A systematic review of studies of web portals for patients with diabetes mellitus
Background
Diabetes affects over 29 million Americans and is the sixth leading cause of death (1,2). Diabetes is the leading cause of kidney failure, lower-limb amputations, and blindness in adults (2). In 2012, the total economic cost of diabetes in the U.S. was between $245 billion and $322 billion (3). Diabetes accounts for over 20% of health care spending. Although good glycemic control is associated with improved health outcomes and lower morbidity and premature mortality, almost half of patients with type 2 diabetes do not meet recommended targets for glycemic control, blood pressure control, or low density lipoprotein (LDL) cholesterol control (4). Many patients with type 2 diabetes cared for in the community do not meet recommended treatment goals (5,6).
Type 2 diabetes requires effective patient-provider communication and patient self-management to manage side effects, monitor blood test results, and screen for potential complications (7). Studies have shown that increasing patients’ knowledge about their risk factors can lead to improved clinical outcomes (8,9). Moreover, evidence shows that fostering a collaborative relationship between patients and their health care providers can also improve clinical outcomes (10,11).
To improve diabetes care and health outcomes, there has been increasing interest by care providers in utilizing information technology to support patient-provider communication and patient self-management. Patient portals provide health care information that is linked to a patient’s electronic medical record (EMR) (12,13). Patients are able to view their health care information such as medications, laboratory test results, doctor visits, discharge summaries, and results of diagnostic tests (14,15). Many patient portals also allow patients with diabetes and other chronic conditions to request refills of prescription medications, schedule appointments, and exchange e-mail with their health care provider (12).
The goal of the current article was to review the evidence on patient web portals for diabetes mellitus including patient web portals tethered to EMRs and web portals developed specifically for patients with diabetes.
Methods
This review is based upon PubMed bibliographic searches and appropriate search terms. Articles published in English from 1993 through February 2017 were identified using Boolean algebra commands and MeSH search terms: (web portal or patient web portal) and diabetes. The references of review articles were also reviewed (12,13,16,17). Information obtained from the bibliographic searches (information presented in abstract, key words, and study design) was used to determine whether to retain each identified article. Only studies with a randomized controlled trial, retrospective cohort, or cross-sectional study design were included.
A total of 94 articles were identified. After screening the full texts or abstracts of the 94 articles and reviewing review articles (12,13,16,17), 12 studies met the eligibility criteria.
Results
Of the 12 studies identified in this review, three had a cross-sectional design, one employed mixed-methods, one had a matched-control design, three had a retrospective cohort design, and 5 were randomized controlled trials. Six of the studies examined web portals tethered to EMRs and six were web portals developed specifically for diabetes patients.
Studies of web portals tethered to EMRs and used for diabetes management are summarized in Table 1. None had a randomized controlled trial design. Sarkar et al. (15) examined web portal use by adult diabetics who were included in the Kaiser Permanente Northern California Diabetes Registry. Among 14,102 participants, 6,099 (62%) had a limitation in health literacy. A total of 5,671 respondents (40%) registered for the web portal. Those with lower health literacy were more likely to not sign on to the patient portal [adjusted odds ratio (OR) =1.7; 95% CI: 1.4–1.9] than those who did not have a health literacy limitation. Wade-Vuturo et al. (18) examined patient web portal use by 54 adults with type 2 diabetes seen at a Nashville, Tennessee hospital. Secure messaging between patient and their health care provider was positively associated with patients’ glycemic control (P=0.04). In a retrospective cohort study of patients registered for the U.S. Department of Veteran’s Affairs My HealtheVet patient web portal, Shimada et al. (7) evaluated the use of web-based prescription refill, secure messaging and laboratory tests used in the management of type 2 diabetes. Patients with elevated hemoglobin A1c (HbA1c) at baseline who used secure messaging were more likely than those who did not use secure messaging to achieve glycemic control after age and sex were controlled for [OR =1.24; 95% confidence interval (CI): 1.14–1.34]. Patients with elevated blood pressure at baseline who used My HealtheVet to refill prescription medications were more likely than nonusers to achieve blood pressure control at follow-up (OR =1.08; 95% CI: 1.02–1.14). Studies of Group Health Cooperative diabetic patients found positive associations between the use of secure messaging and improvements in HgbA1c testing and glycemic control (19,20). Positive associations between portal use and improvements in cholesterol were also observed among Kaiser Permanente patients with diabetes or hypertension in Southern California (21). Secure patient-physician messaging was associated with an improvement in performance (P<0.0001) on HbA1c screening and control, LDL-C screening, LDL-C control, retinopathy screening, and nephropathy screening of 2.4–6.5%. Tenforde et al. (22) examined use of electronic personal health records by adult patients with diabetes who were treated at the Cleveland Clinic (n=10,746). Compared to non-users, personal health record users had improved diabetes quality measures. The adjusted OR of HbA1c testing was 2.06 (P<0.01).
