Analysis of the virtual healthcare model in Latin America: a systematic review of current challenges and barriers
Highlight box
Key findings
• Few studies have explored the challenges to the implementation of virtual care in Latin American countries.
• In Latin America, connectivity problems, lack of a complete physical examination, issues of privacy, high risk of medical malpractice, and absence of local regulation were the identified barriers and challenges to overcome.
What is known and what is new?
• The implementation and use of virtual care models around the world reflect a high degree of inequity, which varies according to the social, economic, and technological context of each country.
• The findings of this study can serve as a baseline for the generation of interventions and public health policies that favor the consolidation of this model in the region.
What is the implication, and what should change now?
• Strengthening training programs in the use of healthcare technologies, optimizing communication channels, and improving data management and cybersecurity, as well as guaranteeing interoperability with the current system, are essential for expanding the virtual model in Latin American countries.
Introduction
Background
The virtual care model is a safe and reliable alternative for the delivery of health services, with multiple benefits for patients and their families. This model has been a strategy to provide health services closer to the communities while guaranteeing the highest quality and safety standards (1). The virtual care or telemedicine model is the delivery of healthcare services at a distance via technology and the term includes a wide range of applications, such as remote consultations, telerehabilitation, remote monitoring, remote patient education or teleinterpretation (e.g., radiology exams) (2). The virtual care model can be used in all aspects of healthcare, such as prevention, diagnosis, treatment, and follow-up of most medical and surgical conditions. This modality began in the 1970s due to the technological boom of the era, but it was not until the advent of the coronavirus disease 2019 (COVID-19) pandemic that it positioned itself as an optimal alternative for providing specialized care in the management of acute and chronic conditions. For this reason, it is now considered a developing field with exponential growth, both for developed and developing countries (2-4).
Rationale and knowledge
Beyond just performing real-time remote outpatient consultations, virtual care is a model that enables the delivery of comprehensive inpatient care remotely, turning patients’ homes into rooms attached to conventional hospitals. Virtual care has made it possible to reduce hospital length of stay and decrease the risk of nosocomial infections. In fact, patient satisfaction levels with the treatment have increased since the care process of these patients takes place in a familiar environment, achieving better clinical results and more favorable costs for insurers (5-7). In addition, this model of health care can positively reduce the workload of healthcare workers, which translates into a minimization of the risk of burnout syndrome due to fewer hours of face-to-face work (8). Despite the multiple benefits of the virtual care model, its implementation and use around the world reflect a high degree of inequity, which varies according to the social, economic, and technological context of each country (9). In Latin America, prior to the pandemic, the implementation of this model of care was considered low compared to countries such as the United States, Canada, and Europe (3). For example, in countries such as Argentina, Colombia, Mexico, and Costa Rica, less than 30% of hospitals offered virtual care services (10). Although the COVID-19 pandemic forced the adoption of this model, there is still a gap relative to first-world countries, especially after all mobility restrictions imposed during the pandemic were lifted. In addition, the World Health Organization (WHO) in the year 2022 urged decision-makers to consolidate the use of the virtual model to guarantee access and timeliness care for a greater percentage of the population (11). We present this qualitative systematic review in accordance with the PRISMA reporting checklist (available at https://mhealth.amegroups.com/article/view/10.21037/mhealth-23-47/rc) (12).
Objective
The objective of this systematic review was to identify the current barriers to the implementation and consolidation of the virtual healthcare model “telemedicine” in Latin American countries during and after the advent of COVID-19.
Methods
Selection criteria and search strategy
The literature search was conducted through four databases: PubMed, Scopus, Web of Science, and Virtual Health, between February 25 and 26, 2023. The search was performed using a combination of Boolean operators with the following terms: “telemedicine”, “telehealth”, “telecare”, “home care services”, “remote care”, and the name of each Latin American country. The strategy used for the four databases consulted is described in Table S1.
Study selection and data extraction
The identified records were managed with Rayyan software (13). After removing duplicate records, two investigators independently reviewed titles and abstracts to identify those that met the selection criteria described in Table 1. Subsequently, the two authors reviewed the full text of the articles pre-selected for inclusion. When discrepancies existed, these were resolved in the presence of a third reviewer. Quality assessment in the qualitative studies was performed with the tool available in the critical appraisal skill program (CASP) (14). The cross-sectional studies were evaluated with the Newcastle-Ottawa Scale (NOS) (15), and finally, a narrative synthesis of the barriers reported in Latin American countries was performed.
Table 1
| Inclusion criteria |
| Articles focused on describing or discussing the barriers and challenges of the use or implementation of telemedicine or virtual health care in Latin American countries |
| Articles published in English, Spanish, or Portuguese |
| Articles published between January 2020 and January 2023 |
| Original articles and reviews |
| Exclusion criteria |
| Editorials, commentaries, conferences, or articles without statistical or theoretical evidence |
| Articles whose full text could not be obtained |
| Articles that use technological tools for teaching |
Results
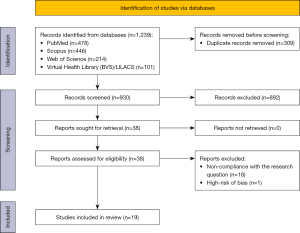
After removing duplicates, the initial search identified a total of 930 articles among the four databases. After reviewing the title and abstract of each article, a total of 38 were pre-selected. Of these, 19 studies met the selection criteria and were included in this review (Figure 1).
