
Social support via Internet communication technology for diabetes self-management: a scoping review
Highlight box
Key findings
• This review identifies and describes highly scalable social support interventions combining Internet and communication technologies (ICT) to enhance diabetes self-management for adults. A variety of ICT modalities were examined, including peer web forums, interactive voice recordings, messaging, and email, with no suggestion of difference between ICT modality of support training.
What is known and what is new?
• Studies that explicitly measured patients’ perception of social support consistently reported positive effects on psychosocial, behavioral, and clinical outcomes. Strategies that prioritize existing support relationships over new connections may demonstrate better behavior change and clinical outcomes. Despite observational evidence that social support plays a crucial role in diabetes self-management, the effectiveness of ICT strategies to enhance social support in changing health beliefs, behaviors, and clinical outcomes requires more rigorous research.
• This scoping review focuses on the addition of support to patient-focused ICT interventions, contributing a new perspective to the literature.
What is the implication, and what should change now?
• This study highlights the potential impact of different ICT modalities on diabetes self-management and emphasizes the importance of targeting specific social support domains, including informational, tangible, appraisal, and emotional support.
Introduction
The global prevalence of diabetes has increased over the past 30 years due to nutritional changes, physical inactivity, and rising rates of obesity (1). Diabetes is the leading cause of amputations, blindness, and kidney failure in developed countries (2-4). Although diabetes is preventable, and the risk of complications can be reduced through appropriate self-management with adequate medical care, the disease is recalcitrant due to the complex and continued behavior changes required (5). Many people with diabetes find the necessary lifestyle changes–continual attention to nutrition choices, physical activity, and medication taking–overwhelming, and are unable to effectively manage their chronic disease (6-8). Diabetes self-management education and support interventions generally focus on the individual patient, guiding patients towards healthier behavior choices (9). However, these approaches are stymied if patients face systemic barriers related to social determinants of health or do not have sufficient support from family and friends to make these changes (10). Higher levels of social support are consistently associated with improved clinical outcomes for people living with diabetes (11).
Strategies that incorporate family and friends that impact daily health decisions may reduce barriers to healthy behavior choices for patients with chronic disease (12), and specifically for patients with diabetes who are not achieving glycemic stability (13-16). In a systematic review without meta-analysis, Strom and Egede describe how appropriate social support is related to improved health behaviors and blood glucose levels for patients with diabetes (17). In a meta-analysis of social network interventions for diabetes, Spencer-Bonilla et al. found that social network interventions improved A1C at −0.25 percentage points at 3 months post intervention (18). Social support consists of four domains: informational, tangible, appraisal, and emotional (19). Appraisal support is the provision of information useful for self-evaluation. Emotional support refers to expressions of empathy, love, trust, and care which result in improved affect for the recipient, such as listening to the concerns of a loved one. Informational support refers to advice, suggestions, and information provided to a loved one. Tangible support consists of tangible aid and services, such as driving a loved one to a doctor’s appointment. While the American Diabetes Association recommends a mixture of emotional, tangible, and informational support, there is also value in appraisal support (20). Interventions designed to instigate social support may be designed to target one or more of these categories.
Recruiting family or friends to serve as a support person to a person with diabetes is effective, but requires a high level of commitment, and implementing and maintaining in-person support person trainings can impose financial, logistical, and personnel burdens (20,21). For example, many support persons may be employed on a full-time basis, making it difficult for them to be fully present for in-person interventions (22). To reduce these burdens, interventions using Internet and communication technologies (ICT) can be used to train support persons by prompting them to provide appropriate social support and as an avenue to offer support to a person with diabetes. Employing ICT for social support interventions could allow for inclusion of family members who most influence the patient’s behaviors and can be trained to provide support, rather than those who live closest to the patient or who have the most available free time to travel and be trained. ICT-based strategies may broaden the reach of interventions that develop new support relationships between peers, matching people with similar experiences and challenges rather than those that share a living space. Merging ICT and social support interventions could generate a solution that has the cost-effectiveness and scalability of mobile technologies coupled with the personal touch of social support.
While well established for patient-focused interventions (23), few studies implement mHealth and other ICT strategies to incorporate support persons, and a variety of ICT and social support strategies are used in the studies that do incorporate social support and ICT. Many interventions incorporate physicians, nurses and other health professionals into patient monitoring and decision making, which is particularly sought after and effective for patients who lack sufficient baseline support (24). However, these interventions have limited scalability, as they still require intensive amounts of time from these health professionals. Recruiting family members and friends to be trained to provide self-management support via ICT strategies is less prevalent, as is building new support networks. For those studies that augment existing support relationships or build new ones, the domains of social support emphasized in these interventions must be better understood to be able to highlight features and domains that should be continued in new interventions. An additional barrier to assessing the literature on this topic is the limited studies examining support interventions against patient-focused interventions, rather than patient and supporter-focused interventions against usual care control groups.
In this scoping review, we examine the current state of interventions that combine scalable ICT strategies and social support techniques to improve diabetes self-management for adults. We focused on rigor of study design and risk of bias, ICT modalities employed, support relationships strengthened or created, and social support domain emphasized. We present our findings in tables organized by these guiding themes. We present this article in accordance with the PRISMA-ScR reporting checklist (available at https://mhealth.amegroups.com/article/view/10.21037/mhealth-23-34/rc) (25).
Methods
We conducted three searches on October 6, 2018, December 19, 2022, and September 11, 2023 for studies combining terms for diabetes, ICT, and social support interventions (including family support, peer support, and support from community health workers). We searched the following search engines: PubMed, Ovid, Cumulative Index to Nursing and Allied Health Literature (CINAHL), and Association for Computing Machinery (ACM) Digital Library. See Appendix 1 for detailed search terms for PubMed. The protocol for this study was registered in the PROSPERO database (ID #CRD42023402169).
Both investigators independently screened titles and abstracts for inclusion. Criteria for inclusion were adult patients with diabetes, a primarily ICT-based strategy to instigate social support, and augmentation of peer, family member, friend, or community health worker-based social support. If either author elected to include a manuscript for full-text review, the manuscript was included. Manuscript full-texts were examined for inclusion by two investigators. All disagreements were reviewed weekly, and collaborative decisions on study inclusion were reached on all manuscripts. Based on these exclusion criteria, we excluded 723 articles during the full-text review process. Studies were excluded based on the following criteria:
- No intervention outcomes described n=197 (cross-sectional studies n=24, no intervention described n=72, discussion of design features/needs assessment n=36, study protocol only n=65).
- Not social support-based n=134 (no social support/peer support/community health worker social support n=134).
- Patient population was not adults with diabetes n=79 (not diabetes n=21, emerging adults n=4, pediatric population n=44, wrong patient population n=10).
- Not original research n=102 (review papers n=100, duplicate in another journal n=2).
- Not scalable ICT intervention n=145 (not ICT-based n=32, telephone call-based n=30, more than 2 face to face visits n=83).
- Reported outcomes were not clinical, behavioral, or psycho-social n=66 (wrong outcomes n=66).
We categorized any web-cam interactions requiring synchronous one-on-one counseling or training—such as video-based or telehealth meetings—as face-to-face meetings. While these methods fall within the realm of ICT, their exclusion allows researchers to focus on exploring novel technologies or strategies that are highly scalable and increase the number of patients who could be served by a single provider.
Studies selected for inclusion were then abstracted for study population, design [quasi-experimental/observational vs. randomized controlled trials (RCTs)], and outcomes. We additionally abstracted the social support domains emphasized (whether explicitly defined, implicitly referenced, or lacking in theoretical framework), support relationship intervention strategy (strengthening an existing relationship or developing a new support relationship), and ICT modality [messaging-based interventions—including Short Message Service (SMS) and instant messaging, app-based/web portal/social media forum, email, or interactive voice recording (IVR)]. Outcomes were categorized as perception of social support, psychosocial, behavioral, or clinical outcomes. In situations where divergent opinions or disputes arose, the authors engaged in a collective effort to establish a unified consensus.
