
Updated taxonomy of digital mental health interventions: a conceptual framework
Introduction
The role of digital mental health interventions (DMHIs) in the delivery of mental health prevention and treatment services has grown rapidly (1). DMHIs can transcend the limitations of space and time, as we will describe below. One of the efforts to organize DMHI offerings was provided by a think tank on “Digital CBT Technologies to Provide Care to Difficult-to-Reach and Underserved Populations” sponsored by the Association of Behavioral and Cognitive Therapies (ABCT). Their article describes “digital apothecaries”, that is, repositories of apps, websites, and other digital tools available to professionals and the public and four types of interventions (2). The current article updates the definitions of these four types and illustrates each as applied to prevention and treatment. These illustrations will focus primarily on studies that involve populations that have historically experienced health disparities to demonstrate that DMHIs can benefit these groups (3). We propose that the field use this taxonomy of DMHIs to mindfully develop interventions within each category and to use these categories to organize reviews of the literature.
The National Academies of Science, Engineering, and Medicine (4) has suggested that the mental health intervention spectrum consists of interventions that are focused on (I) promoting mental health, including healthy development of children and youth, (II) preventing mental disorders prior to the onset of clinical episodes, (III) treatment which occurs during the active phase of a clinical episode, and (IV) maintenance interventions designed to reduce relapse and recurrence of clinical episodes. The current article presents illustrations of preventive and treatment interventions for various mental health problems. The purpose of preventive interventions is to reduce incidence, that is, the number of new clinical episodes. Treatment interventions aim to reduce prevalence, that is, the number of persons experiencing current clinical episodes.
The taxonomy previously proposed (2) describes four types of digital interventions: Type 1 and Type 2 DMHIs are those offered within the context of a professional relationship, there is an identified provider and an identified patient or client. Type 1 DMHIs are traditional provider-client interventions that can be carried out remotely using electronic means such as teletherapy, phone call(s), or online conferencing. Type 2 are Type 1 (provider-client) interventions enhanced by digital adjuncts, such as email, text, chat, and other remote communication options, asynchronous data collection tools (e.g., smartphones, wearables, websites, or apps), or other digital tools intended to provide supplemental therapeutic experiences, such as virtual reality (VR) or augmented reality (AR).
Interventions such as teletherapy can transcend space, that is, the constraints that geographical distance places on our ability to serve all who need services. Interventions administered via telephone [e.g., Mohr et al. (5)] or video conferencing [e.g., Batastini et al. (6)] can be as effective as in-person services. Distance as an obstacle is particularly relevant in rural areas where patients need to travel large distances to reach clinics, and for patients who have severe debilitating health and mental health conditions that may prevent them from receiving care at an in-person clinic (e.g., severe social anxiety disorder/social phobia or physical limitations) (6). Even in urban areas, many patients often experience difficulties paying for transportation to clinics, arranging for time off from work, or caregiving obligations related to child or elder care for family members. For example, a recent patient perception study focused on telehealth trauma services for youth, found that telemental health can help address barriers to receiving treatment such as caregiver job schedules, distance to clinics, and lack of transportation (7). Furthermore, during the coronavirus disease (COVID) pandemic, when many providers began to offer telehealth services, many clinics found that the no-show rate decreased (8).
Type 3 and Type 4 DMHIs are digital self-help interventions. These are used similar to a self-help book and do not involve a formal relationship with a provider. The author of a self-help book does not undertake professional responsibility for the reader nor offers crisis intervention services, and neither does the provider of digital self-help tools. Type 3 DMHIs are guided self-help interventions; human support is offered only to increase adherence and effectiveness, and to reduce dropout. Reviews of digital interventions have identified two types of support: therapeutic and technical support (9). Therapeutic support involves providing information and explanations regarding how behavior change tools are intended to be used. Technical support is limited to helping users to navigate the digital tool. Type 4 DMHIs are fully automated self-help interventions and do not require human support. They include websites, apps, automated text messaging, or chatbots.
Muñoz et al. (2) in which this taxonomy was first suggested, defined Type 1 interventions as “traditional in-person clinical services that do not use digital interventions” (p. 3). The COVID-19 pandemic greatly changed the delivery of health care in March 2020. Most mental health providers began using video conferencing therapy sessions, thus embracing digital technology to provide live sessions. This is the reason we now include synchronous treatment and preventive interventions as part of Type 1 interventions provided via digital telehealth media. In-person interventions that do not involve digital elements will no longer be included in the definition of Type 1 digital interventions.
Consumable and non-consumable interventions
An important concept relevant to the four types of DHMIs is the difference between consumable and non-consumable interventions. Consumable interventions are used up after they are administered. For example, the nicotine patch is discarded at the end of the day, antidepressants are consumed as they are ingested, and psychotherapy sessions “use up” the therapist’s time as they are delivered—no other patient will benefit from that hour of the therapist’s time. Non-consumable interventions, on the other hand can be used again and again, without losing their therapeutic power. DHMIs, such as websites or apps, can thus benefit thousands of people at very low cost anytime and anywhere there is access to the Internet. For example, a website that costs $1 million to create and evaluate, costs $1,000 per person if 1,000 people use it, $10 if 100,000 people use it, and $1 if a million people use it. This could make it possible for non-consumable interventions to be provided to the public free of charge, especially if supported by public health systems, academic, or other non-profit institutions. For-profit institutions could offer non-consumable interventions (Type 4) at no charge to attract paying clients to their websites and as part of their corporate contribution to the public good. They could then obtain revenue by charging users for consumable services, modest fees for coaches supporting guided interventions (Type 3) and market rates for therapists (Type 1 and Type 2) for users who choose (and can afford) these professional care options.
Although consumable interventions are generally more effective and have lower dropout rates, the reach of non-consumable interventions can sometimes mean that more people can benefit from them (9,10). For example, if a consumable intervention serves 1,000 people in a month and is 50% therapeutically effective, it will benefit 500 people a month. If a non-consumable intervention serves 100,000 people in a month and is only 10% effective, it still can benefit 10,000 people that month. This is 20 times more than the consumable intervention.
How the proposed taxonomy fits within the World Health Organization (WHO) taxonomy
The WHO (11) developed a taxonomy to classify digital health interventions (DHIs) that is called “Classification of Digital Health Interventions v1.0”. This classification focuses on public health and was created to provide “standardized vocabulary” to the communities working with digital health. The WHO organized DHIs in four categories: interventions for clients, interventions for healthcare providers, interventions for health care system or resource managers, and interventions for data services. These classifications and categories are intended for general health care. Our updated taxonomy is specific to DMHIs for clients (Type 1 and Type 2) within a healthcare system, self-help users with human support (Type 3) outside a healthcare system, and fully automated (no human support) self-help (Type 4) similar to self-help books.