Characteristics of the studies
The included studies were published between January 2020 and January 2023. Of the 19 articles, 17 studies were based on data collected in a single country, and two articles performed an analysis of the realities of two or more countries. Most of the studies had a cross-sectional design (n=9), followed by a qualitative design (n=6). Two systematic literature reviews, one mixed-approach study, and one case report were included (Table 2).
Table 2
| First author, year | Country | Journal | Study design | Virtual care intervention assessed | Findings | Limitations of the study |
|---|---|---|---|---|---|---|
| Caetano et al., 2020, (16) | Brazil | Cadernos de Saúde Pública | Systematic review | General virtual care | Limitation for performing a complete and exhaustive physical examination | Only the Brazilian context |
| Limited use in the context of patients with neurological or critical pathologies | ||||||
| Lack of local regulation for the provision of the virtual service | ||||||
| Lack of integration of telemedicine in management guidelines | ||||||
| Lack of standardization of use and adequate structures for virtual care | ||||||
| Lack of implementation of specific applications to provide follow-up and virtual evaluation tools | ||||||
| Lack of information and education on virtual care in the population | ||||||
| Casilang et al., 2020, (17) | Dominican Republic | JMIR Pediatrics and Parenting | Qualitative study | General virtual care/mobile application | Lack of skills in the use of technological tools (e.g., apps, computers, smartphones) | A single hospital center in an urban area |
| High perceived costs | ||||||
| Lack of privacy | ||||||
| Morais et al., 2021, (18) | Brazil | Ciência & Saúde Coletiv | Qualitative study | Remote care | Non-acceptance by patients and/or environment | A single hospital center in an urban area |
| Exposure of health personnel to urban violence | Small sample size (n=8) | |||||
| Pedernera Bradichansky et al., 2021, (19) | Argentina | Archivos Argentinos de Pediatría | Cross-sectional study | General virtual care | Connectivity problems | A single hospital center in an urban area |
| Need for specific technological equipment (e.g., computer with camera) | ||||||
| Escobar et al., 2021, (20) | Colombia | International Journal of Medical Informatics | Cross-sectional study | General virtual care | Connectivity problems | A single hospital center in an urban area |
| Difficulty in making online payments | It uses institutional indicators, not a designed questionnaire | |||||
| Böhm da Costa et al., 2021, (21) | Brazil | International Journal of Medical Informatics | Mixed study | General virtual care | Connectivity problems | Small sample size (n=26) |
| Lack of integration with institutional systems | A single hospital center in an urban area | |||||
| Loza et al., 2021, (22) | Argentina | Medwave | Qualitative study | General virtual care | Lack of technological resources | A single hospital center in an urban area |
| Lack of skill in the use of technological tools (e.g., apps, computers, smartphones) | Phone interviews | |||||
| Limitation for performing a complete and thorough physical examination | ||||||
| Palma et al., 2021, (23) | Argentina | Journal of Pain and Symptom Management | Cross-sectional study | General virtual care | Connectivity problems | A single hospital center in an urban area |
| Catapan et al., 2021, (24) | Brazil | Epidemiologia e Serviços de Saúde | Cross-sectional study | General virtual care | Territorial inequalities in access to information and communication technologies | Ecological approach |
| Chávarri-Guerra et al., 2021, (25) | Mexico | The Oncologist | Cross-sectional study | General virtual care | Lack of privacy | A single hospital center in an urban area |
| Lack of skills in the use of technological tools (e.g., apps, computers, smartphones) | ||||||
| García-Huidobro et al., 2022, (26) | Chile | Health Promotion Practice | Qualitative study | Remote care | Connectivity problems | Email exchanges to measure resource utilization to recruit clinics, providers, and patients. |
| Lack of institutional motivation to create and promote remote care | ||||||
| Lack of integration with the institutional medical record system | ||||||
| Perception of work overload | ||||||
| High costs associated with the implementation process and staff training | ||||||
| Mayela et al., 2022, (27) | Mexico | Neurology India | Cross-sectional study | General virtual care | Lower quality of the doctor-patient relationship | A single hospital center in an urban area |
| Lower perceived consultation time | ||||||
| Michell et al., 2022, (28) | Chile, Brazil and Colombia | Salud Pública de México | Case report | Virtual rehabilitation | High implementation costs | Only the Chilean, Brazilian and Colombian contexts are analyzed |
| Non-reimbursement by insurers to providers for virtual service delivery | ||||||
| Resistance on the part of health personnel to offer virtual care | ||||||
| Poor quality of care associated with technological limitations (e.g., camera resolution, connectivity, interference) | ||||||
| Low perception of therapeutic benefit by patients and health personnel | ||||||
| Lack of privacy | ||||||
| Lack of local regulation for the provision of the virtual service | ||||||
| Gutiérrez et al., 2022, (29) | Colombia | Sustainability | Qualitative study | General virtual care | Lack of resources for the acquisition of specialized software | A single hospital center in an urban area |
| Lack of clarity on the fees associated with virtual services | ||||||
| Limitation for performing a complete and exhaustive physical examination | ||||||
| Lack of clarity on medical liability for possible adverse events and/or medical errors | ||||||