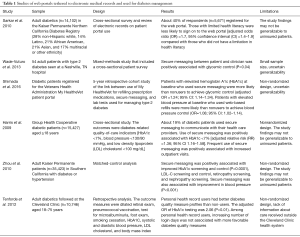
Full table
Studies of web portals developed specifically for patients with diabetes are summarized in Table 2. Grant et al. (23) conducted a 12-month cluster randomized controlled trial of a personal health record linked to the patient’s EMR, which enabled patients to access and read guidelines, review their lab results and medication lists, write comments to the EMR, and edit their medication lists. The primary outcomes were changes from baseline in HbA1c, blood pressure, and LDL cholesterol. More patients in the intervention group had their diabetes treatment regimens adjusted compared with controls (53% vs. 15%, P<0.001). However, there were no significant differences in risk factor control between study groups (P=0.053). Ralston et al. (24) conducted a randomized controlled trial that compared usual care plus Living with Diabetes program Web-based care management (patient access to EMR, secure e-mail with providers, feedback on blood glucose readings, an online diary for physical activity and nutrition, and an educational site) vs. usual care. On average, HbA1c levels declined by 0.7% (95% CI: 0.2–1.3) among patients in the intervention arm compared with the usual care group. McCarrier et al. (25) conducted a 12-month pilot randomized controlled trial of usual care plus Web-based collaborative care (Living with Diabetes program) vs. usual care alone. A non-significant decrease in average HbA1c was observed in the intervention group compared to the usual care group (−0.48; 95% CI: −1.22 to 0.27, P=0.160). Tang et al. (26) conducted a 12-month randomized controlled trial of an online diabetes management system that included home glucometer readings, nutrition and exercise logs, secure messaging with the patient’s providers, comprehensive patient-specific diabetes status report, advice and medication management from a nurse care manager and dietitian, and brief educational videos. Compared with usual care patients, the intervention group patients had reduced HbA1c at 6 months (−1.32% vs. −0.66%, P<0.001). No significant differences were observed at 12 months (−1.14% vs. −0.95%, P=0.133). In a retrospective cohort study, Lau et al. (27) found that, compared to patient web portal non-users, a higher proportion of users achieved HbA1c <7% at follow-up (56% vs. 32%, P<0.031). Tutino et al. (28) conducted a randomized controlled trial comparing web portals for diabetic patients alone vs. patient web portal plus nurse-coordinated follow-up visits. The primary outcomes was proportion of patients achieving ≥2 treatment targets (GbA1c <7%, blood pressure <130/80 mmHg, and LDL cholesterol <2.6 mmol/L). The proportion of participants attaining >2 treatment targets increased in both groups and there similar absolute reductions in HbA1c and LDL cholesterol, with no between-group difference.
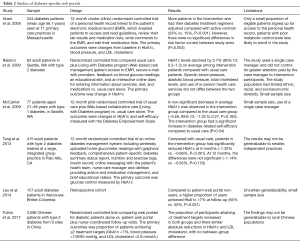
Full table
Discussion
Although results-to-date have been mixed, this review suggests that secure messaging between adult diabetic patients and their clinician is associated with improved glycemic control. Improvements in LDL cholesterol and blood pressure have also been observed in some studies of web portals used by patients with diabetes and hypertension (7). The specific portal features that may impact quality of care or improve glycemic control (e.g., patient-provider secure messaging, online access to lab test results or instructions, other patient supports) has not been clearly distinguished by studies completed to date. Secure messaging may facilitate coordination of diabetes care and make it easier for providers to refer patients to related services such as weight loss programs and advice from a dietician (7).