For each of the four types (Figure 1, Table 1) we will provide illustrations and we will also specify whether the interventions are intended to produce treatment or prevention effects. We will refer to review articles for most categories and provide descriptions of illustrative studies involving underserved populations for each category whenever possible. It is important to emphasize the need to conduct more research with these populations [e.g., Classen et al. (12)]. For example, 37.6% of White adults with diagnosis-based need for mental health or substance abuse care receive treatment, compared to 22.4% of Latinos and 25.0% of African American (13). Furthermore, minority adolescents are predicted to be at greater risk of mental disorders than their White counterparts, and yet are less likely to use mental health services (14).
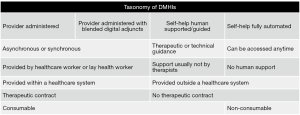
Table 1
| Type | Description | Therapeutic contract | Consumable | Example |
|---|---|---|---|---|
| Type 1: provider administered DMHIs | These are asynchronous or synchronous digital interventions by independent practitioners or lay health workers who are providing treatment or prevention services in their role as health care providers via telehealth media | Yes | Yes | Since the COVID-19 pandemic began, many if not most of these interventions include “teletherapy”, in which the provider administers an intervention using digital tools such as the telephone or online video conferencing |
| Type 2: provider administered DMHIs with blended digital adjuncts | These are asynchronous or synchronous digital interventions by independent practitioners or lay health workers who are providing treatment or prevention services in their role as health care providers and are using digital adjuncts | Yes | Yes | The addition of email, text messaging, apps or websites as adjuncts to treatment, or other digital tools such as VR, AR, or other forms of adjuncts beyond live interactions |
| Type 3: self-help human supported/guided DMHIs with therapeutic or technical guidance | These interventions offer human support for the user of self-help digital tools to reduce the large proportion of dropouts from most digital self-help interventions. The support is not generally provided by licensed therapists | No | Yes | Support can be provided by students or other lay individuals trained to encourage users to adhere to the self-help digital tools or to help them navigate these tools |
| Type 4: self-help fully automated DMHIs | These interventions are fully automated self-help interventions. They do not require human time when administered | No | No | These interventions, such as websites and apps, can be used by anyone, anywhere, ideally at no charge to the user. Thus, they transcend the limitations of both space and time; users anywhere in the world can access them, without having to arrange for an appointment time with a provider or a guide |
DMHIs, digital mental health interventions; COVID-19, coronavirus disease 2019; VR, virtual reality; AR, augmented reality.
Type 1: provider administered DMHIs
Type 1 interventions are asynchronous or synchronous DMHIs by licensed practitioners or lay health workers who provide live treatment or prevention services in their role as health care providers. These interventions include “teletherapy”, in which the provider administers an intervention using tools such as the telephone or online video conferencing. Regarding treatment, there is a therapeutic contract with the client or patient and the therapist assumes legal and/or professional responsibility for the case. With preventive interventions, there is an implied professional relationship because the provider is offering official health services. This type of DMHI is offered within a healthcare system. Because Type 1 interventions involve provider time, they are consumable and are limited to how many people the provider can serve.
Illustrations of Type 1 DMHIs
As Type 1 DMHIs became popular because of their convenience and extended outreach capacity to different populations and geographic regions, many systematic and general reviews and individual studies have been conducted. Following are systematic reviews and individual studies of treatment and preventive interventions to illustrate the effectiveness of Type 1 DMHIs.
Reviews of Type 1 DMHIs
Lawes-Wickwar et al. (1) conducted a systematic review of 29 randomized controlled trials (RCTs) about the application and effectiveness of telehealth and other therapy technologies for individuals with severe mental illness (SMI). Results indicated that technological tools have different outcomes depending on the disorder and reported symptoms. For example, the authors reported that telephone support effectively improved medication adherence, reduced manic symptoms, and reduced days at an inpatient facility. Another review by Zhao et al. (15) about the effectiveness of telehealth interventions for women with postpartum depression (PPD), found that “telehealth interventions could effectively reduce symptoms of depression and anxiety in women with PPD” (p. 1). These reviews present evidence that Type 1 interventions can be effective in reducing severity of mental health symptoms.
Illustrative treatment studies
See Table 2 for individual study details. A recent pilot RCT by Spruill et al. (16) evaluated the feasibility, acceptability, and effectiveness of a culturally adapted depression self-management program [project UPLIFT (Using Practice and Learning to Increase Favorable Thoughts)] delivered via telephone to Hispanic adults with epilepsy. Intention-to-treat analyses showed that participants in the UPLIFT program (n=36) had significantly lower rates of depressive symptoms in comparison to the usual care group (n=36) at 8-week follow-up (63% vs. 72%), 6-month follow-up (40% vs. 70%), and 12-month follow-up (47% vs. 70%). Stewart et al. (17) evaluated the effectiveness of a pilot trauma-focused cognitive-behavioral therapy (TF-CBT) treatment delivered via one-to-one videoconferencing for racial and ethnic minority children and adolescents from economically disadvantaged backgrounds or living in rural areas. Post-traumatic stress disorder (PTSD), depression, and anxiety symptoms significantly decreased in participating children and adolescents from pretreatment to post-treatment. Caretakers participating in the study also reported seeing a reduction in PTSD, depression, anxiety, and emotional/behavioral problems. Pilot studies such as these exemplify how Type 1 interventions such as teletherapy and telephone interventions can be effective in treating the mental health needs of underserved populations. Full scale DMHIs studies with these populations are much needed.
Table 2
| Treatment or prevention | Example | Disorder(s) | Intervention(s) | Sample | ||||
|---|---|---|---|---|---|---|---|---|
| Population(s) | Sample size | Gender; race/ethnicity | Country | Language | ||||
| Treatment | Spruill et al. (16) | Depression | Telephone-based self-management training called “Project UPLIFT” vs. usual care | Adults with epilepsy; age: M =42.8 years | N=72 (UPLIFT: n=36; usual care: n=36) | 70.8 % female; 100% Hispanic | USA | English Spanish |
| Treatment | Stewart et al. (17) | PTSD | TF-CBT via videoconferencing | Youths who had trauma exposure; age: M =10.8 years | N=15 | 93.3% female; 46.7% Hispanic, 40% African American, 13.3% Caucasian | USA | English Spanish |
| Prevention | Lopez et al. (18) | Depression | CBCC vs. BACC vs. usual care | Adult caregivers with elevated depressive symptoms; age: M =54 years | N=219 (CBCC: n=69; BACC: n=70; usual care: n=80) | 90.9% female; no race/ethnicity provided | Spain | Spanish |
If gender/ethnicity information is only available by group, then total percentage = aggregate sample from each group/total sample. DMHIs, digital mental health interventions; CBCC, cognitive-behavioral conference call; UPLIFT, Using Practice and Learning to Increase Favorable Thoughts; M, mean; PTSD, post-traumatic stress disorder; TF-CBT, trauma-focused cognitive-behavioral therapy; BACC, behavioral-activation conference call.
