Applying a mobile survey tool for assessing lymphatic filariasis morbidity in Mtwara Municipal Council of Tanzania
Introduction
Lymphatic filariasis (LF) is a disease of the poor that is prevalent in 73 tropical and sub-tropical countries. LF is caused by three species of filarial worms—Wuchereria bancrofti, Brugia malayi and B. timori—and is transmitted by multiple species of mosquitoes. The disease is expressed in a variety of clinical manifestations, the most common being hydrocele and chronic lymphedema/elephantiasis of the legs or arms. People affected by the disease suffer from disability, stigma and associated social and economic consequences. Marginalized people, particularly those living in areas with poor sanitation and housing conditions are more vulnerable and more affected by the disease. Estimates made in 1996 indicated that 119 million people were infected with LF at that time, 43 million of them having the clinical manifestations (principally lymphedema and hydrocele) of chronic LF disease (1).
In Tanzania, with an estimated 34 million people at risk and 6 million people affected (2), a National Lymphatic Filariasis Elimination Programme (NLFEP) was established and began operations in 2000 focusing mainly on preventive chemotherapy using mass drug administration (MDA) of ivermectin and albendazole. The endemicity varies from being highly endemic along the coast with antigenemia levels of 45–60%, to low endemicity in the areas of Western Tanzania with endemicity of 2–4%, and varying endemicity in the regions in between, i.e., central Tanzania, the southern Highlands and north and northwestern Tanzania (2). Following six rounds of MDA, there is evidence to suggest considerable decrease in all the measured indices of LF transmission and human infection (3); however, cut-off levels required to interrupt transmission have not been attained even after 8 years of MDA in Tanga (4).
A number of methods have been used to estimate LF morbidity, including: routine programmatic data; cluster random surveys (5); and the “town crier” method recently trialed in Nigera (6). Currently, few accurate data exist on the global LF morbidity burden. The global estimates, 40 million people with clinical filarial disease—25 million with hydrocele and 15 million with lymphedema/elephantiasis—haven’t changed in the last decade (7). Even in developed countries (Europe and the US) estimating the population burden of lymphedema and hydrocele is considered difficult due to complex and variable pathology and current prevalence estimates are considered likely underestimates. Accurate estimation of the prevalence of a condition that occurs at low prevalence (<1%) requires large sample sizes thus making population-based clinical surveys costly. In the published literature there have been numerous methods used to quantitate LF morbidity burden, yet the literature suffers from minimal research on the quality of the methods and there is no ‘gold standard’ methodology. Operational research is needed to make formal recommendations on the best methods to assess lymphedema/elephantiasis and hydrocele burden. This mobile phone-based survey aimed to estimate prevalence of hydrocele and lymphedema in Mtwara Municipal Council.
Methods
Study population
The study was undertaken in Mtwara Municipal Council which has an estimated population of 108,299 (8) with an estimated 60–70% of population being mobile phone subscribers (Figure 1, map). Mtwara Municipal council was selected because it has one of the highest LF morbidity and is served under the Morbidity Management Programme in Mtwara Region (http://imaworldhealth.org/morbidity-management-another-dimension-in-the-fight-against-ntds-in-tanzania/). The survey targeted adult mobile phone users in Mtwara Municipal Council.
Study design
The study was a cross-sectional mobile phone-based survey. A sample size of 384 completed surveys was required to estimate prevalence of lymphedema (both male and female) and hydrocele (male only) morbidity of 50% given a 5% error margin, 5% level of significance and 95% level of significance. The survey system was set-up to automatically send surveys until exactly 384 surveys were completed and submitted, which was estimated to be achievable over the course of one week.
Data collection and data security
The data was collected via GeoPoll (http://research.geopoll.com/). Mobile phone users in study setting were randomly selected from GeoPoll database. Consent and survey questions were sent to participants via short message service (SMS) with a choice of English or Swahili languages. Only people aged 18 years and above were eligible to participate in the survey. All participants who completed survey were offered a talk-time incentive of TZs500. Prior to the survey broadcast, information was provided to the target population via local radio station.
The survey was interactive with branching and looping based on previous responses. As a standard procedure, all respondents were assigned an anonymous user identification (ID) number thus it was not possible to know the mobile phone number for individual participants. Survey response data received from respondents was housed in Mobile Accord/GeoPoll’s secure servers. Only authorized investigators were allowed to access and download data from secure servers using password protected applications.
Data analysis
Statistical analysis was conducted using Stata 12.0 (Stata Corporation, College Station, Texas). Descriptive statistics were generated to describe characteristics of study population and estimates of prevalence of lymphedema and hydrocele. Differences in mean age and proportions were tested for statistical significance using the t-test and prtest, respectively.
