanding the aetiological underpinnings of psychosis in the real-world context (33). Methods such as experiential sampling provide greater insight into SMI’s, constructing a picture of individual’s experiences of psychosis in day-to-day life. These uses, however, need to be evaluated in larger well-designed studies.
Limitations
The major limitation of the present review is that we were only able to identify 7 studies with relatively smaller sample sizes. It is unlikely that we missed any studies as we used a comprehensive search strategy. However, the limited literature shows that it is possible to design and conduct studies using mHealth interventions for improving treatment adherence, monitoring symptoms, and social functioning. Although this data is useful in providing evidence for the proof of concept of the potential benefits and applicability of mHealth for psychosis, this has not been properly evaluated. Furthermore, we were unable to find studies which looked at both the assessment and treatment of psychosis, using a randomised controlled trial design. This is important as interventions which can provide assessment and treatment for psychosis in real time such as the Depp et al. (21) study can be hugely beneficial to individuals with SMI particularly in low resourced settings.
Implications
The utility of mHealth has been shown in a number of Non-Communicable disorders globally. For example, Piette et al. (34) reported that mobile technologies can be used effectively in self-management of hypertensive patients to improve outcomes. Tran et al. (35), investigated teleconsultation with a software-enabled mobile telephone for common skin diseases by a dermatologist, it was found that mobile technology enabled greater access to dermatological expertise where access is limited. It may be possible to employ these methodologies for providing teleconsultations with mental health professionals, in areas where there is limited access to specialist mental health care. This potentially may be of huge benefit to those individuals who live in remote or rural areas and areas of high deprivation. Similarly, it may be possible to employ the cheap and widespread use of SMS messages for public health interventions such as reducing stigma associated with psychosis.
Search strategy
- random$ or control or controlled or trial or condition or assigned or groups
- exp schizophrenia/ or exp psychosis/ (psychotic or schizo$ or psychos$ or psychoses) or ((chronic$ or sever$) adj5 mental$ adj5 (ill$ or disorder$)) or exp psychiatric treatment/ or exp therapy/ or exp therapy/ or exp sociotherapy/ or exp clinical study/
- (intervention or psychotherapy or rehabilitation or training or therapy) or ((psychological or psychosocial or psychiat$ or clinical) adj5 (intervention or therap$ or rehabilitation or remediat$ or training or clinical or care)) or ((cognitive or behav$ or family or focused or psycho$ or social$ or education$ or skill$) adj5 (intervention or therap$ or rehabilitation or remediat$ or training))
- smartphone$ OR smart phone$ OR (window? adj3 phone) OR (window? adj3 mobile) OR nokia OR palm OS OR symbian OR iphone OR ipad OR iPod touch$ OR m health OR mhealth OR PDA OR personal digital assistant? OR android OR blackberr$ cellular phone [MeSH] OR phone$ OR telephone$ app OR apps OR application? OR software OR twitter OR facebook OR telemedicine OR tele medicine OR telehealth OR tele health OR ehealth OR computerised intervention$ OR computerized intervention$ OR e health OR e mail$ OR email$ OR Electronic mail OR health technolog$ OR intranet?
Acknowledgements
The authors wish to thank Miv Riley and Yaseen Edros, for their support in preparing the manuscript. NG gratefully acknowledges the support and funding of his PhD Studentship with the NIHR Collaboration for Leadership in Applied Health Research and Care (CLAHRC) North West Coast, UK.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Whiteford HA, Degenhardt L, Rehm J, et al. Global burden of disease attributable to mental and substance use disorders: findings from the Global Burden of Disease Study 2010. Lancet 2013;382:1575-86. [Crossref] [PubMed]
- Oh H, Rizo C, Enkin M, et al. What Is eHealth (3): A Systematic Review of Published Definitions. J Med Internet Res 2005;7:e1. [PubMed]
- Kay M, Santos J, Takane M. mHealth: New horizons for health through mobile technologies. World Health Organization 2011;64:7:66-71.
- Gire N, Chaudhry I B, Naeem F, et al. TechCare: mobile-assessment and therapy for psychosis: An intervention for clients within the early intervention service. SAGE Open Med 2016;4:2050312116669613. [PubMed]
- Palmier-Claus JE, Ainsworth J, Machin M, et al. The feasibility and validity of ambulatory self-report of psychotic symptoms using a smartphone software application. BMC Psychiatry 2012;12:172. [Crossref] [PubMed]
- Bucci S, Barrowclough C, Ainsworth J, et al. Using mobile technology to deliver a cognitive behaviour therapy-informed intervention in early psychosis (Actissist): study protocol for a randomised controlled trial. Trials 2015;16:404. [Crossref] [PubMed]
- Collins PY, Patel V, Joestl SS, et al. Grand challenges in global mental health. Nature 2011;475:27-30. [Crossref] [PubMed]
- Arjadi R, Nauta MH, Chowdhary N, et al. A systematic review of online interventions for mental health in low and middle income countries: a neglected field. Glob Ment Health (Camb) 2015;2:e12. [Crossref] [PubMed]
- van Os J, Linscott RJ, Myin-Germeys I, et al. A systematic review and meta-analysis of the psychosis continuum: evidence for a psychosis proneness-persistence-impairment model of psychotic disorder. Psychol Med 2009;39:179-95. [Crossref] [PubMed]
- Walker ER, McGee RE, Druss BG. Mortality in mental disorders and global disease burden implications: a systematic review and meta-analysis. JAMA Psychiatry 2015;72:334-41. [Crossref] [PubMed]
- McGlashan TH. Commentary: Progress, issues, and implications of prodromal research: an inside view. Schizophr Bull 2003;29:851-8. [Crossref] [PubMed]
- Ruhrmann S, Schultze-Lutter F, Salokangas RK, et al. Prediction of psychosis in adolescents and young adults at high risk: results from the prospective European prediction of psychosis study. Arch Gen Psychiatr 2010;67:241-51. [Crossref] [PubMed]
- Stafford MR, Jackson H, Mayo-Wilson E, et al. Early interventions to prevent psychosis: systematic review and meta-analysis. BMJ 2013;346:f185. [Crossref] [PubMed]
- Alvarez-Jimenez M, Alcazar-Corcoles MA, Gonzalez-Blanch C, et al. Online, social media and mobile technologies for psychosis treatment: a systematic review on novel user-led interventions. Schizophr Res 2014;156:96-106. [Crossref] [PubMed]
- Kasckow J, Felmet K, Appelt C, et al. Telepsychiatry in the assessment and treatment of schizophrenia. Clin Schizophr Relat Psychoses 2014;8:21-27A. [Crossref] [PubMed]
- Internet World Stats. Internet usage statistics - The internet big picture 2015, Available online: http://www.internetworldstats.com/stats.htm. Accessed on 8th July, 2017.