Illustrative prevention studies
Many Type 1 interventions have shown to be effective as a prevention tool for various mental health disorders. Lopez et al. (18) conducted an RCT to evaluate the long-term efficacy of a cognitive-behavioral conference call (CBCC) intervention (n=69) in comparison to a behavioral-activation conference call (BACC) intervention (n=70) and a usual care control group (UCCG, n=80) to prevent depressive symptoms in informal caregivers showing elevated but subclinical depressive symptoms. At the 36-month follow-up, the incidence of depression was lower for CBCC [8.7%, relative risk (RR) =0.26] and BACC (8.6%, RR =0.25) in comparison to the UCCG (33.7%). “For both interventions, it was found that approximately one new case of depression would be prevented for every four caregivers treated” (p. 17), compared to the UCCG.
Type 2: provider administered DMHIs with blended digital adjuncts
Type 2 are asynchronous and synchronous DMHIs by independent practitioners or lay health workers providing treatment or prevention services using digital adjuncts to enhance their interventions. These include email, text messaging, apps or websites, VR, AR or other forms of adjuncts beyond synchronous online interactions.
With Type 2 treatment, there is still a therapeutic contract with the client or patient, and the therapist is legally and professionally responsible for the case. Type 2 DMHIs are offered within a healthcare system and are consumable, that is, limited in terms of how many people they can serve by provider availability. However, it is possible that the addition of digital adjuncts could reduce the time a provider needs to spend on each patient, and thus the cost involved. For example, Lock et al. (19) conducted a feasibility study of an RCT comparing the efficacy of a family-based treatment through videoconference (FBT-V) and an online guided self-help version of the program (GSH-FBT) to treat anorexia nervosa in adolescents. Participants in this study had to be under the care of a physician to monitor their safety throughout the treatment. One of the findings was that there was a reduction in time spent by therapists favoring the GSH-FTB group, “depending on the outcome, this efficiency if confirmed in an adequately powered study could lead to cost differences related to therapist time being approximately 1.9–3.4 times less costly in GSH-FBT than FBT-V” (p. 2006).
Review of Type 2 DMHIs
Berrouiguet et al. (20) conducted a systematic review of studies using mobile phone text messaging as an adjunct to mental health care services. Within the studies analyzed, text messaging was used to send reminders, information/education, supportive messages, or for self-monitoring. The authors conclude that a large overarching benefit of text messaging was its use for self-assessment and ecological momentary assessment (EMA) via real-time data capture. In addition, text-messaging contributed to continuity of care, was often used to extend care after discharge, or for delivery of preventive messages to at-risk populations. The authors point out that text-messaging can be readily accepted by populations who often refuse treatment, such as patients suffering from eating disorders (EDs) or suicide attempters who initially refused hospitalization. And text-messaging can also reduce feelings of isolation in patients suffering from mental illnesses.
Illustrative treatment studies
See Table 3 for individual study details. Mantani et al. (21) conducted a parallel-group RCT to evaluate the effectiveness of a smartphone app (Kokoro-app) as an adjunct to treatment. The Kokoro-app is a CBT-based self-help smartphone app to treat depression in patients with major depression and antidepressant resistance. Patients were randomized to a medication change + Kokoro-app CBT (n=81) group or medication change only (n=83) group. Medication change meant that at the beginning of the study (week 0), participants began changing their antidepressant to a new one, with “the previous antidepressant tapered off by week 5” (p. 3). With intention-to-treat analysis, results showed that participants in the app group had significantly lower depression symptoms (primary outcome, P<0.001) than the control group at post intervention (week 9). Aguilera et al. (22) evaluated text messaging as an adjunct to CBT group therapy sessions (total of 16 weeks) for depression to increase engagement and improve outcomes. With intention-to-treat analysis, results showed that attendance in the CBT program significantly improved for text messaging participants (median of 13.50 weeks) compared to the control group (median of 3 weeks) before dropping out. Mantani et al. (21) and Aguilera et al. (22) show that using a digital tool as an adjunct to treatment, that is, a Type 2 intervention, can be beneficial in reducing depressive symptoms and increasing participant engagement.
Table 3
| Treatment or prevention | Example | Disorder(s) | Intervention(s) | Sample | ||||
|---|---|---|---|---|---|---|---|---|
| Population(s) | Sample size | Gender; race/ethnicity | Country | Language | ||||
| Treatment | Mantani et al. (21) | Depression | Cognitive behavioral therapy app Kokoro + antidepressant switch vs. antidepressant switch only | Adult patients with primary diagnosis of major depression; age: M =40.2 years | N=164 (app: n=81; medication: n=83) | 53% female; no race/ethnicity provided | Japan | Japanese |
| Treatment | Aguilera et al. (22) | Depression | CBT group therapy + text messaging vs. CBT group therapy only | Adult patients at an urban public hospital referred to a behavioral health clinic; age texting: M =51.71 years, age group therapy only: M =51.83 years | N=85 (CBT + text: n=45; CBT only: n=40) | 78.8% female; 100% Hispanic | USA | Spanish |
| Prevention | Barrera et al. (23) | Postpartum depression | The MB course + SMS text messages | Pregnant women (17 to 31 years); age: M =23.7 years | N=28 | 100% female; 43% Black or African American, 36% Hispanic or Latinx, 14% White, 4% Biracial, 4% prefer to not specify | USA | English |
If gender/ethnicity information is only available by group, then total percentage = aggregate sample from each group/total sample. DMHIs, digital mental health interventions; M, mean; CBT, cognitive-behavioral therapy; MB, mothers and babies; SMS, short messaging service.
Illustrative prevention study
Barrera et al. (23) assessed the feasibility and acceptability of an intervention course called the mothers and babies (MB) course, intended to prevent PPD that integrated text messages as part of the intervention. The MB was delivered in-person over 12 sessions in a period of 9 weeks as part of a home visiting program. The text messages were sent in English or Spanish using a web-based platform called HealthySMS. After each session, “home visitors were instructed to log-in to the HealthySMS platform to enter session data and trigger session-specific SMS text messages” (p. 6). Thirty-six text messages were integrated focusing on skill reinforcement, homework reminders, and self-monitoring. Overall, 68% of participants received the full set of text messages and completed the whole intervention. Participants found the text messages acceptable, rating the text messages as useful to very useful (64% to 86.3%) and understandable to very understandable (80% to 100%).
Type 3: self-help human supported/guided DMHIs
Type 3 DMHIs interventions offer human support for the use of self-help digital tools to reduce the substantial proportion of dropouts from most digital self-help interventions (24). Type 3 support can be provided by students or other lay helpers, or even health care providers trained to encourage users to adhere to the digital self-help tools or to help them navigate these tools. Because they involve human time, Type 3 self-help human supported/guided DMHIs are consumable and are limited in the number of users they can serve and by the number of hours that support staff have allotted.
- Type 3A: self-help human supported/guided DMHIs with therapeutic guidance. These offer what has been termed “Therapeutic guidance”, that is, “technology-mediated human support” with a focus on “content and processes related to the treatment and … of a genuine therapeutic nature” [(9), p. 11-12].