Ethical considerations
The study protocol was approved by the Medical Research Coordinating Committee (MRCC) of the National Health Research Ethics Review Sub-Committee (NatHREC). Participation the survey was voluntary. Consent was obtained from all study participants through the SMS-based questionnaire. No personal identifiers were collected for this study.
Results
Characteristics of the sample
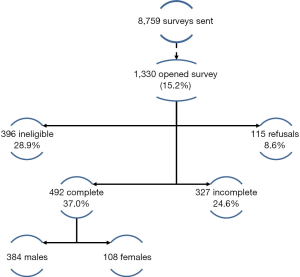
Figure 2 shows the number of SMS sent by Geopoll and outcomes of the surveys. A total of 8,759 surveys were sent to mobile phone subscribers via SMD of whom 1,330 (15.2%) opted-in to complete the survey. A total of 492 (37.0% of those opted-in, 384 male and 108 female) people completed the survey. Of the opened SMS not completed, 28.9% were ineligible, 24.6% were incomplete and 8.6% declined to participate. The mean age of survey participants was 20.1 (standard deviation, 6.5) years. There was no difference in mean aged between male and female participants (P value=0.5). The survey was completed over a period of 4 days.
Prevalence of lymphedema and hydrocele
Table 1 summarizes the prevalence of lymphedema and hydrocele. Of all the 492 surveys completed, lymphedema signs were reported by 20.9% (95% CI, 17.4–24.8) respondents. Females reported higher lymphedema (22.2%) compared to males (20.6%); however, this difference was not statistically significant (P value=0.7). Among 384 male respondents, hydrocele signs were reported by 20.6% (95% CI, 16.6–25.0) of respondents. In addition, 9.4% of the male respondents reported having signs of both lymphoedema and hydrocele.
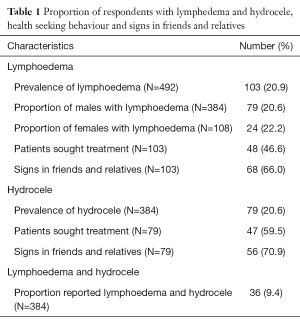
Full table
Health seeking behaviour and symptoms among family members
Majority of hydrocele patients (59.5%) reported having sought treatment and 70.9% reported similar symptoms among friends and relatives. Among lymphedema patients, 46.6% of reported having sought treatment and majority (66.0%) reported similar symptoms among friends and relatives (Table 1).
Discussion
This survey of lymphedema and hydrocele showed that application of mobile phone based methods can be rapidly deployed to undertake morbidity surveys in endemic settings. The survey showed that a fifth adult respondents (male and female) had lymphedema, a fifth of adult males had hydrocele and nearly a tenth of adult males reported having both lymphedema and hydrocele. Three fifths of hydrocele patients and nearly half of lymphedema patients reported having sought treatment. Of the participants reporting signs of LF morbidity, 2 thirds and 7 out of 10 reported that friends had relatives had signs of lymphedema and hydrocele, respectively. This survey will be valuable in planning services in this resource poor setting.
The World Health Organization recognizes that the use of mobile and wireless technologies to support the achievement of health objectives (mHealth) has the potential to transform the face of health service delivery across the globe (9). In developing country settings, mobile phone technology has been successfully pilot for use in routine disease surveillance (10) and large scale population based surveys (11). Compared to traditional paper based methods, use of mobile phone based applications has been shown to improve accuracy of data, reduced data transmission time and cost, and improve data quality (9). However, use of mobile phones to directly poll respondents has been limited.
Consistent with our findings, a recent case study of Mobiles for Reproductive Health in Kenya showed that SMS surveys are a feasible mode of data collection for target populations (12). In Malawi and Ghana, a mobile phone based pilot concluded that community-based health workers were able to quantify LF morbidity burden, and other NTDs with observable symptoms (13). Unlike, the Malawi study, our survey polled the respondent directly for self-reports of clinical signs of lymphedema and hydrocele.
The mobile phone based survey approach has a number of strengths. The main advantages of using SMS messages for health campaigns are their low cost and broad reach (9). The entire survey of 492 participants was completed within 4 days with the first batch of 384 questionnaires being completed within 24 h. This mobile-based approach can be expected to have low cost per completed survey especially in surveys where large numbers of people are polled. Our study has a number of potential limitations. Firstly, the survey was based on self-reports of the clinical signs of lymphedema and hydrocele; therefore, there is need to undertake further clinical surveys to verify the sensitivity and specificity of self-diagnosis compared to diagnosis by clinicians. In addition, there are concerns that there are other differential diagnosis that have similar clinical presentations to lymphedema and hydrocele. However, morbidity surveys based on questionnaires have shown that this approach is likely to underestimate morbidity prevalence (14). We offered the participants a talk-time incentive of TZs500/- for the completed survey. There are concerns that offering incentives may be a source of bias; however, evidence from a case study in Kenya suggests that survey incentives for completion had no effect on the response rates (12).