Quantitative data synthesis was not possible given the inconsistency and non-conformity of reporting of clinical, psychosocial or support outcomes. Instead, patterns of significant differences, positive but non-significant differences and equivalent differences were examined qualitatively using tables organized by these categories: type of support relationships emphasized in the intervention, perception of social support measured, implicit vs. explicit social support domains described and study design.
Results
The searches resulted in 12,206 studies from the registered databases. After 5,377 duplicates were removed, there were 6,829 unique articles that matched the search terms (Figure 1). From title and abstract review, 762 articles were selected for full-text review if the title or abstract indicated an original research study that referenced diabetes, social or family support, and any digital, mobile, or asynchronous communication modalities. After full-text review, 39 articles were selected for data abstraction. However, several interventions were deployed in multiple study populations, so these 39 studies actually represent 27 unique interventions. Four ICT modalities were identified: app- and web forum-based interventions, IVR-based interventions, email-based interventions, and messaging-based interventions; some studies incorporated multiple modalities (Table 1).
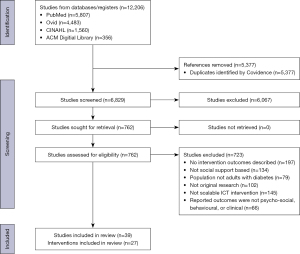
Table 1
| ICT modality | First author (month year) | Intervention name | Study design | Study population |
|---|---|---|---|---|
| App- and web forum-based interventions | Glasgow, August 1999 (26) | D-NET | Quasi-experimental (no comparator) | International population (n=221) |
| Smith, July 2000 (27) | Women to Women Diabetes Project | RCT (computer intervention vs. control) | Gestating patients with type 1 diabetes in rural Montana, USA (n=30, 15 in intervention group) | |
| McKay, February 2002 (28); Glasgow, April 2003 (29) | D-NET | RCT (Peer support vs. self-management coach vs. usual care) | Patients with diabetes in the Pacific Northwest of the USA (n=320) | |
| Barrera, October 2002 (30) | D-NET | RCT (diabetes information only vs. a personal self-management coach vs. a social support intervention vs. a personal self-management coach and the support intervention) | Patients with diabetes with no prior access to Internet in USA (n=160, 40 per each of four arms) | |
| Jennings March 2009 (31); Powell, April 2009 (32) | Virtual Clinic | Quasi-experimental (no comparator) | Patients with diabetes in the United Kingdom using insulin pumps (n=17) | |
| Chomutare, July 2013 (33) | FTA | Quasi-experimental (no comparator) | Patients with diabetes (n=7) | |
| Heisler, November 2014 (34) | iDecide | RCT (peer coaches who used iDecide vs. those who did not) | Patients with diabetes from predominantly Latine, African American, and low socioeconomic backgrounds at a Detroit, Michigan, USA community health center (n=188, 93 iDecide, 95 printed materials) | |
| Linden, February 2018 (35) | MoDIAB | RCT (web-based support with peer forum vs. usual care) | Patients with gestational diabetes in Sweden, postpartum (n=174, 83 in intervention group) | |
| Berg, May 2018 (36) | MoDIAB | Quasi-experimental (no comparator) | Patients with gestational diabetes in Sweden, postpartum (n=81, 61 used peer support web forum) | |
| Saslow, August 2018 (37) | Low-Carb Program | Quasi-experimental (pre-post) | Women with diabetes from predominantly white backgrounds (n=1,000) | |
| Heisler, June 2019 (38) | iDecide | RCT (peer coaches who used iDecide vs. those who did not) | Outpatients with diabetes from predominately African American backgrounds at a VA clinic in the USA (n=255, 74 peer coaches) | |
| Pemu, June 2019 (39) | e-Healthystrides | Quasi-experimental (no comparator) | Churchgoers with diabetes from African American backgrounds in the USA (n=264) | |
| Zheng, December 2019 (40); Liu, November 2022 (41) | TangTangQuan | Quasi-experimental (no comparator) | Patients with diabetes in China (n=693) | |
| Lyles, February 2021 (42) | InquisitHealth | Quasi-experimental (no comparator) | English and Spanish-speaking patients with diabetes at a safety-net delivery system in New York, USA (n=618) | |
| Zhang, February 2021 (43) | LCCP | Retrospective cohort with matched controlled | Patients with diabetes in China (n=780, 394 for matched controls) | |
| Allen, March 2022 (44) | SHARE plus | Quasi-experimental (no comparator) | Patients with diabetes in Utah, USA (n=20) | |
| Litchman, July 2022 (45) | CGM + OPSC | Quasi-experimental (no comparator) | Spanish speaking patients with diabetes from Latine backgrounds recruited from community events (n=34 enrolled, 5 moderators) | |
| Sklar, December 2022 (46) | CGM Share | Non-randomized trial | Gestating patients with type 1 diabetes in Colorado, USA (n=28, 13 CGM alone, 15 shared CGM) | |
| Interactive voice recording-based interventions | Heisler, November 2005 (47) | Reciprocal Peer Support | Quasi-experimental (no comparator) | Midwestern USA VA patients with diabetes (n=40, all with peer supporter) |
| Heisler, October 2010 (48) | Reciprocal Peer Support | RCT (peer support vs. nurse case manager support) | Male veterans in Ann Arbor, Michigan, USA (n=244, 126 with supporter) | |
| Rosland, November 2022 (49) | CO-IMPACT | RCT (IVR to patient and supporter vs. standard care) | Veterans with diabetes in USA (n=239, 119 with CO-IMPACT intervention) | |
| Email-based interventions | Reese, April 2016 (50) | PROMOTE + SUPPORT | RCT (supporter receives email about patient’s medication adherence vs. usual care) | Patients with diabetes in USA with Humana insurance (n=200, 150 with supporter) |
| Short-message-service/text message-/instant message-based interventions | Mayberry, November 2016 (21) | FAMS | Quasi-experimental (no comparator) | Patients with diabetes from low-socioeconomic backgrounds in Nashville, Tennessee, USA (n=19, 7 with supporter) |
| Burner, January 2018 (51) | TExT-MED + FANS | RCT (SMS to supporter and patient vs. SMS to patient alone) | Patients with diabetes from Latine and low socioeconomic backgrounds residing in Los Angeles, California, USA (n=44; 22 with SMS to supporter) | |
| Mayberry, March 2021 (52); Roddy, February 2022 (53) | FAMS | RCT (control to self-management only to self-management + FAMS) | Patients with diabetes from racial/ethnic minority and low-socioeconomic backgrounds residing in Nashville, Tennessee, USA (n=506, 253 control, 127 self-management only, 126 self-management + FAMS) | |
| Ojewale, December 2022 (22) | FIDE | Quasi-experimental (cluster randomization with two clusters) | Patients with diabetes in university hospitals in southwest Nigeria (n=170, 82 receiving intervention, 88 control) | |
| Mixed modality-based interventions | Aikens, March 2014 (54), March 2015 (55), April 2015 (56) | CarePartners | Quasi-experimental (comparator groups of patients with and without supporter not randomized) | Patients with diabetes at a Midwestern USA VA clinic (n=301; 118 with supporters) |
| Suh, April 2014 (57) | Internet Mentoring Program | RCT (SMS to peer mentor vs. no peer mentor assigned, patients upload glucose readings to web) | Patients with diabetes in South Korea (n=57, 26 with peer mentor) | |
| Ho, November 2015 (58) | mDAWN | Quasi-experimental (no comparator) | Patients with diabetes in Canada (n=56, 28 agreed to enroll a supporter) | |
| Ramirez, June 2017 (59) | PMFF | RCT (control vs. phone messaging vs. phone messaging + social support) | Participants of a diabetes management program at an ambulatory care clinic of Los Angeles County Department of Health Services in Los Angeles, California, USA (n=42, 14 per each of three arms) | |
| Lari, January 2018 (60) | CD Training + SMS | RCT (SMS to patient and supporter with CD training in home vs. usual care) | Patients with diabetes in southwest Iran (n=76, 40 in intervention) | |
| McManus, July 2018 (61) | FDD | RCT (web forum and emails for patient and partner vs. usual care) | Patients with gestational diabetes in Canada during the postpartum period (n=170, 89 in intervention) | |
| Lystrup, September 2020 (62) | Fitbit + Friends | RCT (activity monitor with or without placement into virtual activity groups) | Patients with diabetes at Department of Defense military medical facilities (n=120, 60 per each of two arms) |
ICT, internet and communication technologies; D-NET, Diabetes Network; RCT, randomized-controlled trial; FTA, FewTouch Application; MoDIAB, Mothers and Diabetes Web; VA, Veterans Affairs; LCCP, Lilly Connected Care Program; CGM + OPSC, Continuous Glucose Monitoring and Online Peer Support Community; CO-IMPACT, Caring Others Increasing Engagement in Patient Aligned Care Teams; IVR, interactive voice recording; FAMS, Family-focused Add-on to Motivate Self-care; TExT-MED + FANS, Trial to Examine Text-Messaging in Emergency patients with Diabetes + Family and friends Network Support; SMS, Short Message Service; FIDE, Family-Integrated Diabetes Educational Programme; mDAWN, mobile Digital Access to a Web-enhanced Network; PMFF, Phone Messaging + Friends/Family; CD, computer compact disk; FDD, Family Defeating Diabetes.