- Type 3B: self-help human supported/guided DMHIs with technical guidance. These offer only technical guidance, that is, “technical and compliance facilitating support” with the goal of solving “technical problems and facilitate the motivation and compliance of patients to the intervention” [(9), p. 11].
- Type 3A and 3B DMHIs are sometimes referred to as “guided” or “supported” interventions and are offered outside a healthcare system.
Reviews of Type 3 treatment DMHIs
In a recent meta-analysis, Moshe et al. (9) explored the efficacy of digital interventions for the treatment of depression. Remote interventions have gained traction since the onset of the COVID-19 pandemic, which has increased depression and reliance on technology-delivered treatment (6,25). Eighty-three RCTs were reviewed. Interventions with human technical guidance had an average effect size of g=0.46 (P<0.001) and interventions with human therapeutic guidance resulted in an average effect size of g=0.63 (P<0.001). Furthermore, there was no significant difference between guided digital interventions and face-to-face psychotherapy, suggesting that Type 3 interventions can be as effective as Type 1 and Type 2 interventions to treat depression.
Karyotaki et al. (26) explored if guided Internet-based interventions reduced depressive symptoms among adults. Twenty-four RCTs with 4,889 participants were analyzed. Results showed that guided internet interventions effectively reduced depressive symptoms and yielded higher response and remission rates than fully automated interventions. One important point to make is that in this review, ethnic minorities had lower response and remission rates.
Illustrative treatment studies
See Table 4 for study details and additional examples (27,28). To reduce mental health disparities among refugee immigrant populations in Sweden, Lindegaard et al. (29,30) conducted RCTs to investigate the effectiveness of culturally adapted Internet-Based Cognitive Behavior Therapy (iCBT) with weekly therapeutic guidance to treat depressive symptoms. In Lindegaard et al. (29), the iCBT was culturally adapted for a Kurdish population (n=50). In Lindegaard et al. (30), the iCBT was culturally adapted for an Arabic-speaking population (n=59). With intention-to-treat analysis, results showed that the treatment groups in both studies had a reduction in depressive symptoms in comparison to the wait-list control posttreatment [d=1.27, Lindegaard et al. (29); d=0.85, Lindegaard et al. (30)]. Both studies showed that guided self-help Internet interventions with therapeutic guidance can be effective in treating mental health symptoms in immigrant and refugee populations when the treatment is culturally adapted.
Table 4
| Treatment or prevention | Example | Disorder(s) | Intervention(s) | Sample | ||||
|---|---|---|---|---|---|---|---|---|
| Population(s) | Sample size | Gender; race/ethnicity | Country | Language | ||||
| Treatment | Harper Shehadeh et al. (27)* | Depression | WHO-guided step-by-step e-mental health intervention | Adults not at risk of suicide; age: M =27.7 years | N=129 | 78% female; 88% Lebanese, 6% Palestinian, 4% Syrian | Lebanon | Arabic |
| Prevention | Otero et al. (28)* | Depression | Happy app + telephone support through a conference call system | Adult non-professional caregivers; age: M =54 years | N=31 | 93.5% female; no race/ethnicity provided | Spain | Spanish |
| Treatment | Lindegaard et al. (29) | Depression | Culturally adapted iCBT vs. wait-list | Adult Kurdish immigrants; age: M =33.86 years | N=50 (iCBT: n=25; wait-list: n=25) | 46% female; no race/ethnicity provided | Sweden | Kurdish (Sorani) |
| Treatment | Lindegaard et al. (30) | Depression, anxiety, insomnia | Culturally adapted Individually tailored iCBT vs. wait-list | Adult Arabic immigrants; age: M =37.5 years | N=59 (iCBT: n=30; wait-list: n=29) | 42% female; no race/ethnicity provided | Sweden | Arabic |
| Treatment | Fitzimmons-Craft et al. (31) | Eating, disorders | SB-ED digital CBT-guided self-help program vs. usual care | Adult female college students; age: M =22.12 years | N=690 (SB-ED: n=385; usual care: n=305) | 100% female; 60% White, 17.1% Asian or South Asian, 5.4% Black or African American, 0.1% Native Hawaiian or Pacific Islander, 0.4% American Indian or Alaskan Native, 7.7% Multiracial, 6.7% Other | USA | English |
| Prevention | Buntrock et al. (32) | Depression | Psychoeducation, behavior therapy, and problem-solving therapy web-based multimedia intervention supported by an online trainer vs. enhanced usual care | Adults with subthreshold depression; age: M =45.04 years | N=406 (intervention: n=202; usual care: n=204) | 73.9% female; 83.5% White, 0.2% Black, 0.2% Hispanic, 16% not reported | Germany | German |
If gender/ethnicity information is only available by group, then total percentage = aggregate sample from each group/total sample. *, additional examples not described in the text. DMHIs, digital mental health interventions; WHO, World Health Organization; M, mean; iCBT, internet-based cognitive behavior therapy; SB-ED, student bodies-eating disorders.
In a cluster RCT, Fitzimmons-Craft et al. (31) investigated the effectiveness of an online guided self-help CBT intervention to improve outcomes of college women with EDs in 27 US universities. The intervention called student bodies-eating disorders (SB-ED) was part of an online Healthy Body Image program. Participants had access to this program for eight months and were assigned a coach. Coaches were doctoral students, social work master’s students, study staff, or postdoctoral fellows who received training in cognitive behavioral approaches for EDs, motivational interviewing, technical skills, and effective digital coaching. Therefore, this would be a Type 3A DMHI, providing therapeutic guidance. There were 1- and 2-year follow-ups. Follow-ups were combined for analysis. Participants were assigned to the SB-ED intervention group (n=385) or a referral to the usual care control group (n=305). With intent-to-treat analysis, results showed that participants in the intervention group had a significant reduction in ED psychopathology post intervention (d=−0.40, P<0.001) and follow-up (d=−0.35, P<0.001). There was also a significant reduction in depression for the intervention group at post intervention (d=−0.22, P=0.01) and follow-up (d=−0.21, P=0.001).
Review of Type 3 prevention DMHIs
Martínez et al. (33) conducted a systematic review to evaluate the effectiveness of Internet interventions for the prevention and treatment of depression focusing on populations from developing countries. Five feasibility studies and one protocol with the number of participants ranging from 23 to 17,318 per study were reviewed. Most studies focused on depression prevention (n=5) and came from Latin American countries (n=4). Results showed that Internet interventions for depression prevention with low levels of human support are useful and acceptable to users.
Illustrative prevention studies
Buntrock et al. (32) investigated the effect of a guided self-help depression prevention Internet intervention in adults with subthreshold depression in Germany. At 1-year follow-up, 47% of the control group developed a major depressive episode, compared to 27% in the intervention group. This study shows the potential of Type 3 interventions to serve as effective treatment and preventive measures for various mental and health disorders such as depression [e.g., Lindegaard et al. (29,30); Moshe et al. (9)]. These interventions have shown to be effective for various populations facing challenges seeking therapeutic services because of the lack of available services, stigma, time constraints, financial implications, and other barriers (9,33).