| Piskorz et al., 2022, (30) | Mexico, Argentina, Colombia, Brazil, Venezuela, Guatemala and Paraguay | Blood pressure | Cross-sectional study | General virtual care | Lack of training in the use of the platforms developed for the virtual provision of the service | Voluntary survey with low response rate (3.2% to 24%) |
| Lack of local regulation and clarity on the form of reimbursement/payment by insurers | ||||||
| Sarti et al., 2022, (31) | Brazil | Cadernos de Saúde Pública | Cross-sectional study | General virtual care | Absence of institutional virtual assistance programs | Only one region in Brazil |
| Aliaga-Castillo et al., 2022, (32) | Chile | Musculoskeletal Science and Practice | Qualitative study | Virtual rehabilitation | Lack of specialized equipment at home. | A single hospital center in urban area |
| Shorter perceived consultation time | Small sample size (n=12) | |||||
| Limitation for performing a complete and exhaustive physical examination | ||||||
| In rehabilitation processes, it limits the feedback made by the specialists to the patients | ||||||
| García-Gutiérrez et al., 2023, (33) | Peru | BMC Medical Education | Cross-sectional study | General virtual care | Decreased patient safety | Participants were recruited from a single free online course |
| Lack of privacy | ||||||
| Increases the possibility of medical malpractice | ||||||
| Lack of training during professional training in telemedicine | ||||||
| Alonso et al., 2023, (34) | Argentina | Neurological Sciences | Systematic review/expert consensus | General virtual care | Lack of local regulation for the provision of the virtual service | Only the Argentine context |
| Limitation for performing a complete and thorough physical examination |
General virtual care: remote consultations/teleconsultations, or remote patient education; virtual rehabilitation: home exercises with remote supervision; remote care: home visits and remote patient monitoring.
Individually, barriers to the use of virtual care have been most frequently explored in countries such as Brazil (n=5) and Argentina (n=4), accounting for nearly half of the reported articles. Countries such as Colombia, Chile, Mexico, Peru, and the Dominican Republic were also represented in this review (Table 2). Most of the studies evaluated barriers to the implementation of a virtual care model in general, with a greater emphasis on the implementation of teleconsultations (n=14). The remaining articles were conducted in the context of a home visiting care model supported by technological tools (n=2), telerehabilitation programs (n=2), and a combination of virtual care with a follow-up app (n=1). In summary, the barriers identified were categorized into five major themes: (I) technological and technical issues; (II) absence of a physical examination; (III) patient’s negative perceptions; (IV) negative perceptions among healthcare professionals; and (V) structural obstacles and those associated with the healthcare system. The barriers identified within each category are described below.
Technological and technical issues
Problems associated with Internet access and connectivity (17,19-21,23,26), the need for specialized equipment and software (e.g., smartphone, camera, among others) (16,21,26,29,32), as well as having the technical skills in the use of technological tools to provide and receive virtual service delivery (17,22,25,30,33) were the main barriers associated with the care process in the studies analyzed (n=14). Although the lack of connectivity during virtual care was a recurring complaint among patients, non-attendance at virtual appointments did not exceed 5% of cases (20), but it was recognized as a factor that increases the perception of poor clinical care (21,28). From the point of view of healthcare workers, the lack of specialized software and equipment for the correct professional practice and issues of interoperability with existing institutional programs were identified as factors that affect productivity and generate the perception of work overload due to the additional procedures required compared to face-to-face care (21,26,29). Additionally, because it is not common to receive training in telemedicine during professional training (33), the requirement for additional specialized courses during professional practice was perceived as a constraint to adoption and willingness to adopt the virtual model (30). On the other hand, it was found that in older adults, the lack of skills in the use of technological tools was reported as a barrier to accessing the healthcare system (22). Similarly, the difficulty of making co-payments online was identified as a barrier to access that led to the cancellation of the service (20).
Absence of a physical examination
The limitation of performing a complete and exhaustive physical examination was identified as a barrier in five studies (16,22,29,32,34) mainly when virtual care was used in patients with neurological pathologies, older adults, and in those requiring a physical rehabilitation process. During the diagnostic process of most pathologies, performing a physical examination is important, both to confirm and to rule out suspicion. For example, some authors believe that the use of the virtual care model should not be used initially in the diagnosis of neurological disorders due to the need for physical and cognitive testing to confirm the condition and to evaluate the evolution of patients during follow-up (16,34). In addition, it was also reported that gynecology and dentistry services may be limited during routine practice (21,29). From the patient’s perspective, this barrier also meant that the virtual care model was perceived as insufficient, requiring a complementary face-to-face consultation (22). On the other hand, in rehabilitation programs, although the care modality is a good alternative for follow-up, some patients and physiotherapists reported difficulties in carrying out direct supervision and, consequently, proper feedback (32).