Conclusions
In conclusion, the findings suggest that mobile phone based surveys are a practical approach of undertaking morbidity surveys. While further surveys are needed to verify the findings, this approach can be expected to encourage identification of lymphedema and hydrocele morbidity at community level and provide evidence where further morbidity surveys are warranted.
Acknowledgements
The authors are grateful to the health authorities in Mtwara Municipal Council for help with survey planning and Prime FM radio for community sensitization prior to the surveys.
Funding: The survey was funded by RTI International.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study protocol was approved by the Medical Research Coordinating Committee (MRCC) of the National Health Research Ethics Review Sub-Committee (NatHREC). Participation the survey was voluntary. Consent was obtained from all study participants through the SMS-based questionnaire. No personal identifiers were collected for this study.
References
- Michael E, Bundy DA, Grenfell BT. Re-assessing the global prevalence and distribution of lymphatic filariasis. Parasitology 1996;112:409-28. [Crossref] [PubMed]
- Malecela M, Lazarus W, Mwingira U, et al. Eliminating LF: a progress report from Tanzania. J Lymphoedema 2009;4:10-2.
- Simonsen PE, Derua YA, Kisinza WN, et al. Lymphatic filariasis control in Tanzania: effect of six rounds of mass drug administration with ivermectin and albendazole on infection and transmission. BMC Infect Dis 2013;13:335. [Crossref] [PubMed]
- Simonsen PE, Derua YA, Magesa SM, et al. Lymphatic filariasis control in Tanga Region, Tanzania: status after eight rounds of mass drug administration. Parasit Vectors 2014;7:507. [Crossref] [PubMed]
- WHO Global Programme to Eliminate Filariasis. Monitoring and epidemiological assessment of the programme to eliminate lymphatic filariasis at implementation unit level. Geneva: World Health Organization; 2005. Available online: [cited 2016 Oct 24].http://apps.who.int/iris/bitstream/10665/69172/1/WHO_CDS_CPE_CEE_2005.50.pdf
- Mathieu E, Amann J, Eigege A, et al. Collecting baseline information for national morbidity alleviation programs: different methods to estimate lymphatic filariasis morbidity prevalence. Am J Trop Med Hyg 2008;78:153-8. [PubMed]
- Ottesen EA, Hooper PJ, Bradley M, et al. The global programme to eliminate lymphatic filariasis: health impact after 8 years. In: Institute of Medicine (US) Forum on Microbial Threats. The Causes and Impacts of Neglected Tropical and Zoonotic Diseases: Opportunities for Integrated Intervention Strategies. Washington (DC): National Academies Press (US); 2011.
- National Bureau of Statistics (NBS) and Office of Chief Government Statistician (OCGS), Zanzibar. 2013. 2012 Population and Housing Census: Population Distribution by Administrative Units; Key Findings. Dar es Salaam, Tanzania: NBS and OCGS. Available from: [cited 2016 Oct 10].http://nbs.go.tz/nbs/sensa/PDF/2012%20PHC%20POPULAR%20VERSION.pdf
- World Health Organization. mHealth: new horizons for health through mobile technologies. Geneva: World Health Organization; 2011.
- Déglise C, Suggs LS, Odermatt P. SMS for disease control in developing countries: a systematic review of mobile health applications. J Telemed Telecare 2012;18:273-81. [Crossref] [PubMed]
- Solomon AW, Pavluck AL, Courtright P, et al. The Global Trachoma Mapping Project: Methodology of a 34-Country Population-Based Study. Ophthalmic Epidemiol 2015;22:214-25. [Crossref] [PubMed]
- Johnson D. Collecting Data from mHealth Users via SMS Surveys: A Case Study in Kenya. Surv Pract 2016;9. [cited 2016 Oct 27].
- Stanton MC, Mkwanda SZ, Debrah AY, et al. Developing a community-led SMS reporting tool for the rapid assessment of lymphatic filariasis morbidity burden: case studies from Malawi and Ghana. BMC Infect Dis 2015;15:214. [Crossref] [PubMed]
- Mathieu E, Amann J, Eigege A, et al. Collecting baseline information for national morbidity alleviation programs: different methods to estimate lymphatic filariasis morbidity prevalence. Am J Trop Med Hyg 2008;78:153-8. [PubMed]
Cite this article as: Mwingira UJ, Downs P, Uisso C, Chikawe M, Sauvage-Mar M, Malecela MN, Crowley K, Ngondi JM. Applying a mobile survey tool for assessing lymphatic filariasis morbidity in Mtwara Municipal Council of Tanzania. mHealth 2017;3:8.