Type 4: self-help fully automated DMHIs
Type 4 are fully automated self-help DMHIs. They do not require human time when administered, thus they are not consumable. Type 4 interventions, such as websites, apps, chatbots, and text-messaging interventions can be used by anyone, anywhere, ideally at no charge to the user. Thus, they transcend the limitations of both space and time. Users anywhere in the world with an internet connection and a mobile device can access them without having to arrange for an appointment time with a provider. Type 4 interventions also address the limitations of cost because human time is not an issue. As more people use them, the marginal cost (the cost of providing an intervention to one additional person) eventually approaches, though it never reaches, zero. Type 4 DMHIs are offered outside a healthcare system. Users complete the intervention on their own with no human support and do not receive human supported feedback.
Review of Type 4 treatment DMHIs
Karyotaki et al. (34) systematically analyzed the effectiveness of self-guided iCBT in treating adults with depression. Self-guided iCBT was significantly more effective than control groups in treating depressive symptom severity and inducing a positive treatment response. The studies evaluated were conducted in six countries including Australia, Germany, Spain, Switzerland, the Netherlands, and the United Kingdom.
Illustrative treatment studies
See Table 5 for study details and additional examples (25,35-38). Muñoz and colleagues conducted a series of smoking cessation studies that provide evidence about the potential for the global outreach of fully automated digital interventions and the advantage of non-consumable interventions in terms of cost. Their first study (39) was an RCT with 1,000 randomized participants from 68 countries. Their second RCT (40) had 16,430 randomized participants from 165 countries. The website then morphed into a participant preference trial (3,10) with 15,170 participants from 168 countries. Across the three studies, 48,274 provided consent, and 32,600 provided sufficient pre-assessment data to be part of the studies. This level of global reach would be difficult to match with consumable interventions. Moreover, the cost of helping approximately 20% of participants quit smoking was significantly lower compared with the estimated cost of nicotine patches or smoking cessation groups.
Table 5
| Treatment or prevention | Example | Disorder(s) | Intervention(s) | Sample | ||||
|---|---|---|---|---|---|---|---|---|
| Population(s) | Sample size | Gender; race/ethnicity | Country | Language | ||||
| Treatment | Muñoz et al. (3) | Smoking/tobacco use | San Francisco Stop Smoking Site | Adults worldwide | Total visitors: n=164,182; consented: n=8,981; completed baseline: n=7,407 | 43.6% female; 73.5% Hispanic/Latino, 58.2% European, 10.8% Asian, 1.3% African, 0.5% Indigenous, 17.6 Other/Multiethnic, 11.3% Mestizo | 168 different countries and territories | English, Spanish |
| Treatment | Muñoz et al. (10) | Smoking/tobacco use | San Francisco Stop Smoking Site | Adults worldwide | Total visitors: n=94,158; consented: n=9,173; completed baseline: n=7,763 | 45% female (n=7,724); 75.5% Hispanic/Latino (n=7,692), race (n=7,504) (62.8% European, 7.3% Asian, 0.7% African, 0.3% Indigenous, 18.2% other/multiethnic, 10.6% Mestizo) | 152 different countries and territories | English, Spanish |
| Treatment | Aguilera et al. (25)* | Depression, anxiety | StayWell text-messaging | Adults with a mobile phone; age: M =33.3 years | N=303 | 76% female; 47.9% White or Caucasian, 20.5% Latino(a) or Hispanic, 13.2% Asian or Pacific Islander, 11.5% Multiethnic, 6.6% Black or African American, 0.3% unknown | USA | English, Spanish |
| Treatment | Schure et al. (35)* | Depression | iCBT online intervention thrive vs. wait-list with mental health information | Adults from a rural community in Montana with mild-to-severe depression; age: M =42.9 years | N=343 (iCBT: n=181; wait-list: n=162) | 85% female; 93% Caucasian | USA | English |
| Treatment | Andrade et al. (36)* | Alcohol consumption/use | Web-based intervention Beberemos (drink less) | Adult low-risk users; age: M =40 years | Total accessed site: n=32,401; registered: n=3,339; completed assessment n=929 | 46.4% female; no race/ethnicity provided | Brazil | English, Portuguese |
| Harmful/hazardous users; age: M =38 years | ||||||||
| Suggestive of dependance users; age: M =40 years | ||||||||
| Prevention | Barrera et al. (37)* | Postpartum depression | Mothers and babies online course (Curso Mamás y Bebés) vs. information only | Adult pregnant women; age: M =30.19 years | N=111 (course: n=57; info only: n=54) | 100% female; 71.3% Latino/Hispanic, 53.2% Caucasian/European, 31.8% Mestizo | 23 countries worldwide | English, Spanish |
| Prevention | Lara et al. (38)* | Depression | Web-based (HDep) for depression in Spanish (ADep = Ayuda para Depresión) based on CBT | Adults; age: M = NA | Total accessed site: n=28,078; qualified as users: n=17,318 | 84.4% female | Mexico | Spanish |
| Treatment | Muñoz et al. (39) | Smoking/tobacco use | San Francisco Stop Smoking Site | Adults worldwide | Total visitors: n=6,000; consented: n=1,417; randomized: n=1,000 (stop smoking guide alone: n=247; stop smoking guide + educational messages: n=251; stop smoking guide + educational messages + mood management course: n=251; stop smoking guide + educational messages + mood management + virtual group: n=251) | 45% female (n=1,000); 52.9% (n=975) Hispanic/Latino, race (n=992) (70% European; 8.3% Asian; 1.4% African; 0.3% Indigenous; 3% Multiethnic; 6.2% other; 10.8% Mestizo) | 68 different countries and territories | English, Spanish |
| Treatment | Leykin et al. (40) | Smoking/tobacco use | San Francisco Stop Smoking Site | Adults worldwide | Screened for eligibility: n=78,623; consented: n=28,703; randomized: n=16,430 (stop smoking guide alone: n=4,118; stop smoking guide + educational messages: n=4,097; stop smoking guide + educational messages + mood management course: n=4,110; stop smoking guide + educational messages + mood management + virtual group: n=4,105) | 47.2% female (n=16,349); 68.7% White (n=16,306) | 165 different countries and territories | English, Spanish |
| Prevention | Ebert et al. (41) | Stress management | Stress management mobile intervention iSMI GET.ON Stress vs. wait-list | Adults in the working population; age: M =41.76 years | N=396 (iSMI GET.ON: n=198; wait-list: n=198) | 76.3% female; 80.6% white, 2.3% Asian, 0.5% Hispanic, 16.7% prefer not to say | Germany | German |
If gender/ethnicity information is only available by group, then total percentage = aggregate sample from each group/total sample. *, additional examples not described in the text. DMHIs, digital mental health interventions; M, mean; iCBT, internet-based cognitive behavior therapy; NA, not available; iSMI, internet-based mobile-supported stress management intervention.