Twenty-one studies described 15 unique peer-support app-based or web forum-based interventions. Glasgow et al. (26,29), Barrera et al. (30), and McKay et al. (28) describe the Diabetes Network (D-NET) intervention, a curated diabetes informational website designed for adults with low technological literacy, and included two in home training sessions, online assessments, and automated dietary goal settings. In a randomized controlled trial, patients received D-NET alone, D-NET plus Tailored Self-Management Professional Coaching, or D-NET plus Peer Support via the Diabetes Support Conference, a peer forum that had minimal moderation. While they found that web forum use was correlated with higher perception of support by multiple measures, and a non-significant difference improvement in glycemic stability (A1c), they did not find any changes in neither self-reported behavioral outcomes nor psycho-social outcomes. Smith and Weinert (27) focus on patients with gestational diabetes for the Women to Women Diabetes Project, which showed no difference in psycho-social outcomes or perceived support between the intervention and control groups. Jennings et al. (31) and Powell et al. (32) describe an observational study of a Virtual Diabetes Clinic for patients with type 1 diabetes mellitus (T1DM) utilizing insulin pumps which provided curated information, a venue to reach care providers, and a peer support forum. The researchers found no difference in quality of life or glycemic stability. Chomutare et al. (33) discuss the FewTouch Application (FTA), a quasi-experimental study featuring seven participants meant to better understand the design feature needs of FTA. Study results indicate non-significant improvements in psycho-social and clinical outcomes, with no measure of explicit support or behavioral outcomes. Heisler et al. (34,38) discuss iDecide, an interactive app-based RCT where both groups’ A1c values improved. Linden et al. (35) and Berg et al. (36) describe the Motherhood and Diabetes Web (MoDIAB) study web forum which contains a peer support forum in addition to diabetes information and a self-management diary. Patients were randomized to MoDIAB or usual care. In qualitative analysis, they found that participants found the emotional support comforting, but found no differences in psycho-social or clinical outcomes. Saslow et al. (37) study the Low-Carb Program, a quasi-experimental study with a study population that mostly consisted of females identifying from white racial/ethnic backgrounds, showed an overall improvement in glycemic stability and weight. Pemu et al. (39) describe e-Healthystrides, a web forum and remote discussion peer support facilitated by coaches, which indicated that improvements to self-management behaviors significantly improved during the study. Zheng et al. (40) and Liu et al. (41) discuss TangTangQuan, a quasi-experimental retrospective study with participants located in China. The TangTangQuan program resulted in improved A1c, mean fasting blood glucose (FBG), and postprandial blood glucose within a 12-month period. Lyles et al. (42) discuss InquisitHealth, which showed significant improvement in clinical outcomes, including glycemic stability and blood pressure. Zhang et al. (43) describe Lilly Connected Care Program (LCCP), a retrospective cohort with matched control groups for patients with type 2 diabetes mellitus (T2DM) in China. Results for this study indicated significant improvements in behavioral and clinical outcomes for those enrolled in the study with a support person. Allen et al. (44) describe SHARE plus, which were dyadic communication, problem-solving, and action planning platforms to facilitate continuous glucose monitor (CGM) data sharing, and broad improvements were shown in diabetes-related clinical outcomes. Litchman et al. (45) focused on Continuous Glucose Monitoring and Online Peer Support Community (CGM + OPSC), a web forum for Spanish-speaking adults from Hispanic/Latine backgrounds that showed significant improvement in A1c and CGM monitoring outcomes. Sklar et al. (46) describe CGM Share, a non-randomized trial featuring patients with gestational diabetes. While it did not mention psycho-social or behavioral outcomes, or perceived support, it did show significant improvement in clinical outcomes for study participants enrolled in the study with social support.
Three articles described two unique IVR interventions, in which patients can interact with pre-recorded messages via touch tone or voice commands. Heisler and Piette (47) and Heisler et al. (48) describe an IVR-based peer-support intervention named Reciprocal Peer Support, in which peer supporters were prompted to contact each other via IVR. In a quasi-experimental study, the investigators found improvements in self-efficacy and self-management. In the RCT of IVR prompted peer support vs. nurse case manager support, the investigators found improved perception of social support, and a trend toward improvements in depression, diabetes distress, and A1c of 0.58 (P=0.004) compared to nurse case manager support. Moreover, Rosland et al. (49) discuss the Caring Others Increasing Engagement in Patient Aligned Care Teams (CO-IMPACT), which showed that patients in the CO-IMPACT arm also had greater 12-month improvements in healthy eating, diabetes self-efficacy, and satisfaction with support person involvement. Despite this, the two arms had similar improvements in A1c levels and in other measures.
One email-based intervention was described by Reese et al. (50) in a RCT of PROMOTE + SUPPORT, an intervention in which email reports of a patient’s medication taking was emailed to a family member in addition to the patient vs. to the patient alone. This study found no differences between active control and support arms.
Five studies described two messaging-based support interventions. Mayberry et al. (21,52) and Roddy et al. (53) describe an active arm only pilot of Family-focused Add-on to Motivate Self-care (FAMS), a family-focused text message based intervention; the intervention showed improved family/friend involvement, self-efficacy, and diet at the three- and six-month timepoints. Burner et al. (51) describe a RCT pilot of an SMS-based intervention titled Trial to Examine Text-Messaging in Emergency Patients with Diabetes + Family and Friends Network Support (TExT-MED + FANS) for family members that synchronized to a patient-focused SMS intervention, compared to patients who received only the patient based intervention without the family member receiving text messages. In the intervention groups, the investigators found a significant increase in self-monitoring of glucose, a trend toward improved glycemic stability, but no differences in psycho-social outcomes, perceived support, or other self-reported health behaviors. Ojewale et al. (22) describe the Family-Integrated Diabetes Educational (FIDE) Programme. Study participants were cluster-randomized in a quasi-experimental study. The study did not report any psycho-social or behavioral outcomes or perceived support, but did report significant clinical outcome differences between pre/post groups. The one-day support training with SMS follow up was selected as the investigators were limited to a one day in-person training for social supporters due to job inflexibility, an elegant solution to the barrier of enrolling a friend/family member as a support person.