A further issue is that results from observational studies indicate that many diabetic patients do not take advantage of web portal features such as secure messaging, when offered, perhaps because of a lack of internet access or to a lack of experience in navigating web portal resources (18). Patient concerns about confidentiality may also play a role. Because observational studies are subject to selection bias and uncontrolled confounding, results from retrospective cohort studies do not establish that diabetic patient use of web portals has a positive effect on glycemic control. Although results from randomized controlled trials provide stronger evidence of the efficacy of web portal use in improving glycemic control among diabetic patients, only 5 trials have been reported and, of these, 2 were pilot trials with a small sample size. In addition, results from the randomized controlled trials have been mixed (Table 2).
With respect to limitations of this review, not all eligible published studies may have been identified by the bibliographic search process. We minimized this potential source of bias by reviewing the references of review articles.
Limited health literacy is relatively common among patients with type 2 diabetes and is likely to contribute to poorer diabetes outcomes (15,29-31). Studies indicate that patients with lower health literacy are less likely to use web portals to help manage a chronic illness (14,15). Patients with lower health literacy or computer literacy may have difficulty learning how to use a web portal or they may have difficulty navigating a portal. This may represent a contributing factor that compromises exploring the true impact and valid effects of patient portal use and improvement of diabetes management. Educational outreach efforts for potential web portal users may be helpful in overcoming these perceived barriers.
In summary, studies suggest that secure messaging between adult diabetic patients and their clinician is associated with improved glycemic control, but negative findings have also been reported and the causality of this association is uncertain. The number of randomized controlled trials that have examined the efficacy of web portal use in improving glycemic control among diabetics is still small. Additional research is needed to identify specific portal design features and patient demographic characteristics that may impact quality of care and improvement in specific and comprehensive elements of diabetes care.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Disclaimer: The contents do not represent the views of the U.S. Department of Veterans Affairs or the U.S. Government.
References
- CDC. National Center for Health Statistics. Leading causes of death. Available online: https://www.cdc.gov/nchs/fastats/leading-causes-of-death.htm [accessed February 24, 2017].
- CDC. Diabetes. Available online: [accessed February 24, 2017].https://www.cdc.gov/chronicdisease/resources/publications/aag/diabetes.htm
- American Diabetes Association. Economic costs of diabetes in the U.S. in 2012. Diabetes Care 2013;36:1033-46. [Crossref] [PubMed]
- Ali MK, Bullard KM, Saaddine JB, et al. Achievements of goals in U.S. diabetes care, 1999-2010. N Engl J Med 2013;368:1613-24. [Crossref] [PubMed]
- Saydah SH, Fradkin J, Cowie CC. Poor control of risk factors for vascular disease among adjults with previously diagnosed diabetes. JAMA 2004;291:335-42. [Crossref] [PubMed]
- Gaede P, Vedel P, Larsen N, et al. Multifactorial intervention and cardiovascular disease in patients with type 2 diabetes. N Engl J Med 2003;348:383-93. [Crossref] [PubMed]
- Shimada SL, Allison JJ, Rosen AK, et al. Sustained use of patient portal features and improvements in diabetes physiological measures. J Med Internet Res 2016;18:e179. [Crossref] [PubMed]
- Heisler M, Piette JD, Spencer M, et al. The relationship between knowledge of recent HbA1c values and diabetes care understanding and self-management. Diabetes Care 2005;28:816-22. [Crossref] [PubMed]
- Berikai P, Meyer PM, Kazlauskaite R, et al. Gain in patients’ knowledge of diabetes management targets is associated with better glycemic control. Diabetes Care 2007;30:1587-9. [Crossref] [PubMed]
- Anderson RM, Funnell MM, Butler PM, et al. Patient emplowerment: results of a randomized controlled trial. Diabetes Care 1995;18:943-9. [Crossref] [PubMed]