Review of Type 4 prevention DMHIs
Sander et al. (42) systematically reviewed 17 articles on Internet-based interventions that aimed to prevent mental disorders. The Internet-based intervention platforms evaluated the prevention of EDs, depression, anxiety, PTSD, generalized-anxiety disorder, or a combination of these disorders in a wide array of adult populations, including cancer patients, and university students. Internet interventions were effective in preventing EDs, depression, and anxiety. “Evidence was found for effectiveness of interventions for EDs, depression, and anxiety. Internet-based interventions can be considered effective in reduction of subthreshold symptomatology and may also be suitable for preventing the onset of mental disorders over the long term” (p. 15).
Illustrative prevention studies
Ebert et al. (41) conducted an RCT to investigate the effectiveness of a self-guided Internet-based mobile stress management universal prevention intervention in Germany. The 7-session plus one booster session of the intervention program called GET.ON, was delivered over seven weeks. There was no human support. Participants could choose to receive automated text messages. “Text messages focused on ultra-brief exercises to be carried out in daily life routine, aiming to facilitate transfer from training into real life” (p. 4). Participants were assigned to an intervention group (GET.ON Stress, n=198) or a wait-list control (n=198). The primary outcome was perceived levels of stress. With intention-to-treat analysis, results showed that the intervention group had lower perceived stress levels posttreatment (d=0.71) and at 6-month follow-up (d=0.61) compared to the wait-list-control.
Discussion
There are currently many DMHIs that are often grouped together indiscriminately. We believe that it is important to categorize DMHIs in a coherent manner because, as we have shown above, there are differences in effectiveness, dropout rates, and ability to reach large numbers of people depending on the type of DMHI being administered. This article presents an updated taxonomy of DMHIs to encourage the field in purposefully developing and evaluating interventions that clearly fit into one of four categories (Table 1). Types 1 and Types 2 refer to DMHIs specifically provided by a health professional or lay health worker within a healthcare system. Type 3 DMHIs refer to self-help interventions that require therapeutic or technical human support, given to all interested users outside a healthcare system. Type 4 DMHI’s refer to fully automated interventions similar to self-help books that do not involve human support. In addition, our conceptual framework notes the significant difference between consumable and non-consumable interventions regarding cost and the ability to reach large numbers of individuals. We also highlight the difference between preventive and treatment interventions. Preventive interventions are intended to forestall the onset of mental, emotional, or behavioral disorders. Treatment interventions are intended to help individuals who already meet criteria for a diagnosable condition. We hope that future studies and reviews of the efficacy and effectiveness of DMHIs will use this taxonomy to allow readers to compare results appropriately. Using the proposed taxonomy, we suggest that investigators specify (I) the type of DMHI being administered, (II) if it is consumable or non-consumable, and (III) if it is a preventive or treatment intervention study.
Specifying if the DMHIs are consumable or non-consumable will clarify whether the interventions require human time to administer or if they can be fully automated so that they can be accessed from anywhere at any time. Reporting whether the DMHI is intended to prevent or treat a mental health condition will be useful to systematically categorize the growing body of research on the use of digital technology for mental health treatment and prevention. More prevention DMHIs are needed to reach as many people possible and help prevent mental health conditions such as depression (43,44). This will allow us to serve more adequately those who develop serious mental health issues and decrease the burden that many mental health professionals are facing in the aftermath of the COVID-19 pandemic (45).
We believe each of the four categories are important and have unique advantages. We summarize each in turn below.
Type 1 DMHIs are closest to traditional therapy because the provider and the client or patient are engaged in a professional relationship. Telehealth interventions reduce the need for the client or patient to travel to the provider’s office. This can benefit patients who cannot afford transportation costs, are very distant from providers, have physical problems that require accommodations, or are afraid of being seen entering a mental health facility.
Type 2 DMHIs add the use of digital adjuncts to traditional sessions with the provider, which can contribute information that the provider can use to track progress, provide additional sources of support for the client or patient, and help the patient to adhere to treatment elements by monitoring mood, activity levels, and other daily behaviors that can enhance treatment outcomes. In addition, some studies have shown that digital adjuncts can reduce the number of hours that providers need to yield good outcomes [e.g., Lock et al. (19)].
Type 3 DMHIs have demonstrated reductions in dropout rates and increases in efficacy compared to unguided self-help interventions (9). Human support increases adherence, helps users surmount potential obstacles to using the interventions, and thereby add to the likelihood that the interventions will be effective.
Type 4 DMHIs are easily accessible for individuals with access to digital devices and the Internet. By being fully automated, they can be used at any time at the user’s convenience, and from anywhere in the world. Type 4 DMHIs are the only type that is non-consumable and therefore the least costly. Although they generally have higher dropout rates, and less efficacy than interventions with human support, the total number of people reached is potentially greater (9,10).
However, DMHIs could have potentially harmful effects due to unintended consequences. For example, because they are available only to those with access to digital devices and the Internet, they could widen health disparities. Allowing wealthier and more educated populations that tend to have greater access these resources to benefit from preventive and treatment interventions unavailable to others. Methods to make these tools available to those who do not own digital devices need to be developed, such as having community health workers equipped with digital devices visit communities without Internet access and share digital interventions with them. As is the case with traditional interventions, DMHIs will not be effective for everyone. It is important for more studies to include usually underrepresented members of our communities, to identify those groups for which more culturally appropriate interventions need to be developed, as well as those groups who respond as well to specific interventions as did the participants in the original clinical trials. Finally, the issue of cost must be addressed. Although there are examples of DMHIs that have been made available at no charge to anyone in the world (39,46), many DMHIs maintain a paywall. Thus, the call for DMHIs to be available to anyone at no charge is aspirational rather than a current reality.
Our search for illustrative studies representing each of the four types of digital interventions showed us that we need more studies with underrepresented groups (such as Black and Indigenous populations). We also need to consider implementing a stepped care model, as they do in the UK, in which people with mild and moderate symptoms are offered DMHIs (9,47). Those who do not respond to them are then provided access to live therapists.
This updated taxonomy can also be used to address the needs of underserved populations. Despite the number of research studies that focus on DMHIs, there are very few studies that focus on underserved populations. Developing culturally adapted DMHIs within the context of this taxonomy could help test their effectiveness and increase the likelihood of sharing these DMHIs with as many underserved populations as possible. For example, Caplan et al. (48) described the development of a culturally adapted mental health mobile app to prevent depression among low-income primary care participants in the Dominican Republic. And Tighe et al. (49) reported that a suicide prevention app culturally adapted for Aboriginal and Torres Strait Islander youth participants in Australia, “was deemed effective, acceptable, and culturally appropriate” (p. 1).