Nine articles described seven multi-modality interventions. Aikens et al. (54-56) describe a quasi-experimental investigation of an email version of the CarePartners intervention in which glucose readings and other clinical data were sent to a designated supporter. Aikens et al. found improved medication taking for patients with a CarePartner. Suh et al. (57) describe a RCT of an Internet-based mentoring program, in which patients with T1DM uploaded glucose readings to a website, which prompted a text message to an online peer mentor, who would then call, text, or email the patient to encourage behavior changes to achieve better glycemic stability (43). Compared to patients uploading glucose readings without peer mentorship, the investigators found an improvement in frequency of self-monitoring of glucose, but no differences in quality of life or glycemic stability. Ho et al. (58) describe the mobile Digital Access to a Web-enhanced Network (mDAWN), a quasi-experimental investigation of a website containing curated information, peer web forum, text messages with tips and challenges, and remote monitoring equipment that patients and family members could use for home monitoring. The investigators noted improvements in quality of life, diabetes distress, and glycemic stability, but did not examine differences between patients who did and did not have a care-giver enrolled. Ramirez and Wu (59) describe Phone Messaging + Friends/Family (PMFF), a RCT featuring patients who were enrolled in a diabetes management program within Los Angeles County. The study found no difference between groups for behavioral outcomes and nonsignificant improvements in perceived support for all three intervention arms. Lari et al. (60) describe a RCT of a computer compact disc course and SMS messaging intervention sent to patients and a family member to increase physical activity. Compared to usual care, patients who received this intervention had improved self-efficacy, perceived support, report of physical activity, and improved perception of health status. McManus et al. (61) describe an email and web forum-based intervention, Family Defeating Diabetes (FDD), for patients with a recent history of gestational diabetes in which participants who were pregnant and their respective partners were randomized to usual care or the FDD intervention. The investigators found a trend toward improved dietary choices, but no difference in weight or glycemic stability. Lystrup et al. (62) describe Fitbit + Friends, a RCT for patients with diabetes at Department of Defense military medical facilities. Patients and their partners were randomized to activity monitoring with or without placement into virtual activity groups. The investigators did not find any differences between groups for psycho-social outcomes and found non-significant differences between the two groups for clinical outcomes.
Support relationships emphasized by intervention types, and the social support domains targets, varied among the interventions. Examining the pattern of outcomes by whether an intervention utilized an existing or new support relationship (Table 2) may indicate that engaging existing supporters over developing new relationships may be more effective for behavior change and clinical outcomes. A standout against this pattern is the Reciprocal Peer Support intervention, which matched patients 1:1 to another patient with similar self-management challenges. Additionally, examining the pattern of outcomes by studies that explicitly measure the patient’s perception of support (Table 3) against those interventions that more explicitly measure support shows a more consistent pattern of improvement of psycho-social, behavioral, and clinical outcomes for studies. The interventions also varied in the incorporation of definitions of social support (see Table 4). Seven explicitly stated the domains of social support that were targeted in the intervention. These seven studies all incorporated more than one domain of social support. The most common domain emphasized overall was emotional support, followed by informational support, and appraisal support. When exploring the patterns of outcomes based on whether explicit domains of social support were targeted, or which domains were emphasized, there was no clear trend towards a benefit of explicitly or implicitly defined these domains.
Table 2
| Intervention name | Psycho-social outcomes | Perceived support | Behavioral outcomes | Clinical outcomes |
|---|---|---|---|---|
| Existing social support relationship | ||||
| CarePartners | NR | NR | + | ++ |
| CGM Share | NR | NR | NR | ++ |
| CD Training + SMS | ++ | ++ | ++ | ++ |
| e-Healthystrides | ++ | NR | ++ | – |
| FAMS | + | NR | NR | NR |
| FDD | NR | NR | ++ | – |
| FIDE | NR | NR | NR | ++ |
| LCCP | NR | NR | ++ | ++ |
| mDawn | + | NR | NR | ++ |
| PMFF | NR | + | – | NR |
| PROMOTE + SUPPORT | NR | NR | – | NR |
| SHARE plus | + | + | NR | NR |
| TExT-MED + FANS | NR | ++ | – | + |
| New social support relationship | ||||
| CGM + OPSC | ++ | NR | NR | + |
| CO-IMPACT | NR | NR | NR | ++ |
| D-NET | – | NR | NR | – |
| Fitbit + Friends | – | NR | NR | + |
| FTA | + | NR | NR | + |
| iDecide | NR | ++ | NR | – |
| InquisitHealth | NR | NR | NR | ++ |
| Internet Mentoring Program | – | NR | ++ | – |
| Low-Carb Program | NR | NR | NR | ++ |
| MoDIAB | – | ++ | – | + |
| Reciprocal Peer Support | ++ | ++ | ++ | ++ |
| TangTangQuan | NR | NR | NR | ++ |
| Virtual Clinic | – | NR | NR | – |
| Women to Women Diabetes Project | – | – | NR | NR |
NR, not reported; −, no difference between groups or pre/post; +, non-significant improvement or qualitative findings only; ++, significant difference between groups or pre/post. CGM, Continuous Glucose Monitor; CD, computer compact disc; SMS, Short Message Service; FAMS, Family-focused Add-on to Motivate Self-care; FDD, Family Defeating Diabetes; FIDE, Family-Integrated Diabetes Educational Programme; LCCP, Lilly Connected Care Program; PMFF, Phone Messaging + Friends/Family; TExT-MED + FANS, Trial to Examine Text-Messaging in Emergency patients with Diabetes + Family and friends Network Support; OPSC, Online Peer Support Community; CO-IMPACT, Caring Others Increasing Engagement in Patient Aligned Care Teams; D-NET, Diabetes Network; FTA, FewTouch Application; MoDIAB, Mothers and Diabetes Web.
Table 3
| Intervention name | Psycho-social outcomes | Behavioral outcomes | Clinical outcomes |
|---|---|---|---|
| Perception of support measured | |||
| CD Training + SMS | ++ | ++ | ++ |
| CGM + OPSC | ++ | NR | + |
| iDecide | NR | NR | - |
| PMFF | NR | – | NR |
| SHARE plus | + | NR | NR |
| Reciprocal Peer Support | ++ | ++ | ++ |
| TangTangQuan | NR | NR | ++ |
| TExT-MED + FANS | − | ++ | + |
| Women to Women Diabetes Project | – | NR | NR |
| Perception of support not measured | |||
| CarePartners | NR | + | ++ |
| CGM Share | NR | NR | ++ |
| CO-IMPACT | ++ | ++ | - |
| D-NET | − | NR | − |
| e-Healthystrides | NR | + | + |
| FAMS | + | NR | NR |
| FDD | NR | ++ | − |
| FIDE | NR | NR | ++ |
| Fitbit + Friends | – | – | – |
| FTA | – | – | – |
| InquisitHealth | NR | NR | ++ |
| Internet Mentoring Program | − | ++ | − |
| LCCP | NR | ++ | ++ |
| Low-Carb Program | NR | NR | ++ |
| mDawn | + | NR | ++ |
| MoDIAB | − | − | + |
| PROMOTE + SUPPORT | NR | − | NR |
| Virtual Clinic | − | NR | − |
NR, not reported; −, no difference between groups or pre/post; +, non-significant improvement or qualitative findings only; ++, significant difference between groups or pre/post. CD, computer compact disc; SMS, Short Message Service; CGM, Continuous Glucose Monitor; OPSC, Online Peer Support Community; PMFF, Phone Messaging + Friends/Family; TExT-MED + FANS, Trial to Examine Text-Messaging in Emergency patients with Diabetes + Family and friends Network Support; CO-IMPACT, Caring Others Increasing Engagement in Patient Aligned Care Teams; D-NET, Diabetes Network; FAMS, Family-focused Add-on to Motivate Self-care; FDD, Family Defeating Diabetes; FIDE, Family-Integrated Diabetes Educational Programme; FTA, FewTouch Application; LCCP, Lilly Connected Care Program; MoDIAB, Mothers and Diabetes Web.