Patient perceptions
Lack of privacy was one of the main barriers expressed by patients due to the risks of cyber-attacks and reliability in handling data and their clinical information (17,28). This aspect was also found to be compromised because some patients reported requiring support from their caregivers during the provision of the service, which diminished the privacy of the information shared with their treating physician and the quality of the physician-patient relationship (25,27). Some patients have the misconception belief that the virtual care model is not good for therapeutic benefit (22,28). In the study by Morais et al. (18) which included a face-to-face encounter for home health care, some patients or caregivers showed resistance to accepting healthcare staff inside their homes because they believed their privacy is violated. Another perception reported was the perceived high costs due to the need to pay for monthly internet or cell phone services (17), as well as the perception of shorter consultation time (27,32). These barriers may be attributed to the lack of implementation of patient and clinical staff education programs on the benefits and advantages of the virtual care model (16).
Perceptions of healthcare professionals
Four studies identified barriers to the use of the virtual care model associated with healthcare personnel’s beliefs or perceptions about service delivery (18,28,29,32). Among clinicians, a concern about the benefit or effectiveness of the care model in treating patients’ health conditions was identified (28), which consequently led to an increased perception of the risk of committing medical malpractice and jeopardizing patient safety (33). In the context of performing specialized teleconsultation with support from a general practitioner at the remote site of care, a concern was found regarding the use of this model by specialists due to shared medical responsibility (29). Additionally, in two studies, clinicians also reported a lack of privacy during care as a barrier to its use (28,33). In the virtual model that includes face-to-face follow-up in patients’ homes, exposure to urban violence was a barrier reported by healthcare workers in Brazil (18).
Structural barriers associated to the healthcare system
The need for specific local laws to regulate the provision of virtual services, including the process of implementation, use, and integration with the current model, was identified as a common barrier among Latin American countries (16,28,30,34). This was reflected in the various problems encountered concerning the rates established and the reimbursements offered by the insurers to the hospital institutions (28-30). Gutiérrez et al. (29) reported that the billing process was the greatest obstacle identified due to the absence of regulations in Colombia governing service rates. On the other hand, the lack of motivation and standardized programs within health institutions was also a reported barrier to the use of the virtual model (26,31). For example, in Brazil, the prevalence of use during primary care was higher in hospitals with institutional programs (73.3% vs. 32.7%) (31), which had trained personnel and the necessary equipment for the adequate provision of virtual services. The high costs associated with the acquisition of specialized equipment and software, as well as the training of health personnel, were another barrier identified for the implementation of virtual care in Latin America (26,28). In addition, the existence of structural inequalities and access to information and communication tools is also a limitation in guaranteeing the use of virtual care throughout the territories (24).
Discussion
Key findings
This is the first systematic review performed with studies conducted in Latin America that reports on barriers to the implementation of the virtual care or telemedicine model in the region. Specifically, the aim was to explore the main challenges to improve the coverage, in order to serve as a baseline for the generation of interventions and public health policies that favor the consolidation of this model. The findings from this research can help to design different strategies seeking to overcome the identified challenges.
Despite substantial interest and investment in virtual care by governments in developed and developing countries, widespread adoption was modest before the pandemic. As the COVID-19 pandemic evolved, the main health actors were pressured to have to use virtual care to attend the health needs of patients and comply with the isolation regulations imposed by governments. Today, virtual care should not be treated differently from other elements of the health care experience, primarily because it has proven to be a positive experience for patients and providers, with better health outcomes and lower costs (35).
Strengths and limitations
The main limitation of this review is the design of the included studies because most were conducted in a single hospital center, in specific areas of healthcare, and with limited sample sizes. Therefore, the findings summarized here may not reflect the opinion of the entire region. Furthermore, no published studies were found for all the countries, which limits the generalizability of the findings. During the literature search, only studies conducted in the context of outpatient care were identified, and consequently, it was not possible to assess the virtual care model in hospitalized patients.
Comparison with similar research and explanations of findings
The transition from face-to-face care to a virtual care model is occurring, moving from being an elective component to becoming a fundamental part of healthcare delivery. Following the COVID-19 pandemic, the virtual care model has grown around the world in terms of the number of services provided, as well as in terms of indications in the different clinical specialties (36). This phenomenon has also been observed in Latin American countries, which has led physicians, patients, and regulatory bodies to support this transformation and merger with the current model. This model has also been recognized as a tool that improves the opportunities for care and combats health inequity, which is mainly attributed to the remoteness of the territories, the difficulty of mobilization, and the centralization of some medical specialties in cities with a high concentration of population (3,36). Additionally, it is worth mentioned that due to the epidemiological transition and the increase in life expectancy, virtual care will be considered a great alternative to strengthen the care of these elderly people and to reduce the burden attributed to the chronic diseases prevalent in this age group.