Conclusions
Although there are effective treatments currently available for many mental health conditions, the prevalence of these conditions in the general population has not decreased (50). It is important to reach a larger proportion of the population with evidence-based interventions. Treatment interventions alone are unlikely to reduce prevalence sufficiently. Preventive interventions that reduce incidence are also needed. In this article, we have provided illustrations of both levels of intervention. DMHIs have the potential to reach large numbers of people and provide access to mental health resources to those who need it the most. As Bettis et al. (51) state, “there is immense opportunity to enhance the quality of emotion-regulation interventions and expand their reach to populations with limited access to mental health care resources through digital intervention delivery tools” (p. 15). We should systematically work to fill in a grid of digital interventions in which columns represent specific health conditions (depression, smoking, obesity, etc.) and rows represent languages. We encourage clinical and research teams to focus on developing and testing any of the four types of DMHIs and share their findings in the literature. Those DMHIs that have been found effective can then use the Internet to share them with people locally and with similar populations elsewhere. This will allow us to not only “Think globally, Act locally” but also “Share globally”.
Acknowledgments
Funding: None.
Footnote
Peer Review File: Available at https://mhealth.amegroups.com/article/view/10.21037/mhealth-23-6/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://mhealth.amegroups.com/article/view/10.21037/mhealth-23-6/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Lawes-Wickwar S, McBain H, Mulligan K. Application and Effectiveness of Telehealth to Support Severe Mental Illness Management: Systematic Review. JMIR Ment Health 2018;5:e62. [Crossref] [PubMed]
- Muñoz RF, Chavira DA, Himle JA, et al. Digital apothecaries: a vision for making health care interventions accessible worldwide. Mhealth 2018;4:18. [Crossref] [PubMed]
- Muñoz RF, Bunge EL, Chen K, et al. Massive open online interventions: A novel model for delivering behavioral-health services worldwide. Clinical Psychological Science 2016;4:194-205. [Crossref]
- Committee on Fostering Healthy Mental, Emotional, and Behavioral Development Among Children and Youth, Board on Children, Youth, and Families. Development in children and youth: A national agenda. Washington, D.C.: National Academies Press; 2019.
- Mohr DC, Vella L, Hart S, et al. The Effect of Telephone-Administered Psychotherapy on Symptoms of Depression and Attrition: A Meta-Analysis. Clin Psychol (New York) 2008;15:243-53. [Crossref] [PubMed]
- Batastini AB, Paprzycki P, Jones ACT, et al. Are videoconferenced mental and behavioral health services just as good as in-person? A meta-analysis of a fast-growing practice. Clin Psychol Rev 2021;83:101944. [Crossref] [PubMed]
- Villalobos BT, Dueweke AR, Orengo-Aguayo R, et al. Patient perceptions of trauma-focused telemental health services using the Telehealth Satisfaction Questionnaire (TSQ). Psychol Serv 2023;20:107-21. [Crossref] [PubMed]
- Frank HE, Grumbach NM, Conrad SM, et al. Mental health services in primary care: Evidence for the feasibility of telehealth during the COVID-19 pandemic. J Affect Disord Rep 2021;5:100146. [Crossref] [PubMed]
- Moshe I, Terhorst Y, Philippi P, et al. Digital interventions for the treatment of depression: A meta-analytic review. Psychol Bull 2021;147:749-86. [Crossref] [PubMed]
- Muñoz RF, Aguilera A, Schueller SM, et al. From online randomized controlled trials to participant preference studies: morphing the San Francisco Stop Smoking site into a worldwide smoking cessation resource. J Med Internet Res 2012;14:e64. [Crossref] [PubMed]
- World Health Organization. Classification of digital health interventions [Internet]. Geneva; 2018. Report No. WHO/RHR/18.06. Available online: https://apps.who.int/iris/bitstream/handle/10665/260480/WHO-RHR-18.06-eng.pdf?sequence=1&isAllowed=y
- Classen B, Tudor K, du Preez E, et al. An Integrative Review of Contemporary Perspectives on Videoconference-Based Therapy-Prioritising Indigenous and Ethnic Minority Populations in the Global South. J Technol Behav Sci 2021;6:545-58. [Crossref] [PubMed]
- McGuire TG, Miranda J. New evidence regarding racial and ethnic disparities in mental health: policy implications. Health Aff (Millwood) 2008;27:393-403. [Crossref] [PubMed]
- Lu W, Todhunter-Reid A, Mitsdarffer ML, et al. Barriers and Facilitators for Mental Health Service Use Among Racial/Ethnic Minority Adolescents: A Systematic Review of Literature. Front Public Health 2021;9:641605. [Crossref] [PubMed]
- Zhao L, Chen J, Lan L, et al. Effectiveness of Telehealth Interventions for Women With Postpartum Depression: Systematic Review and Meta-analysis. JMIR Mhealth Uhealth 2021;9:e32544. [Crossref] [PubMed]
- Spruill TM, Friedman D, Diaz L, et al. Telephone-based depression self-management in Hispanic adults with epilepsy: a pilot randomized controlled trial. Transl Behav Med 2021;11:1451-60. [Crossref] [PubMed]
- Stewart RW, Orengo-Aguayo RE, Cohen JA, et al. A Pilot Study of Trauma-Focused Cognitive-Behavioral Therapy Delivered via Telehealth Technology. Child Maltreat 2017;22:324-33. [Crossref] [PubMed]
- Lopez L, Vázquez FL, Torres ÁJ, et al. Long-Term Effects of a Cognitive Behavioral Conference Call Intervention on Depression in Non-Professional Caregivers. Int J Environ Res Public Health 2020;17:8329. [Crossref] [PubMed]
- Lock J, Couturier J, Matheson BE, et al. Feasibility of conducting a randomized controlled trial comparing family-based treatment via videoconferencing and online guided self-help family-based treatment for adolescent anorexia nervosa. Int J Eat Disord 2021;54:1998-2008. [Crossref] [PubMed]
- Berrouiguet S, Baca-García E, Brandt S, et al. Fundamentals for Future Mobile-Health (mHealth): A Systematic Review of Mobile Phone and Web-Based Text Messaging in Mental Health. J Med Internet Res 2016;18:e135. [Crossref] [PubMed]
- Mantani A, Kato T, Furukawa TA, et al. Smartphone Cognitive Behavioral Therapy as an Adjunct to Pharmacotherapy for Refractory Depression: Randomized Controlled Trial. J Med Internet Res 2017;19:e373. [Crossref] [PubMed]
- Aguilera A, Bruehlman-Senecal E, Demasi O, et al. Automated Text Messaging as an Adjunct to Cognitive Behavioral Therapy for Depression: A Clinical Trial. J Med Internet Res 2017;19:e148. [Crossref] [PubMed]