- International Telecommunication Union (ITU) (2014). ICT Facts and Figures 2014, Available online: http://www.itu.int/en/ITU-D/Statistics/Documents/facts/ICTFactsFigures2014-e.pdf. Accessed on 8th July, 2017.
- Higgins JP, Green S, editors. Cochrane handbook for systematic reviews of interventions. John Wiley & Sons; 2011.
- Higgins JP, Altman DG, Gøtzsche PC, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 2011;18;343:d5928.
- Pijnenborg GH, Withaar FK, Evans JJ, et al. SMS text messages as a prosthetic aid in the cognitive rehabilitation of schizophrenia. Rehabil Psychol 2007;52:236-40. [Crossref]
- Depp CA, Mausbach B, Granholm E, et al. Mobile interventions for severe mental illness: design and preliminary data from three approaches. J Nerv Ment Dis 2010;198:715-21. [Crossref] [PubMed]
- Ben-Zeev D, McHugo GJ, Xie H, et al. Comparing retrospective reports to real-time/real-place mobile assessments in individuals with schizophrenia and a nonclinical comparison group. Schizophr Bull 2012;38:396-404. [Crossref] [PubMed]
- Ainsworth J, Palmier-Claus JE, Machin M, et al. A comparison of two delivery modalities of a mobile phone-based assessment for serious mental illness: native smartphone application vs text-messaging only implementations. J Med Internet Res 2013;15:e60. [Crossref] [PubMed]
- Dang J, Zhang J, Guo Z, et al. A pilot study of iPad-assisted cognitive training for schizophrenia. Arch Psychiatr Nurs 2014;28:197-9. [Crossref] [PubMed]
- Pijnenborg GH, Withaar FK, Brouwer WH, et al. The efficacy of SMS text messages to compensate for the effects of cognitive impairments in schizophrenia. Br J Clin Psychol 2010;49:259-74. [Crossref] [PubMed]
- Španiel F, Vohlídka P, Hrdlička J, et al. ITAREPS: information technology aided relapse prevention programme in schizophrenia. Schizophr Res 2008;98:312-7. [Crossref] [PubMed]
- Kauppi K, Kannisto KA, Hätönen H, et al. Mobile phone text message reminders: measuring preferences of people with antipsychotic medication. Schizophr Res 2015;168:514-22. [Crossref] [PubMed]
- Montes JM, Medina E, Gomez-Beneyto M, et al. A short message service (SMS)-based strategy for enhancing adherence to antipsychotic medication in schizophrenia. Psychiatry Res 2012;200:89-95. [Crossref] [PubMed]
- Kasckow J, Zickmund S, Gurklis J, et al. Using telehealth to augment an intensive case monitoring program in veterans with schizophrenia and suicidal ideation: A pilot trial. Psychiatry Res 2016;239:111-6. [Crossref] [PubMed]
- Lu W, Zhang C, Yi Z, et al. Association between BDNF Val66Met polymorphism and cognitive performance in antipsychotic-naive patients with schizophrenia. J Mol Neurosci 2012;47:505-10. [Crossref] [PubMed]
- Yellowlees P. Trends in e-Health–Technological Advances that will Impact on Diagnosis and Treatment. Business Briefing: Global Healthcare, 2003;1-4.
- Myin-Germeys I, Oorschot M, Collip D, et al. Experience sampling research in psychopathology: opening the black box of daily life. Psychol Med 2009;39:1533-47. [Crossref] [PubMed]
- Myin-Germeys I, Peeters F, Havermans R, et al. Emotional reactivity to daily life stress in psychosis and affective disorder: an experience sampling study. Acta Psychiatr Scand 2003;107:124-31. [Crossref] [PubMed]
- Piette JD, Datwani H, Gaudioso S, et al. Hypertension management using mobile technology and home blood pressure monitoring: results of a randomized trial in two low/middle-income countries. Telemed J E Health 2012;18:613-20. [Crossref] [PubMed]
- Tran K, Ayad M, Weinberg J, et al. Mobile teledermatology in the developing world: implications of a feasibility study on 30 Egyptian patients with common skin diseases. J Am Acad Dermatol 2011;64:302-9. [Crossref] [PubMed]
Cite this article as: Gire N, Farooq S, Naeem F, Duxbury J, McKeown M, Kundi PS, Chaudhry IB, Husain N. mHealth based interventions for the assessment and treatment of psychotic disorders: a systematic review. mHealth 2017;3:33.