Mixed methods evaluation of pediatric telehealth equity for patients/families who communicate in languages other than English
Highlight box
Key findings
• Patients/families who communicate in languages other than English were underrepresented among pediatric telehealth encounters and encounters were concentrated among few providers. Clinicians and families who communicate in languages other than English describe similar telehealth technology challenges across the telehealth care process but also successes in telehealth care.
What is known and what is new?
• Several studies have now documented telehealth disparities for patient populations that communicate in languages other than English. This study provides novel information about the concentration of telehealth encounters with patients who communicate in languages other than English among relatively few providers. This suggests that particular attributes of the providers and/or the clinics where they work facilitate telehealth success with this patient population and offers additional potential interventions to promote telehealth equity.
What is the implication, and what should change now?
• Promoting telehealth equity requires addressing technology barriers and increasing the readiness of providers/clinics for telehealth in languages other than English.
Introduction
Emerging research demonstrates telehealth disparities for patients who communicate in languages other than English (LOE) (1-3). Synchronous video telehealth encounters replacing in-person encounters were a key tool in initial coronavirus disease 2019 (COVID-19) pandemic mitigation strategies resulting in rapid expansion of telehealth care throughout US pediatric healthcare (4,5). Attention to the issue of inequitable access to telehealth for patients/families who communicate in LOE is urgently needed because telehealth is expected to remain an important tool in delivering care as its use was already increasing prior to the pandemic (6). Recent systematic reviews support the use of telehealth, finding that patients receiving care via telehealth have comparable or better outcomes than patients receiving in person care (7,8) and that generally patients are satisfied with telehealth (9). As care delivery models evolve to incorporate more telehealth, a better understanding of pediatric telehealth use with families who communicate in LOE is needed to inform interventions to promote telehealth equity.
There are more than 25 million people in the US with limited English proficiency, and Spanish-speaking parents comprise the majority of caregivers in pediatric healthcare settings who communicate in LOE (10,11). Children with caregivers who communicate in LOE experience disparities in healthcare access and quality (12,13) and disparate telehealth use could exacerbate existing disparities. The association of language barriers with lower digital/technology literacy and limited health literacy may place patients/families who communicate in LOE at particular risk (14,15). Accordingly, the purpose of this study was to (I) describe outpatient video telehealth encounters by language in a quaternary children’s hospital system; and (II) to explore the perspectives of clinical providers, staff, and Spanish-speaking parents to inform improvements in telehealth use and quality for patients/families who communicate in LOE. We present this article in accordance with the STROBE and SRQR reporting checklists (available at https://mhealth.amegroups.com/article/view/10.21037/mhealth-22-43/rc).
Methods
Study design and data sources
We conducted a mixed methods study utilizing the following data sources related to telehealth care in a large, academic children’s hospital health system: (I) cross-sectional electronic health record (EHR) data for outpatient video telehealth encounters from April 2020-July 2021 conducted by a physician or advanced practice provider [nurse practitioner or physician assistant (APP)]; (II) qualitative interviews with clinical staff who conducted/supported outpatient LOE telehealth encounters; (III) qualitative interviews with Spanish-speaking parents who attended telehealth encounters with their child. The study health system includes a network of hospitals, emergency departments, and outpatient care centers serving approximately 280,000 patients annually. Based on EHR data from 2019, 11.5% of patient encounters were with patients/families who communicate in LOE. Video telehealth encounters are accessed via the patient portal and utilize a video application external to the EHR to conduct the encounter. Language interpreters were technologically integrated into the telehealth video-conferencing platform in August 2020. Prior to this, providers utilized a phone interpreter on speakerphone while doing video encounters needing interpretation. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by Colorado Multiple Institutional Review Boards (IRB Organization #: IORG0000433, Panel A IRB#: IRB00000648, Panel B IRB#: IRB00000650, Panel C IRB#: IRB00000651, Panel D IRB#: IRB00002760, Panel S IRB#: IRB00006846) and individual consent for this retrospective quantitative analysis was waived. Interview participants completed an oral informed consent process via a waiver of documentation of informed consent.