- Barrera AZ, Hamil J, Tandon D. Integrating SMS Text Messages Into a Preventive Intervention for Postpartum Depression Delivered via In-Home Visitation Programs: Feasibility and Acceptability Study. JMIR Form Res 2021;5:e30995. [Crossref] [PubMed]
- Eysenbach G. The law of attrition. J Med Internet Res 2005;7:e11. [Crossref] [PubMed]
- Aguilera A, Hernandez-Ramos R, Haro-Ramos AY, et al. A Text Messaging Intervention (StayWell at Home) to Counteract Depression and Anxiety During COVID-19 Social Distancing: Pre-Post Study. JMIR Ment Health 2021;8:e25298. [Crossref] [PubMed]
- Karyotaki E, Ebert DD, Donkin L, et al. Do guided internet-based interventions result in clinically relevant changes for patients with depression? An individual participant data meta-analysis. Clin Psychol Rev 2018;63:80-92. [Crossref] [PubMed]
- Harper Shehadeh MJ, Abi Ramia J, Cuijpers P, et al. Step-by-Step, an E-Mental Health Intervention for Depression: A Mixed Methods Pilot Study From Lebanon. Front Psychiatry 2020;10:986. [Crossref] [PubMed]
- Otero P, Hita I, Torres ÁJ, et al. Brief Psychological Intervention Through Mobile App and Conference Calls for the Prevention of Depression in Non-Professional Caregivers: A Pilot Study. Int J Environ Res Public Health 2020;17:4578. [Crossref] [PubMed]
- Nygren T, Brohede D, Koshnaw K, et al. Internet-based treatment of depressive symptoms in a Kurdish population: A randomized controlled trial. J Clin Psychol 2019;75:985-98. [Crossref] [PubMed]
- Lindegaard T, Seaton F, Halaj A, et al. Internet-based cognitive behavioural therapy for depression and anxiety among Arabic-speaking individuals in Sweden: a pilot randomized controlled trial. Cogn Behav Ther 2021;50:47-66. [Crossref] [PubMed]
- Fitzsimmons-Craft EE, Taylor CB, Graham AK, et al. Effectiveness of a Digital Cognitive Behavior Therapy-Guided Self-Help Intervention for Eating Disorders in College Women: A Cluster Randomized Clinical Trial. JAMA Netw Open 2020;3:e2015633. [Crossref] [PubMed]
- Buntrock C, Ebert DD, Lehr D, et al. Effect of a Web-Based Guided Self-help Intervention for Prevention of Major Depression in Adults With Subthreshold Depression: A Randomized Clinical Trial. JAMA 2016;315:1854-63. [Crossref] [PubMed]
- Martínez P, Rojas G, Martínez V, et al. Internet-based interventions for the prevention and treatment of depression in people living in developing countries: A systematic review. J Affect Disord 2018;234:193-200. [Crossref] [PubMed]
- Karyotaki E, Riper H, Twisk J, et al. Efficacy of Self-guided Internet-Based Cognitive Behavioral Therapy in the Treatment of Depressive Symptoms: A Meta-analysis of Individual Participant Data. JAMA Psychiatry 2017;74:351-9. [Crossref] [PubMed]
- Schure MB, Lindow JC, Greist JH, et al. Use of a Fully Automated Internet-Based Cognitive Behavior Therapy Intervention in a Community Population of Adults With Depression Symptoms: Randomized Controlled Trial. J Med Internet Res 2019;21:e14754. [Crossref] [PubMed]
- Andrade AL, de Lacerda RB, Gomide HP, et al. Web-based self-help intervention reduces alcohol consumption in both heavy-drinking and dependent alcohol users: A pilot study. Addict Behav 2016;63:63-71. [Crossref] [PubMed]
- Barrera AZ, Wickham RE, Muñoz RF. Online prevention of postpartum depression for Spanish- and English-speaking pregnant women: A pilot randomized controlled trial. Internet Interv 2015;2:257-65. [Crossref] [PubMed]
- Lara MA, Tiburcio M, Aguilar Abrego A, et al. A four-year experience with a Web-based self-help intervention for depressive symptoms in Mexico. Rev Panam Salud Publica 2014;35:399-406. [PubMed]
- Muñoz RF, Barrera AZ, Delucchi K, et al. International Spanish/English Internet smoking cessation trial yields 20% abstinence rates at 1 year. Nicotine Tob Res 2009;11:1025-34. [Crossref] [PubMed]
- Leykin Y, Aguilera A, Torres LD, et al. Interpreting the outcomes of automated internet-based randomized trials: example of an International Smoking Cessation Study. J Med Internet Res 2012;14:e5. [Crossref] [PubMed]
- Ebert DD, Franke M, Zarski AC, et al. Effectiveness and Moderators of an Internet-Based Mobile-Supported Stress Management Intervention as a Universal Prevention Approach: Randomized Controlled Trial. J Med Internet Res 2021;23:e22107. [Crossref] [PubMed]
- Sander L, Rausch L, Baumeister H. Effectiveness of Internet-Based Interventions for the Prevention of Mental Disorders: A Systematic Review and Meta-Analysis. JMIR Ment Health 2016;3:e38. [Crossref] [PubMed]
- Rigabert A, Motrico E, Moreno-Peral P, et al. Effectiveness of online psychological and psychoeducational interventions to prevent depression: Systematic review and meta-analysis of randomized controlled trials. Clin Psychol Rev 2020;82:101931. [Crossref] [PubMed]
- Muñoz RF, Le HN, Barrera AZ, et al. Leading the charge toward a world without depression: perinatal depression can be prevented. Arch Womens Ment Health 2021;24:807-15. [Crossref] [PubMed]
- Fish JN, Mittal M. Mental Health Providers During COVID-19: Essential to the US Public Health Workforce and in Need of Support. Public Health Rep 2021;136:14-7. [Crossref] [PubMed]
- National Academies of Sciences, Engineering, and Medicine. Tools for supporting emotional wellbeing in children and youth [Internet]. Available online: https://nap.nationalacademies.org/resource/other/dbasse/wellbeing-tools/interactive/
- Palacios J, Adegoke A, Wogan R, et al. Comparison of outcomes across low-intensity psychological interventions for depression and anxiety within a stepped-care setting: A naturalistic cohort study using propensity score modelling. Br J Psychol 2023;114:299-314. [Crossref] [PubMed]
- Caplan S, Sosa Lovera A, Veloz Comas E, et al. A Mobile App to Prevent Depression Among Low-Income Primary Care Patients in the Dominican Republic: Sociocultural Adaptations. J Transcult Nurs 2020;31:413-24. [Crossref] [PubMed]
- Tighe J, Shand F, McKay K, et al. Usage and Acceptability of the iBobbly App: Pilot Trial for Suicide Prevention in Aboriginal and Torres Strait Islander Youth. JMIR Ment Health 2020;7:e14296. [Crossref] [PubMed]
- Global, regional, and national burden of 12 mental disorders in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Psychiatry 2022;9:137-50. [Crossref] [PubMed]
- Bettis AH, Burke TA, Nesi J, et al. Digital Technologies for Emotion-Regulation Assessment and Intervention: A Conceptual Review. Clin Psychol Sci 2022;10:3-26. [Crossref] [PubMed]
Cite this article as: Pineda BS, Mejia R, Qin Y, Martinez J, Delgadillo LG, Muñoz RF. Updated taxonomy of digital mental health interventions: a conceptual framework. mHealth 2023;9:28.