Table 4
| Intervention name | Social support domains | |||
|---|---|---|---|---|
| Informational | Tangible | Appraisal | Emotional | |
| Explicitly defined | ||||
| CarePartners | ● | ● | ● | |
| D-NET | ● | ● | ||
| InquisitHealth | ● | ● | ● | |
| PMFF | ● | ● | ● | |
| TExT-MED + FANS | ● | ● | ● | |
| TangTangQuan | ● | ● | ● | |
| Women to Women Diabetes Project | ● | ● | ||
| Implicitly defined | ||||
| CGM + OPSC | ● | ● | ● | |
| CGM Share | ● | |||
| CO-IMPACT | ● | ● | ● | |
| e-Healthystrides | ● | ● | ● | |
| FAMS | ● | ● | ||
| FIDE | ● | |||
| FTA | ● | |||
| iDecide | ● | |||
| Internet Mentoring Program | ● | ● | ||
| LCCP | ● | ● | ● | |
| MoDIAB | ● | ● | ||
| PROMOTE + SUPPORT | ● | |||
| Reciprocal Peer Support | ● | |||
| SHARE plus | ● | ● | ● | |
| Virtual Clinic | ● | |||
| Undefined | ||||
| CD Training + SMS | Undefined domains | |||
| FDD | Undefined domains | |||
| Fitbit + Friends | Undefined domains | |||
| Low-Carb Program | Undefined domains | |||
| mDawn | Undefined domains | |||
●, social support domain is specified within intervention. D-NET, Diabetes Network; PMFF, Phone Messaging + Friends/Family; TExT-MED + FANS, Trial to Examine Text-Messaging in Emergency patients with Diabetes + Family and friends Network Support; CGM, Continuous Glucose Monitor; OPSC, Online Peer Support Community; CO-IMPACT, Caring Others Increasing Engagement in Patient Aligned Care Teams; FAMS, Family-focused Add-on to Motivate Self-care; FIDE, Family-Integrated Diabetes Educational Programme; FTA, FewTouch Application; LCCP, Lilly Connected Care Program; MoDIAB, Mothers and Diabetes Web; CD, computer compact disc; SMS, Short Message Service; FDD, Family Defeating Diabetes.
Lastly, the heterogeneity of findings did not appear to follow a pattern of small sample studies with inflated results, quasi-experimental, or inadequately controlled trials overestimating the impact of increasing social support via ICT (see Table 5). Examining the pattern of outcomes when viewing studies by size and study design did not clearly indicate that a study design was driving positive findings for any intervention. Interventions that have been tested in quasi-experimental and RCT designs were only shown in the RCT area.
Table 5
| Intervention name | N | Psycho-social outcomes | Perceived support | Behavioral outcomes | Clinical outcomes |
|---|---|---|---|---|---|
| RCT: support vs. patient alone | |||||
| CarePartners | 301 | NR | NR | + | ++ |
| D-NET | 320 | − | NR | NR | − |
| Fitbit + Friends | 120 | – | NR | – | – |
| Internet Mentoring Program | 57 | − | NR | ++ | − |
| PMFF | 42 | NR | + | – | NR |
| PROMOTE + SUPPORT | 200 | NR | NR | − | NR |
| Reciprocal Peer Support | 244 | ++ | ++ | ++ | ++ |
| TExT-MED + FANS | 44 | NR | − | ++ | + |
| RCT: support vs. usual care | |||||
| CD Training + SMS | 76 | ++ | ++ | ++ | ++ |
| CO-IMPACT | 239 | ++ | NR | ++ | - |
| FDD | 170 | NR | NR | ++ | − |
| iDecide | 255 | - | ++ | NR | - |
| MoDIAB | 174 | − | ++ | − | + |
| Women to Women Diabetes Project | 30 | – | – | NR | NR |
| Quasi experimental | |||||
| CGM + OPSC | 34 | ++ | NR | NR | + |
| CGM Share | 28 | NR | NR | NR | ++ |
| e-Healthystrides | 264 | NR | NR | + | + |
| FAMS | 19 | + | NR | NR | NR |
| FIDE | 170 | NR | NR | NR | ++ |
| FTA | 7 | + | NR | NR | + |
| InquisitHealth | 618 | NR | NR | NR | ++ |
| LCCP | 780 | NR | NR | ++ | ++ |
| Low-Carb Program | 1000 | NR | NR | NR | ++ |
| mDawn | 56 | + | NR | NR | ++ |
| SHARE plus | 34 | + | + | NR | NR |
| TangTangQuan | 693 | NR | NR | NR | ++ |
| Virtual Clinic | 17 | − | NR | NR | − |
NR, not reported; −, no difference between groups or pre/post; +, non-significant improvement or qualitative findings only; ++, significant difference between groups or pre/post. RCT, randomized controlled trial; D-NET, Diabetes Network; PMFF, Phone Messaging + Friends/Family; TExT-MED + FANS, Trial to Examine Text-Messaging in Emergency patients with Diabetes + Family and friends Network Support; CD, computer compact disc; SMS, Short Message Service; CO-IMPACT, Caring Others Increasing Engagement in Patient Aligned Care Teams; FDD, Family Defeating Diabetes; MoDIAB, Mothers and Diabetes Web; CGM, Continuous Glucose Monitor; OPSC, Online Peer Support Community; FAMS, Family-focused Add-on to Motivate Self-care; FTA, FewTouch Application; FIDE, Family-Integrated Diabetes Educational Programme; LCCP, Lilly Connected Care Program.
Discussion
In this scoping review of ICT interventions to improve social support for self-management of diabetes, we identified the most common ICT modalities, trends in outcomes (psycho-social, behavioral, and clinical), the social support domains most commonly emphasized, and the types of supporters most often engaged. The most commonly used ICT modality was app- and web forum-based interventions; this strategy was also used in combination with text messaging and Internet-connected medical devices. Outcomes tended to be neutral to positive with a general tendency towards improved psychosocial and clinical outcomes, however these outcomes were heterogeneously reported. The most commonly targeted social support domain was emotional support (fifteen out of 27 interventions). Interventions were balanced between engaging current supporters of patients and developing new social support relationships. We found few patterns of study designs that showed trends towards more effective interventions, apart from including an explicit measurement of social support. In short, there is no dominant direction that interventions are currently headed, nor a consistent pattern of results to guide intervention developers in future endeavors.
The only study design pattern identified that appeared to impact intervention efficacy was the inclusion of a measurement of perceived social support. Five out of the nine interventions studied that included measures of perceived support showed improvements in clinical outcomes (44,47,48,51,52,60). Lari et al. and Heisler et al. showed both significant improvements in perception of social support and clinical outcomes (47,48,60). Reciprocal Peer Support showed an improvement in A1c, the most validated clinical outcomes in self-management of diabetes, by incorporating peers with diabetes into an IVR-based intervention. Impressively, this intervention outperformed case management by a nurse, a very resource intensive design. Lari et al. (60) showed improvements in perception of social support from friends as well as family, and a significant improvement in perceived health (measured by SF-12) for patients receiving the intervention over usual care. In TExT-MED + FANS described by Burner et al. (51), the pilot study did not show any differences in perceived support between the intervention arm and an active control arm, but did see a trend toward improved A1c, with a 0.8 mean difference in change scores between the groups. Mayberry et al. (21) noted the aspects of social support by measuring the helpful and harmful aspects of family/friend involvement. Moreover, Allen et al. stated that 63% of people with diabetes and 63% of care partners noted an improvement in social and interpersonal support (44). This pattern highlights what has been seen in other chronic diseases; that the perception of social support impacts patients’ motivation and capacity to care for themselves. Our findings that interventions that purposely measured perceived social support all found positive (or trends towards positive) changes in clinical and patient centered outcomes emphasize the importance of theory-driven intervention design.
Interestingly, in this review of increasing social support, few investigators made their social support models explicit. Only seven interventions described and presented clear models for the planned increase in social support (Table 4). From the descriptions of the other interventions, potential theoretical models and domains of social support could be determined, however without explicit description, it was difficult to know what the authors initially intended. From our data extraction, the most commonly targeted social support domain was emotional support (fifteen out of 27 interventions), followed by informational support (fourteen out of 27 interventions) and appraisal support (fourteen out of 27 interventions). Tangible support was rarely targeted (four out of 27 interventions). The emphasis on emotional support is likely appropriate, given that patients have both informal and formal sources of information, but need the emotional support from loved ones (63). The perceived benefits of emotional and informational support seen in our review highlight prior findings of new support relationships via web forums as particularly supportive in informational and emotional support domains (64).