Electronic health record data
Abstracted telehealth encounter data included: patient medical record number, encounter date, time and department, provider name, and patient language. Telehealth encounters were classified as a LOE encounter if the patient’s preferred healthcare language was not English OR the EHR flag for interpreter needed was set to ‘yes’. LOE encounters were stratified by language to Spanish vs. other languages, based on the predominance of Spanish language encounters. Of note we refer to this patient population as communicating in languages other than English as the term limited English proficiency is no longer preferred. Encounters were also stratified by specialty category: primary care, adolescent/family planning, medical subspecialty (e.g., pulmonary) and surgical subspecialty (e.g., otolaryngology) and miscellaneous (e.g., maternal/fetal medicine, radiology). We separated Adolescent/Family Planning from Primary Care as adolescents often attend appointments on their own or with limited parental involvement; thus, parent language needs status may not be relevant. For some analyses, we stratified providers by the number of LOE telehealth encounters they conducted during the study period into typical (<10 encounters) vs. high LOE provider (≥10 LOE encounters). 10 LOE encounters represented the 80th percentile for number of LOE encounters among providers with at least one LOE encounter. We also stratified providers according to Spanish language skills. Providers who had completed the hospital qualification process to communicate in Spanish were classified as qualified bilingual staff (QBS-Spanish).
Semi-structured Interviews
Interviews with providers and other clinical staff providing telehealth support conducted from October 2020 to March 2021 until thematic saturation was reached. Interviews were conducted by 2 bilingual (English/Spanish) physicians (authors LRD, DAT). We purposively sampled among high LOE providers as we wanted to identify successes and challenges during LOE telehealth encounters among providers with more experience. We selected participants to have variation in specialty, provider type (physician/APP) and QBS-Spanish status. After completing an interview, providers were asked to refer staff members for participation who could provide additional information about telehealth processes and experiences in that clinical area. All potential clinical staff participants were contacted up to 3 times via email to participate and those who provide verbal consent via a waiver of documentation of informed consent completed 30–60 minutes interviews via Zoom with one of the study co-investigators (LRD/DT). Interviews asked about experiences with telehealth with patients/families LOE over time, experiences with technical support and interpretation, and perceptions of family experiences.
Interviews with parents of children <18 years with a preferred healthcare language of Spanish and a telehealth encounter in the previous 6 months were conducted from April-May 2021, using purposive sampling until thematic saturation was reached. Interviews were conducted by a bilingual (English/Spanish)/bicultural Latina professional research assistant (CG). Our sampling strategy included the creation of six strata based on encounters in primary care vs. specialty care and the number of all outpatient telehealth encounters in 2020 for each patient (1, 2–3, >3). We randomly sorted patients into each of these six strata and then contacted families by phone up to three times for each stratum to ensure at least one parent interview participant per stratum. Following verbal consent, a bilingual English/Spanish research staff member interviewed participants for 30–60 minutes via phone. Interviews asked parents about their experiences with telehealth technology, interactions during telehealth encounters and their intention to continue using telehealth.
Digital interview recordings were transcribed and translated (as applicable) by a commercial transcription company and de-identified prior to coding. Parent interview transcripts included both the original Spanish-language transcript and English translation to allow for coding/analysis in the original language and cross-checking of translation accuracy.
Statistical analysis
All statistical analyses were conducted using R version 3.4.1 software (R Foundation for Statistical Computing, Vienna, Austria) (16). We summarized telehealth encounters by language and provider characteristics (specialty, high LOE and QBS-Spanish) status using Wilcoxon rank-sum tests, two-sample t-tests, and Fisher’s exact tests. Linear mixed models were used to test for differences in total encounter time between providers. There were no missing EHR data elements as abstracted data fields include automated fields (e.g., department) or required fields (e.g., language).
We used an exploratory qualitative approach and thematic content analysis to understand LOE telehealth experiences among clinical staff and families. Qualitative data analysis was completed using Dedoose, an online qualitative analytics program (17). Four coders (two physicians (authors LRD, LW), a medical student, and a professional research assistant (author CG) reviewed all transcripts to develop preliminary codes and based on these used an iterative consensus process to determine clear definition of codes and consistent application by all coders. During initial development and use of the codebook, two coders coded three transcripts. The remaining transcripts had one primary coder and a secondary verification coder. Rather than utilizing a measure of intercoder reliability, we used established methods for addressing differences in coding due to multiple coders by addressing all coding discrepancies and reconciling them with discussion and consensus (18,19). Themes present in both clinical staff and parent interviews were identified through team discussions of all coded transcripts. Member checking was completed with clinical telemedicine leadership with familiarity with both clinical staff and patient feedback on health system telehealth.