- Rachmani R, Levi Z, Slavachevski I, et al. Teaching patients to monitor their risk factors retards the progression of vascular complications in high-risk patients with type 2 diabetes mellitus: a randomized prospective study. Diabet Med 2002;19:385-92. [Crossref] [PubMed]
- Irizarry T, Dabbs AD, Curran CR. Patient portals and patient engagement: a state of the science review. J Med Internet Res 2015;17:e148. [Crossref] [PubMed]
- Ammenwerth E, Schnell-Inderst P, Hoebst A. The impact of electronic patient portals on patient care: a systematic review of controlled trials. J Med Internet Res 2012;14:e162. [Crossref] [PubMed]
- Coughlin SS, Prochaska JJ, Williams LB, et al. Patient web portals, disease management, and primary prevention. Risk Manag Healthc Policy 2017;10:33-40. [Crossref] [PubMed]
- Sarkar U, Karter AJ, Liu JY. The literacy divide: health literacy and the use of an Internet-baed patient portal in an integrated health system—results from the Diabetes Study of Northern California (DISTANCE). J Health Commun 2010;15:183-96. [Crossref] [PubMed]
- Goldzweig CL, Orshansky G, Paige NM, et al. Electronic patient portals: evidence on health outcomes, satisfaction, efficiency, and attitudes. Ann Int Med 2013;159:677-87. [Crossref] [PubMed]
- Osborn CY, Mayberry LS, Mulvaney SA, et al. Patient web portals to improve diabetes outcomes: a systematic review. Curr Diab Rep 2010;10:422-35. [Crossref] [PubMed]
- Wade-Vuturo AE, Mayberry LS, Osborn CY. Secure messaging and diabetes management: experiences and perspectives of patient portal users. J Am Med Inform Assoc 2013;20:519-25. [Crossref] [PubMed]
- Harris LT, Haneuse SJ, Martin DP, et al. Diabetes quality of care and outpatient utilization associated with electronic patient-provider messaging: a cross-sectional analysis. Diabetes Care 2009;32:1182-7. [Crossref] [PubMed]
- Harris LT, Koepsell TD, Haneuse SJ, et al. Glycemic control associated with secure patient-provider messaging within a shared electronic medical record: a longitudinal analysis. Diabetes Care 2013;36:2726-33. [Crossref] [PubMed]
- Zhou YY, Kanter MH, Wang JJ, et al. Improved quality at Kaiser Permanente through e-mail between physicians and patients. Health Aff (Millwood) 2010;29:1370-5. [Crossref] [PubMed]
- Tenforde M, Nowacki A, Jain A, et al. The association between personal health record use and diabetes quality measures. J Gen Intern Med 2012;27:420-4. [Crossref] [PubMed]
- Grant RW, Wald JS, Schnipper JL, et al. Practice-linked online personal health records for type 2 diabetes mellitus. A randomized controlled trial. Arch Intern Med 2008;168:1776-82. [Crossref] [PubMed]
- Ralston JD, Hirsch IB, Hoath J, et al. Web-based collaborative care for type 2 diabetes: a pilot randomized trial. Diabetes Care 2009;32:234-9. [Crossref] [PubMed]
- McCarrier KP, Ralston JD, Hirsch IB, et al. Web-based collaborative care for type 1 diabetes: a pilot randomized trial. Diabetes Technol Ther 2009;11:211-7. [Crossref] [PubMed]
- Tang PC, Overhage JM, Chan AS, et al. Online disease management of diabetes: Engaging and Motivating Patients Online With Enhanced Resources-Diabetes (EMPOWER-D), a randomized controlled trial. J Am Med Inform Assoc 2013;20:526-534. [Crossref] [PubMed]
- Lau M, Campbell H, Tang T, et al. Impact of patient use of an online patient portal on diabetes outcomes. Can J Diabetes 2014;38:17-21. [Crossref] [PubMed]
- Tutino GE, Yang WY, Li X, et al. A multicentre demonstration project to evaluate the effectiveness and acceptability of the web-based Joint Asia Diabetes Evaluation (JADE) programme with or without nurse support in Chinese patients with Type 2 diabetes. Diabet Med 2017;34:440-50. [Crossref] [PubMed]
- Morris NS, MacLean CD, Littenberg B. Literacy and health outcomes: a cross-sectional study in 1002 adults with diabetes. BMC Fam Pract 2006;7:49. [Crossref] [PubMed]
- Cavanaugh K, Huizinga MM, Wallston KA, et al. Association of numeracy and diabetes control. Ann Int Med 2008;148:737-46. [Crossref] [PubMed]
- Schillinger D, Grumbach K, Piette J, et al. Association of health literacy with diabetes outcomes. JAMA 2002;288:475-82. [Crossref] [PubMed]
Cite this article as: Coughlin SS, Williams LB, Hatzigeorgiou C. A systematic review of studies of web portals for patients with diabetes mellitus. mHealth 2017;3:23.