The lack of emphasis on tangible support should be further examined, as patients with diabetes often describe issues of medication costs, frequent travel to medical appointments, family pressures such as childcare, and difficulty with frequent self-monitoring of glucose as barriers to healthy behavior choices (65,66). While designing interventions to increase tangible support can be difficult because it may require tailoring to an individual patient’s needs, this may be an avenue to increase intervention efficacy. The focus of several interventions on appraisal support, particularly regarding medication taking, must be carefully examined. Family members who take on too much of a role as a “diabetes cop” may paradoxically decrease healthy behaviors in their loved ones with diabetes (67).
While this scoping review focused on scalable ICT-based social support interventions for people with diabetes, several notable interventions were identified in our search that did not meet inclusion criteria. Some focused on diabetes prevention, such as the PULSE Program (T2DM Prevention Using LifeStyle Education) described by Aguiar et al. (68); tested in an RCT, the PULSE Program emphasized gender congruent peer support program and resulted in weight loss and reduced waist circumference. Many interventions screened utilized ICT technologies in synchronous training of support people, peer coaching or healthcare delivery, such as the interventions described by Higa et al. (69), Zupa et al. (70), Wilczynska et al. (71), Johnson et al. (72), and Lewinski et al. (73). However, we excluded these established but less scalable forms of ICT delivered social support interventions to focus on the potential impact of scalable technologies, highlighting their cost-effectiveness.
This scoping review of ICT interventions was limited by the heterogeneity of outcome reporting, the various study designs employed, and the intermittent theoretical basis of the interventions. Over half of the articles did not include potential mediators of healthy behaviors or clinical outcomes, such as self-efficacy, psychological distress, or social support. Given the high potential for the Hawthorne effect in health behavior interventions, particularly in diabetes, this lack of appropriate control lends itself to significant potential bias, particularly in interpreting positive findings (48,49). Additionally, the above described lack of explicit theoretical basis for the large majority of the interventions made interpreting null findings prone to reader assumptions of where an intervention failed to effect change. Moreover, the method used for this scoping review only allowed for an article to be excluded on the basis of one category and did not account for the overlapping of exclusion criteria.
Outside of the limitations of this scoping review, the widespread adoption of mHealth technologies has transformed healthcare, but comes with challenges (74). One issue is the digital divide, where individuals lacking access to smartphones or stable Internet connections are excluded from the benefits of mHealth solutions, creating disparities in healthcare access (74). Privacy and security concerns also loom large; sensitive health data transmitted through mobile devices are vulnerable to breaches, raising apprehensions about confidentiality (75). Moreover, the rapid evolution of mHealth apps can lead to compatibility issues with various devices and operating systems, causing user frustration and hindering seamless integration into daily routines (76). Additionally, there is a risk of information overload, where individuals may be inundated with health-related data and struggle to discern relevant, accurate information amidst the vast volume of content (77). Addressing these technology-related challenges is crucial to ensuring that mHealth technologies are universally accessible, secure, user-friendly, and genuinely enhance overall healthcare experiences.
The current interventions employing ICT technology to increase social support and improve self-management for adult patients with diabetes were neither consistently theory-based nor were consistent outcomes used between studies. This created difficulty in comparing interventions, and generated confusion when an intervention failed to have an effect on clinical outcomes. While theory-based interventions have been shown to have greater impact and allow for a deeper understanding of the health behavior change being targeted, many current interventions drew from multiple disciplines and were not rooted in any theoretical model. Without this basis, it was difficult to determine what best practices were in this field and how to move forward with future interventions. As ICT developers, researchers, and clinicians continue to converge on this important disease area, it is important that underlying theories are made clear.
Conclusions
This review highlights the potential benefits of incorporating social support enhancement for self-management interventions for adults with diabetes, particularly via ICT. Further exploration of the most effective ICT modalities for changing health beliefs, behaviors, and clinical outcomes is needed. Additionally, the domains of social support targeted in these interventions must be more explicitly defined and measured to identify the most effective strategies. Overall, incorporating ICT into social support interventions shows promise in enhancing diabetes self-management for adults. By harnessing the cost-effectiveness and scalability of ICT, while also maintaining a personal touch supplied by an existing or new supporter, these interventions have the potential to improve the management of diabetes and reduce the burden of complications, thereby bridging gaps in access to care.
Acknowledgments
The authors would like to extend their sincerest gratitude and thanks for the invaluable assistance of Caroline Marshall for her consultation as a research librarian in assisting us in library technology and conducting our literature searches.
Funding: This work was partially supported by
Footnote
Reporting Checklist: The authors have completed the PRISMA-ScR reporting checklist. Available at https://mhealth.amegroups.com/article/view/10.21037/mhealth-23-34/rc
Peer Review File: Available at https://mhealth.amegroups.com/article/view/10.21037/mhealth-23-34/prf
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at https://mhealth.amegroups.com/article/view/10.21037/mhealth-23-34/coif). E.B. reports that she received training grant (No. K23DK106538) from NIH NIDDK. In her role with Agile Health as an advisory board member, she has given advice on scalable ICT solutions for tobacco addiction, which does not directly relate to this scoping review and does not present a conflict of interest. She is also the Vice Chair of the Society for Academic Emergency Medicine Grants Committee and her role as Vice Chair of the SAEMF Grants Committee does not conflict with this review. The other author has no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Khan MAB, Hashim MJ, King JK, et al. Epidemiology of Type 2 Diabetes - Global Burden of Disease and Forecasted Trends. J Epidemiol Glob Health 2020;10:107-11. [Crossref] [PubMed]
- Lazzarini PA, Cramb SM, Golledge J, et al. Global trends in the incidence of hospital admissions for diabetes-related foot disease and amputations: a review of national rates in the 21st century. Diabetologia 2023;66:267-87. [Crossref] [PubMed]
- Kovesdy CP. Epidemiology of chronic kidney disease: an update 2022. Kidney Int Suppl (2011) 2022;12:7-11. [Crossref] [PubMed]
- Wong TY, Sabanayagam C. Strategies to Tackle the Global Burden of Diabetic Retinopathy: From Epidemiology to Artificial Intelligence. Ophthalmologica 2020;243:9-20. [Crossref] [PubMed]