Virtual care is highly likely to be a cost-effective model for the treatment of a broad spectrum of pathologies (37,38). For example, the incorporation of telemedicine during screening for blinding eye diseases in rural and urban populations in China has allowed the timely identification of cases in early stages while reducing medical cost compared to traditional screening (incremental cost-effectiveness ratio of $2,567 vs. $7,251) (39). In cases with stroke in England, the use of telemedicine has optimized rapid access to acute care, with total healthcare cost savings of £482k and £471k with respect to traditional services (40). Similar results have been obtained with improved patient outcomes and lower medical costs in the management of rheumatoid arthritis (41), diabetes (42), musculoskeletal or dermatological conditions (43,44).
Although the COVID-19 pandemic allowed us to visualize the potential of this model of care, it was also an opportunity to identify those barriers or challenges that must be overcome to consolidate and allow its expansion. Similar to the results of other studies conducted in several countries (45,46), access and lack of knowledge about the use of electronic devices were the main barriers identified to accessing virtual care services. It is important to highlight that, in different clinical scenarios, including the management of oncology patients, it has been reported that around 90% of users are in favor and satisfied with the virtual care model (47). Health services in most Latin American countries are provided under a universal public insurance model in which the public and private sectors coexist to achieve universal health coverage (e.g., Argentina, Chile, Colombia, México), with equal access to drugs, surgical procedures, and medical and dental services (48). Health systems are financed by taxes and contributions from individuals according to their ability to pay (e.g., employed, or self-employed), so their sustainability depends on the balance between the percentage of subsidized and contributed population. The systems operate under a free/regulated competition market allowing public and private providers to compete on cost and quality, which leads to a decentralized nature in the provision of services to individuals because the same patient can be attended by several providers simultaneously in order to reduce costs. Although government regulations contain costs and set fair rates/prices, in the context of virtual care, the lack of suitable legislation has resulted in insignificant rates and reimbursement, which is an obstacle to its widespread use in the region. Furthermore, compared to developed countries, the lack of integration between virtual and face-to-face providers may end up increasing the decentralization of healthcare delivery.
The willingness of national governments to provide sufficient infrastructure throughout the territories is paramount to overcoming barriers related to access to the internet or electronic devices. For example, based on the World Bank report, the Latin American region has a gap in the connectivity percentage of its populations compared to the United States and Europe, with 76% coverage compared to 92% and 87%, respectively (49). Given that in rural or remote areas it is difficult to ensure that the entire population has the necessary technology to access virtual care, equipped government and/or private healthcare centers should be available to serve as intermediaries between the virtual programs of highly complex hospital institutions and patients. Beyond the technological aspects, national governments and Ministries of Health should also be concerned with developing and implementing standards to regulate the provision of virtual healthcare services, delimiting indications for use, operational aspects, costs, and the civil liability of institutions and medical personnel. In the region, Colombia, Panama, and Peru have been the countries with the greatest progress in the regulatory framework, including the degree of governance and protection of personal data in the context of virtual healthcare (50).
During the diagnostic process, a complete physical examination together with a detailed clinical history is the fundamental basis for the suspicion of any pathology, taking even more relevance in some specialties, such as neurology, orthopedics, rheumatology, or dermatology (51). Therefore, the impossibility of palpating the patient and not being able to perform certain signs or clinical tests during the medical consultation represents a weakness of the virtual care model, as evidenced in this study. To mitigate this barrier, it is necessary to implement clinical practice guidelines that combine mixed face-to-face and remote visits, in addition to an exhaustive dialogue with patients, so that the physician can extract the necessary information to rule out or suspect a particular diagnosis (52). In the particular case of neurology, the implementation of a sequential care model has been proposed, visualizing it as a tool during the clinical follow-up of patients already diagnosed for whom the physical examination is of minor relevance (34).
In addition, it has been shown that virtual physical assessments may achieve similar accuracy to face-to-face assessments if patients receive standardized, organized, and clear instructions and have the appropriate devices (53-55). Specific procedures should be developed for each clinical specialty or pathology to guide the questions and instructions given to patients to improve self-assessment. For example, Askanase et al. (56) developed a protocol for virtual physical examination in patients with systemic lupus erythematosus and are currently conducting a study to assess the degree of concordance with the face-to-face findings. However, this study is still in the recruitment phase.
Implications and actions needed
As with any transformation, socialization and education of all those involved in the virtual care model are essential for achieving acceptance of the model. This implies that each country and hospital center must identify the environmental factors that generate the greatest resistance to the expansion of the model to generate intervention strategies. Generally, these include strengthening training programs on the use of healthcare technologies, optimizing communication channels, and improving data management and cybersecurity. In addition, ensuring interoperability with the current system is another challenge to be overcome, especially in Latin American countries that have fragmented healthcare systems and limited interaction between the different stakeholders.