- Standards of Care in Diabetes-2023 Abridged for Primary Care Providers. Clin Diabetes 2022;41:4-31. [PubMed]
- Lidegaard LP, Schwennesen N, Willaing I, et al. Barriers to and motivators for physical activity among people with Type 2 diabetes: patients' perspectives. Diabet Med 2016;33:1677-85. [Crossref] [PubMed]
- Saha S. Compliance and barriers to self-monitoring of blood glucose in patients with gestational diabetes mellitus: A systematic review. Int J Health Sci (Qassim) 2019;13:44-52. [PubMed]
- Raaijmakers LG, Hamers FJ, Martens MK, et al. Perceived facilitators and barriers in diabetes care: a qualitative study among health care professionals in the Netherlands. BMC Fam Pract 2013;14:114. [Crossref] [PubMed]
- Powers MA, Bardsley JK, Cypress M, et al. Diabetes Self-management Education and Support in Adults With Type 2 Diabetes: A Consensus Report of the American Diabetes Association, the Association of Diabetes Care & Education Specialists, the Academy of Nutrition and Dietetics, the American Academy of Family Physicians, the American Academy of PAs, the American Association of Nurse Practitioners, and the American Pharmacists Association. Diabetes Care 2020;43:1636-49. [Crossref] [PubMed]
- Davis J, Fischl AH, Beck J, et al. 2022 National Standards for Diabetes Self-Management Education and Support. Sci Diabetes Self Manag Care 2022;48:44-59. [Crossref] [PubMed]
- Stopford R, Winkley K, Ismail K. Social support and glycemic control in type 2 diabetes: a systematic review of observational studies. Patient Educ Couns 2013;93:549-58. [Crossref] [PubMed]
- Clayton C, Motley C, Sakakibara B. Enhancing Social Support Among People with Cardiovascular Disease: a Systematic Scoping Review. Curr Cardiol Rep 2019;21:123. [Crossref] [PubMed]
- Gupta L, Khandelwal D, Lal PR, et al. Factors Determining the Success of Therapeutic Lifestyle Interventions in Diabetes - Role of Partner and Family Support. Eur Endocrinol 2019;15:18-24. [Crossref] [PubMed]
- Koetsenruijter J, van Eikelenboom N, van Lieshout J, et al. Social support and self-management capabilities in diabetes patients: An international observational study. Patient Educ Couns 2016;99:638-43. [Crossref] [PubMed]
- Kirk JK, Ebert CN, Gamble GP, et al. Social support strategies in adult patients with diabetes: a review of strategies in the USA and Europe. Expert Rev Endocrinol Metab 2013;8:379-89. [Crossref] [PubMed]
- van Dam HA, van der Horst FG, Knoops L, et al. Social support in diabetes: a systematic review of controlled intervention studies. Patient Educ Couns 2005;59:1-12. [Crossref] [PubMed]
- Strom JL, Egede LE. The impact of social support on outcomes in adult patients with type 2 diabetes: a systematic review. Curr Diab Rep 2012;12:769-81. [Crossref] [PubMed]
- Spencer-Bonilla G, Ponce OJ, Rodriguez-Gutierrez R, et al. A systematic review and meta-analysis of trials of social network interventions in type 2 diabetes. BMJ Open 2017;7:e016506. [Crossref] [PubMed]
- House JS, Umberson D, Landis KR. Structures and processes of social support. Annu Rev Sociol 1988;14:293-318. [Crossref]
- Heisler M. Overview of peer support models to improve diabetes self-management and clinical outcomes. Diabetes Spectr 2007;20:214-21. [Crossref]
- Mayberry LS, Berg CA, Harper KJ, et al. The Design, Usability, and Feasibility of a Family-Focused Diabetes Self-Care Support mHealth Intervention for Diverse, Low-Income Adults with Type 2 Diabetes. J Diabetes Res 2016;2016:7586385. [Crossref] [PubMed]
- Ojewale LY, Oluwatosin OA. Family-integrated diabetes education for individuals with diabetes in South-west Nigeria. Ghana Med J 2022;56:276-84. [Crossref] [PubMed]
- Wang Y, Min J, Khuri J, et al. Effectiveness of Mobile Health Interventions on Diabetes and Obesity Treatment and Management: Systematic Review of Systematic Reviews. JMIR Mhealth Uhealth 2020;8:e15400. [Crossref] [PubMed]
- Brew-Sam N, Chhabra M, Parkinson A, et al. Experiences of Young People and Their Caregivers of Using Technology to Manage Type 1 Diabetes Mellitus: Systematic Literature Review and Narrative Synthesis. JMIR Diabetes 2021;6:e20973. [Crossref] [PubMed]
- McGowan J, Straus S, Moher D, et al. Reporting scoping reviews-PRISMA ScR extension. J Clin Epidemiol 2020;123:177-9. [Crossref] [PubMed]
- Glasgow RE, Barrera M Jr, McKay HG, et al. Social support, self-management, and quality of life among participants in an internet-based diabetes support program: a multi-dimensional investigation. Cyberpsychol Behav 1999;2:271-81. [Crossref] [PubMed]
- Smith L, Weinert C. Telecommunication support for rural women with diabetes. Diabetes Educ 2000;26:645-55. [Crossref] [PubMed]
- McKay HG, Glasgow RE, Feil EG, et al. Internet-based diabetes self-management and support: Initial outcomes from the diabetes network project. Rehabil Psychol 2002;47:31-48. [Crossref]
- Glasgow RE, Boles SM, McKay HG, et al. The D-Net diabetes self-management program: long-term implementation, outcomes, and generalization results. Prev Med 2003;36:410-9. [Crossref] [PubMed]
- Barrera M Jr, Glasgow RE, McKay HG, et al. Do Internet-based support interventions change perceptions of social support?: An experimental trial of approaches for supporting diabetes self-management. Am J Community Psychol 2002;30:637-54. [Crossref] [PubMed]
- Jennings A, Powell J, Armstrong N, et al. A virtual clinic for diabetes self-management: pilot study. J Med Internet Res 2009;11:e10. [Crossref] [PubMed]
- Powell J, Jennings A, Armstrong N, et al. Pilot study of a virtual diabetes clinic: satisfaction and usability. J Telemed Telecare 2009;15:150-2. [Crossref] [PubMed]
- Chomutare T, Tatara N, Årsand E, et al. Designing a diabetes mobile application with social network support. Stud Health Technol Inform 2013;188:58-64. [PubMed]
- Heisler M, Choi H, Palmisano G, et al. Comparison of community health worker-led diabetes medication decision-making support for low-income Latino and African American adults with diabetes using e-health tools versus print materials: a randomized, controlled trial. Ann Intern Med 2014;161:S13-22. [Crossref] [PubMed]
- Linden K, Berg M, Adolfsson A, et al. Person-centred, web-based support in pregnancy and early motherhood for women with Type 1 diabetes mellitus: a randomized controlled trial. Diabet Med 2018;35:232-41. [Crossref] [PubMed]
- Berg M, Linden K, Adolfsson A, et al. Web-Based Intervention for Women With Type 1 Diabetes in Pregnancy and Early Motherhood: Critical Analysis of Adherence to Technological Elements and Study Design. J Med Internet Res 2018;20:e160. [Crossref] [PubMed]
- Saslow LR, Summers C, Aikens JE, et al. Outcomes of a Digitally Delivered Low-Carbohydrate Type 2 Diabetes Self-Management Program: 1-Year Results of a Single-Arm Longitudinal Study. JMIR Diabetes 2018;3:e12. [Crossref] [PubMed]
- Heisler M, Choi H, Mase R, et al. Effectiveness of Technologically Enhanced Peer Support in Improving Glycemic Management Among Predominantly African American, Low-Income Adults With Diabetes. Diabetes Educ 2019;45:260-71. [Crossref] [PubMed]
- Pemu P, Josiah Willock R, Alema-Mensa E, et al. Achieving Health Equity with e-Healthystrides©: Patient Perspectives of a Consumer Health Information Technology Application. Ethn Dis 2019;29:393-404. [Crossref] [PubMed]
- Zheng XY, Yang DZ, Liu ZY, et al. The effect of mobile application based interactive peer support on glycemic control in patients with type 1 diabetes mellitus. Zhonghua Nei Ke Za Zhi 2019;58:889-93. [PubMed]
- Liu Z, Wang C, Yang D, et al. High engagement in mobile peer support is associated with better glycemic control in type 1 diabetes: A real-world study. J Diabetes Investig 2022;13:1914-24. [Crossref] [PubMed]
- Lyles CR, Sarkar U, Patel U, et al. Real-world insights from launching remote peer-to-peer mentoring in a safety net healthcare delivery setting. J Am Med Inform Assoc 2021;28:365-70. [Crossref] [PubMed]
- Zhang Y, Liu C, Luo S, et al. Effectiveness of the Family Portal Function on the Lilly Connected Care Program (LCCP) for Patients With Type 2 Diabetes: Retrospective Cohort Study With Propensity Score Matching. JMIR Mhealth Uhealth 2021;9:e25122. [Crossref] [PubMed]
- Allen NA, Litchman ML, Chamberlain J, et al. Continuous Glucose Monitoring Data Sharing in Older Adults With Type 1 Diabetes: Pilot Intervention Study. JMIR Diabetes 2022;7:e35687. [Crossref] [PubMed]
- Litchman ML, Ng A, Sanchez-Birkhead A, et al. Combining CGM and an Online Peer Support Community for Hispanic Adults with T2D: A Feasibility Study. J Diabetes Sci Technol 2022;16:866-73. [Crossref] [PubMed]
- Sklar J, Pyle L, Snell-Bergeon JK, et al. Glycemic variability and indices of glycemic control among pregnant women with type 1 diabetes (T1D) based on the use of continuous glucose monitoring share technology. J Matern Fetal Neonatal Med 2022;35:8968-74. [Crossref] [PubMed]
- Heisler M, Piette JD. "I help you, and you help me": facilitated telephone peer support among patients with diabetes. Diabetes Educ 2005;31:869-79. [Crossref] [PubMed]
- Heisler M, Vijan S, Makki F, et al. Diabetes control with reciprocal peer support versus nurse care management: a randomized trial. Ann Intern Med 2010;153:507-15. [Crossref] [PubMed]
- Rosland AM, Piette JD, Trivedi R, et al. Effectiveness of a Health Coaching Intervention for Patient-Family Dyads to Improve Outcomes Among Adults With Diabetes: A Randomized Clinical Trial. JAMA Netw Open 2022;5:e2237960. [Crossref] [PubMed]
- Reese PP, Kessler JB, Doshi JA, et al. Two Randomized Controlled Pilot Trials of Social Forces to Improve Statin Adherence among Patients with Diabetes. J Gen Intern Med 2016;31:402-10. [Crossref] [PubMed]
- Burner E, Lam CN, DeRoss R, et al. Using Mobile Health to Improve Social Support for Low-Income Latino Patients with Diabetes: A Mixed-Methods Analysis of the Feasibility Trial of TExT-MED + FANS. Diabetes Technol Ther 2018;20:39-48. [Crossref] [PubMed]
- Mayberry LS, Berg CA, Greevy RA, et al. Mixed-Methods Randomized Evaluation of FAMS: A Mobile Phone-Delivered Intervention to Improve Family/Friend Involvement in Adults' Type 2 Diabetes Self-Care. Ann Behav Med 2021;55:165-78. [Crossref] [PubMed]
- Roddy MK, Nelson LA, Greevy RA, et al. Changes in family involvement occasioned by FAMS mobile health intervention mediate changes in glycemic control over 12 months. J Behav Med 2022;45:28-37. [Crossref] [PubMed]
- Aikens JE, Zivin K, Trivedi R, et al. Diabetes self-management support using mHealth and enhanced informal caregiving. J Diabetes Complications 2014;28:171-6. [Crossref] [PubMed]
- Aikens JE, Trivedi R, Aron DC, et al. Integrating support persons into diabetes telemonitoring to improve self-management and medication adherence. J Gen Intern Med 2015;30:319-26. [Crossref] [PubMed]
- Aikens JE, Rosland AM, Piette JD. Improvements in illness self-management and psychological distress associated with telemonitoring support for adults with diabetes. Prim Care Diabetes 2015;9:127-34. [Crossref] [PubMed]
- Suh S, Jean C, Koo M, et al. A randomized controlled trial of an internet-based mentoring program for type 1 diabetes patients with inadequate glycemic control. Diabetes Metab J 2014;38:134-42. [Crossref] [PubMed]
- Ho K, Newton L, Boothe A, et al. mobile Digital Access to a Web-enhanced Network (mDAWN): Assessing the Feasibility of Mobile Health Tools for Self-Management of Type-2 Diabetes. AMIA Annu Symp Proc 2015;2015:621-9. [PubMed]
- Ramirez M, Wu S. Phone Messaging to Prompt Physical Activity and Social Support Among Low-Income Latino Patients With Type 2 Diabetes: A Randomized Pilot Study. JMIR Diabetes 2017;2:e8. [Crossref] [PubMed]
- Lari H, Noroozi A, Tahmasebi R. Impact of Short Message Service (SMS) Education Based on a Health Promotion Model on the Physical Activity of Patients with Type II Diabetes. Malays J Med Sci 2018;25:67-77. [Crossref] [PubMed]
- McManus R, Miller D, Mottola M, et al. Translating Healthy Living Messages to Postpartum Women and Their Partners After Gestational Diabetes (GDM): Body Habitus, A1C, Lifestyle Habits, and Program Engagement Results From the Families Defeating Diabetes (FDD) Randomized Trial. Am J Health Promot 2018;32:1438-46. [Crossref] [PubMed]
- Lystrup R, Carlsen D, Sharon DJ, et al. Wearable and interactive technology to share fitness goals results in weight loss but not improved diabetes outcomes. Obes Res Clin Pract 2020;14:443-8. [Crossref] [PubMed]
- Longo DR, Schubert SL, Wright BA, et al. Health information seeking, receipt, and use in diabetes self-management. Ann Fam Med 2010;8:334-40. [Crossref] [PubMed]
- DeHoff BA, Staten LK, Rodgers RC, et al. The Role of Online Social Support in Supporting and Educating Parents of Young Children With Special Health Care Needs in the United States: A Scoping Review. J Med Internet Res 2016;18:e333. [Crossref] [PubMed]
- Adu MD, Malabu UH, Malau-Aduli AEO, et al. Enablers and barriers to effective diabetes self-management: A multi-national investigation. PLoS One 2019;14:e0217771. [Crossref] [PubMed]
- An Effective Model of Diabetes Care and Education: Revising the AADE7 Self-Care Behaviors Diabetes Educ 2020;46:139-60. [Crossref] [PubMed]
- Mayberry LS, Osborn CY. Family support, medication adherence, and glycemic control among adults with type 2 diabetes. Diabetes Care 2012;35:1239-45. [Crossref] [PubMed]
- Aguiar EJ, Morgan PJ, Collins CE, et al. Process Evaluation of the Type 2 Diabetes Mellitus PULSE Program Randomized Controlled Trial: Recruitment, Engagement, and Overall Satisfaction. Am J Mens Health 2017;11:1055-68. [Crossref] [PubMed]
- Higa C, Davidson EJ, Loos JR. Integrating family and friend support, information technology, and diabetes education in community-centric diabetes self-management. J Am Med Inform Assoc 2021;28:261-75. [Crossref] [PubMed]
- Zupa MF, Lee A, Piette JD, et al. Impact of a Dyadic Intervention on Family Supporter Involvement in Helping Adults Manage Type 2 Diabetes. J Gen Intern Med 2022;37:761-8. [Crossref] [PubMed]
- Wilczynska M, Jansson AK, Lubans DR, et al. Physical activity intervention for rural middle-aged and older Australian adults: a pilot implementation study of the ecofit program delivered in a real-world setting. Pilot Feasibility Stud 2021;7:81. [Crossref] [PubMed]
- Johnson C, Feinglos M, Pereira K, et al. Feasibility and preliminary effects of a virtual environment for adults with type 2 diabetes: pilot study. JMIR Res Protoc 2014;3:e23. [Crossref] [PubMed]
- Lewinski AA, Anderson RA, Vorderstrasse AA, et al. Analyzing Unstructured Communication in a Computer-Mediated Environment for Adults With Type 2 Diabetes: A Research Protocol. JMIR Res Protoc 2017;6:e65. [Crossref] [PubMed]
- Scott Kruse C, Karem P, Shifflett K, et al. Evaluating barriers to adopting telemedicine worldwide: A systematic review. J Telemed Telecare 2018;24:4-12. [Crossref] [PubMed]
- Petersen C, DeMuro P. Legal and regulatory considerations associated with use of patient-generated health data from social media and mobile health (mHealth) devices. Appl Clin Inform 2015;6:16-26. [Crossref] [PubMed]
- LeRouge C, Garfield MJ. Crossing the telemedicine chasm: have the U.S. barriers to widespread adoption of telemedicine been significantly reduced? Int J Environ Res Public Health 2013;10:6472-84. [Crossref] [PubMed]
- Sinclair C, Holloway K, Riley G, et al. Online mental health resources in rural Australia: clinician perceptions of acceptability. J Med Internet Res 2013;15:e193. [Crossref] [PubMed]
Cite this article as: Hazime D, Burner E. Social support via Internet communication technology for diabetes self-management: a scoping review. mHealth 2024;10:18.