Conclusions
In conclusion, the virtual care model is a safe and cost-effective alternative for the delivery of health services, with multiple benefits for patients and their families. Therefore, virtual care offers a great alternative for strengthening healthcare systems, enabling a better performance in two indicators on which the health sector is working hard: timeliness of care and coverage. At the same time, this alternative encourages disease promotion and prevention activities. Likewise, the analysis of the main barriers and benefits is fundamental to consolidating this model of care and ensuring its expansion in the region. We hope this research shed new lights that encourage further research in this field.
Acknowledgments
The authors thank Clínica Imbanaco Grupo Quirón Salud for their support during this project.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the PRISMA reporting checklist. Available at https://mhealth.amegroups.com/article/view/10.21037/mhealth-23-47/rc
Peer Review File: Available at https://mhealth.amegroups.com/article/view/10.21037/mhealth-23-47/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://mhealth.amegroups.com/article/view/10.21037/mhealth-23-47/coif). P.D. is the COO of Vitae Health and R.P. is the CEO of Vitae Health. However, the company did not participate in the design or development of this research. The other author has no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- World Health Organization. Telemedicine: opportunities and developments in member states. Report on the second global survey on eHealth. World Health Organization; 2010.
- Doraiswamy S, Abraham A, Mamtani R, et al. Use of Telehealth During the COVID-19 Pandemic: Scoping Review. J Med Internet Res 2020;22:e24087. [Crossref] [PubMed]
- Omboni S, Padwal RS, Alessa T, et al. The worldwide impact of telemedicine during COVID-19: current evidence and recommendations for the future. Connect Health 2022;1:7-35. [Crossref] [PubMed]
- Alexander GC, Tajanlangit M, Heyward J, et al. Use and Content of Primary Care Office-Based vs Telemedicine Care Visits During the COVID-19 Pandemic in the US. JAMA Netw Open 2020;3:e2021476. [Crossref] [PubMed]
- Howard J, Kent T, Stuck AR, et al. Improved cost and utilization among Medicare beneficiaries dispositioned from the ED to receive home health care compared with inpatient hospitalization. The American Journal of Accountable Care 2019;7:10-6.
- Leong MQ, Lim CW, Lai YF. Comparison of Hospital-at-Home models: a systematic review of reviews. BMJ Open 2021;11:e043285. [Crossref] [PubMed]
- Roberts N, Carrigan A, Clay-Williams R, et al. Innovative models of healthcare delivery: an umbrella review of reviews. BMJ Open 2023;13:e066270. [Crossref] [PubMed]
- Lindgren L. Utilizing telehealth to enhance nursing care and reduce burnout. Nursing Made Incredibly Easy 2023;21:41-3. [Crossref]
- Bhaskar S, Bradley S, Chattu VKTelemedicine Across the Globe-Position Paper From the COVID-19 Pandemic Health System Resilience PROGRAM (REPROGRAM) International Consortium, et al. (Part 1). Front Public Health 2020;8:556720. [Crossref] [PubMed]
- LeRouge CM, Gupta M, Corpart G, et al. Health System Approaches Are Needed To Expand Telemedicine Use Across Nine Latin American Nations. Health Aff (Millwood) 2019;38:212-21. [Crossref] [PubMed]
- Consolidated telemedicine implementation guide. World Health Organization; 2022.
- Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Syst Rev 2021;10:89. [Crossref] [PubMed]
- Ouzzani M, Hammady H, Fedorowicz Z, et al. Rayyan-a web and mobile app for systematic reviews. Syst Rev 2016;5:210. [Crossref] [PubMed]
- Critical Appraisal Skills Programme. CASP Qualitative Studies Checklist [Internet]. 2022 [cited 2023 Apr 7]. Available online: https://casp-uk.net/casp-tools-checklists/
- Moskalewicz A, Oremus M. No clear choice between Newcastle-Ottawa Scale and Appraisal Tool for Cross-Sectional Studies to assess methodological quality in cross-sectional studies of health-related quality of life and breast cancer. J Clin Epidemiol 2020;120:94-103. [Crossref] [PubMed]
- Caetano R, Silva AB, Guedes ACCM, et al. Desafios e oportunidades para telessaúde em tempos da pandemia pela COVID-19: uma reflexão sobre os espaços e iniciativas no contexto brasileiro. Cad Saude Publica 2020;36:e00088920. [Crossref] [PubMed]
- Casilang CG, Stonbraker S, Japa I, et al. Perceptions and Attitudes Toward Mobile Health in Development of an Exclusive Breastfeeding Tool: Focus Group Study With Caregivers and Health Promoters in the Dominican Republic. JMIR Pediatr Parent 2020;3:e20312. [Crossref] [PubMed]
- Morais APP, Guimarães JMX, Alves LVC, et al. The production of care in psychosocial care services: home visits as an intervention technology to be used in the territory. Cien Saude Colet 2021;26:1163-72. [Crossref] [PubMed]
- Pedernera Bradichansky P, Selvatici L, Napoli S, et al. Teleconsultation during a pandemic. Experience of developmental pediatricians at Hospital de Pediatría "Prof. Dr. Juan P. Garrahan". Teleconsulta en épocas de pandemia. Experiencia de los pediatras del desarrollo del Hospital de Pediatría “Prof. Juan P. Garrahan”. Arch Argent Pediatr 2021;119:419-23. [PubMed]
- Escobar MF, Henao JF, Prieto D, et al. Teleconsultation for outpatient care of patients during the Covid-19 pandemic at a University Hospital in Colombia. Int J Med Inform 2021;155:104589. [Crossref] [PubMed]
- Böhm da Costa C, da Silva Peralta F, Aurelio Maeyama M, et al. Teledentistry System in Dental Health Public Services: A Mixed-Methods Intervention Study. Int J Med Inform 2021;153:104533. [Crossref] [PubMed]
- Loza CA, Baez G, Valverdi R, et al. Estudio cualitativo sobre los adultos mayores y la accesibilidad a los servicios de salud durante el confinamiento por COVID-19 en Buenos Aires, Argentina - parte 2. Medwave 2021;21:e8192. [PubMed]
- Palma A, Rojas V, Ihl F, et al. Implementation of a Palliative Hospital-Centered Spiritual and Psychological Telehealth System During COVID-19 Pandemic. J Pain Symptom Manage 2021;62:1015-9. [Crossref] [PubMed]
- Catapan SC, Willemann MCA, Calvo MCM. Estrutura e processo de trabalho para implantação da teleconsulta médica no Sistema Único de Saúde do Brasil, um estudo transversal com dados de 2017-2018. Epidemiologia e Serviços de Saúde. 2021;30:e2020305. [Crossref] [PubMed]
- Chávarri-Guerra Y, Ramos-López WA, Covarrubias-Gómez A, et al. Providing Supportive and Palliative Care Using Telemedicine for Patients with Advanced Cancer During the COVID-19 Pandemic in Mexico. Oncologist 2021;26:e512-5. [Crossref] [PubMed]
- Garcia-Huidobro D, Vergés A, Basualto P, et al. Mixed-Methods Evaluation of the Initial Implementation of Advanced Home Visits in Chile. Health Promot Pract 2022;23:493-503. [Crossref] [PubMed]
- Mayela RV, Yamil M, Amin CA, et al. Satisfaction With Telemedicine Consultation as Follow-Up Visit in Patients with Parkinsonism and Essential Tremor in during the Covid-19 Pandemic. Neurol India 2022;70:2003-8. [Crossref] [PubMed]
- Michell A, Besomi M, Seron P, et al. Implementation of physiotherapy telerehabilitation before and post Covid-19 outbreak: A comparative narrative between South American countries and Australia. Salud Publica Mex 2022;64:S31-9. [Crossref] [PubMed]
- Gutiérrez Rincón V, Bayon MC, Zambrano JJA, et al. Exploring the Configuration of Institutional Practices—A Case Study of Innovation Implementation in Healthcare. Sustainability 2022;14:3282. [Crossref]
- Piskorz D, Díaz-Barreiro LA, López Santi R, et al. Blood pressure telemonitoring and telemedicine for hypertension management-positions, expectations and feasibility of Latin-American practitioners. SURVEY carried out by several cardiology and hypertension societies of the Americas. Blood Press 2022;31:236-44. [Crossref] [PubMed]
- Sarti TD, Almeida APSC. Incorporação de telessaúde na atenção primária à saúde no Brasil e fatores associados. Cad Saúde Pública 2022;38:PT252221. [Crossref] [PubMed]
- Aliaga-Castillo V, Horment-Lara G, Contreras-Sepúlveda F, et al. Safety and effectiveness of telerehabilitation program in people with severe haemophilia in Chile. A qualitative study. Musculoskelet Sci Pract 2022;60:102565. [Crossref] [PubMed]
- García-Gutiérrez FM, Pino-Zavaleta F, Romero-Robles MA, et al. Self-reported perceptions and knowledge of telemedicine in medical students and professionals who enrolled in an online course in Peru. BMC Med Educ 2023;23:88. [Crossref] [PubMed]
- Alonso R, Eizaguirre MB, López P, et al. Argentinean consensus recommendations for the use of telemedicine in clinical practice in adult people with multiple sclerosis. Neurol Sci 2023;44:667-76. [Crossref] [PubMed]
- Bhatia RS, Chu C, Pang A, et al. Virtual care use before and during the COVID-19 pandemic: a repeated cross-sectional study. CMAJ Open 2021;9:E107-14. [Crossref] [PubMed]
- Mahmoud K, Jaramillo C, Barteit S. Telemedicine in Low- and Middle-Income Countries During the COVID-19 Pandemic: A Scoping Review. Front Public Health 2022;10:914423. [Crossref] [PubMed]
- Bell-Aldeghi R, Gibrat B, Rapp T, et al. Determinants of the Cost-Effectiveness of Telemedicine: Systematic Screening and Quantitative Analysis of the Literature. Telemed J E Health 2023;29:1078-87. [Crossref] [PubMed]
- Eze ND, Mateus C, Cravo Oliveira Hashiguchi T. Telemedicine in the OECD: An umbrella review of clinical and cost-effectiveness, patient experience and implementation. PLoS One 2020;15:e0237585. [Crossref] [PubMed]
- Liu H, Li R, Zhang Y, et al. Economic evaluation of combined population-based screening for multiple blindness-causing eye diseases in China: a cost-effectiveness analysis. Lancet Glob Health 2023;11:e456-65. [Crossref] [PubMed]
- Afolabi O, Parsekar K, Sibson L, et al. Cost effectiveness analysis of the East of England stroke telemedicine service. J Stroke Cerebrovasc Dis 2023;32:106939. [Crossref] [PubMed]
- Skovsgaard CV, Kruse M, Hjollund N, et al. Cost-effectiveness of a telehealth intervention in rheumatoid arthritis: economic evaluation of the Telehealth in RA (TeRA) randomized controlled trial. Scand J Rheumatol 2023;52:118-28. [Crossref] [PubMed]
- Lee JY, Lee SWH. Telemedicine Cost-Effectiveness for Diabetes Management: A Systematic Review. Diabetes Technol Ther 2018;20:492-500. [Crossref] [PubMed]
- Buvik A, Bergmo TS, Bugge E, et al. Cost-Effectiveness of Telemedicine in Remote Orthopedic Consultations: Randomized Controlled Trial. J Med Internet Res 2019;21:e11330. [Crossref] [PubMed]
- López-Liria R, Valverde-Martínez MÁ, López-Villegas A, et al. Teledermatology versus Face-to-Face Dermatology: An Analysis of Cost-Effectiveness from Eight Studies from Europe and the United States. Int J Environ Res Public Health 2022;19:2534. [Crossref] [PubMed]
- Ftouni R, AlJardali B, Hamdanieh M, et al. Challenges of Telemedicine during the COVID-19 pandemic: a systematic review. BMC Med Inform Decis Mak 2022;22:207. [Crossref] [PubMed]
- Khoshrounejad F, Hamednia M, Mehrjerd A, et al. Telehealth-Based Services During the COVID-19 Pandemic: A Systematic Review of Features and Challenges. Front Public Health 2021;9:711762. [Crossref] [PubMed]
- Pogorzelska K, Chlabicz S. Patient Satisfaction with Telemedicine during the COVID-19 Pandemic—A Systematic Review. Int J Environ Res Public Health 2022;19:6113. [Crossref] [PubMed]
- Gilardino RE, Valanzasca P, Rifkin SB. Has Latin America achieved universal health coverage yet? Lessons from four countries. Arch Public Health 2022;80:38. [Crossref] [PubMed]
- The World Bank. Individuals using the Internet (% of population) [Internet]. 2023 [cited 2023 May 24]. Available online: https://data.worldbank.org/indicator/IT.NET.USER.ZS
- Investment Banking Division. Regulatory Framework for Telemedicine: Current status and next steps [Internet]. 2022 [cited 2023 Oct 27]. Available online: https://publications.iadb.org/publications/english/viewer/Regulatory-Framework-for-Telemedicine-Current-status-and-Next-Steps.pdf
- Yao P, Adam M, Clark S, et al. A scoping review of the unassisted physical exam conducted over synchronous audio-video telemedicine. Syst Rev 2022;11:219. [Crossref] [PubMed]
- Laskowski ER, Johnson SE, Shelerud RA, et al. The Telemedicine Musculoskeletal Examination. Mayo Clin Proc 2020;95:1715-31. [Crossref] [PubMed]
- Lu AD, Veet CA, Aljundi O, et al. A Systematic Review of Physical Examination Components Adapted for Telemedicine. Telemed J E Health 2022;28:1764-85. [Crossref] [PubMed]
- Benziger CP, Huffman MD, Sweis RN, et al. The Telehealth Ten: A Guide for a Patient-Assisted Virtual Physical Examination. Am J Med 2021;134:48-51. [Crossref] [PubMed]
- Ogawa EF, Harris R, Dufour AB, et al. Reliability of Virtual Physical Performance Assessments in Veterans During the COVID-19 Pandemic. Arch Rehabil Res Clin Transl 2021;3:100146. [Crossref] [PubMed]
- Askanase AD, Aranow C, Kim MY, et al. Protocol for virtual physical examination in an observational, longitudinal study evaluating virtual outcome measures in SLE. Lupus Sci Med 2023;10:e000952. [Crossref] [PubMed]
Cite this article as: De La Torre A, Diaz P, Perdomo R. Analysis of the virtual healthcare model in Latin America: a systematic review of current challenges and barriers. mHealth 2024;10:20.