Results
Quantitative results
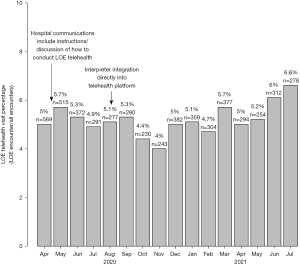
During the 16-month study period, 102,387 telehealth encounters meeting inclusion criteria were conducted by 1,133 providers; 5% (n=5,165) of which were LOE encounters. About half (55%) of telehealth providers conducted at least one LOE encounter. Among providers with at least one LOE telehealth encounter, the median number of LOE encounters was 3 (interquartile range: 1,8) and the number of encounters ranged from 1 to 308. 83% (n=4,298) of LOE telehealth encounters were with patients/families with a preferred healthcare language of Spanish. The next three most common languages for LOE telehealth encounters were American Sign Language (2.8% of LOE encounters, n=144), Arabic (1.5% of LOE encounters, n=80) and Vietnamese (1.1% of LOE encounters, n=56). Figure 1 displays the percentage of LOE telehealth encounters by month during the study period. Table 1 compares English and LOE telehealth encounter by specialty and time. Percent of LOE telehealth significantly differed by specialty with the highest percentage in adolescent/family planning (10%) and the lowest in surgical subspecialty (3%) and miscellaneous (2%), P<0.001. Mean encounter time for LOE encounters was slightly less than English encounters {38 [standard deviation (SD): 25] vs. 40 (SD: 21) minutes, respectively, P=0.0498}.
Table 1
| Characteristic | English encounters (n=97,222) | LOE encounters (n=5,165) | P value |
|---|---|---|---|
| Encounter specialty, n [%] | <0.0001 | ||
| Adolescent/family planning | 10,369 [90] | 1,134 [10] | |
| Medical subspecialty | 79,927 [96] | 3,747 [4] | |
| Primary care | 1,956 [93] | 141 [7] | |
| Surgical subspecialty | 3,264 [97] | 103 [3] | |
| Miscellaneous | 1,706 [98] | 40 [2] | |
| Encounter time, minutes, mean ± SD | 40±21 | 38±25 | 0.0498 |
LOE, language other than English; SD, standard deviation.
Table 2 compares LOE telehealth encounters between typical and high LOE providers. The 11% of all telehealth providers who were high LOE providers completed 71% (n=3,692) of all LOE telehealth encounters. Encounter time was not statistically different between high LOE providers and typical LOE providers. There were 31 providers identified as QBS-Spanish comprising 8% of high LOE providers and 4% of typical LOE providers. Table 3 compares LOE telehealth encounters between high LOE providers by QBS-Spanish status. Mean encounter time was longer for QBS-Spanish high LOE providers than non-QBS high LOE providers {58 [interquartile range (IQR): 42, 74) vs. 41 (IQR: 35, 46) minutes, respectively, P=0.0495}. Table 4 compares LOE telehealth encounters between typical LOE providers by QBS-Spanish status. There was no difference in encounter time by QBS-Spanish status among typical LOE providers.
Table 2
| Characteristic | Typical LOE providers* (n=499) | High LOE providers** (n=128) | P value |
|---|---|---|---|
| Provider specialty, n [%] | <0.0001 | ||
| Adolescent/family planning | 18 [56] | 14 [44] | |
| Medical subspecialty | 380 [77] | 111 [23] | |
| Primary care | 46 [98] | 1 [2] | |
| Surgical subspecialty | 39 [95] | 2 [5] | |
| Miscellaneous | 16 [100] | – | |
| Number of LOE encounters, n [%] | 1,473 [29] | 3,692 [71] | |
| Number of LOE encounters per provider, median (IQR) | 2 (1 to 4) | 17 (12 to 28) | <0.0001 |
| Percent of provider telehealth that was LOE encounters, median (IQR) | 4 (2 to 9) | 8 (5 to 13) | <0.0001 |
| LOE encounter time, minutes, mean (95% CI) | 38 (35 to 42) | 42 (38 to 47) | 0.1328 |
*, typical LOE providers includes only those providers with at least one but less than 10 LOE telehealth encounters; **, high LOE providers had ≥10 LOE telehealth encounters. LOE, language other than English; IQR, interquartile range; CI, confidence interval.
Table 3
| Characteristic | Non-QBS Spanish high LOE provider (n=120) | QBS-Spanish high LOE provider (n=10) | P value |
|---|---|---|---|
| Number of LOE encounters per provider, median (IQR) | 16 (12 to 29) | 19 (14 to 24) | 0.6596 |
| Percent of provider telehealth that was LOE encounters, median (IQR) | 7 (5 to 13) | 18 (13 to 29) | 0.0007 |
| LOE encounter time, minutes, mean (95% CI) | 41 (35 to 46) | 58 (42 to 74) | 0.0495 |
**, high LOE providers had ≥10 LOE telehealth encounters. LOE, language other than English; QBS, qualified bilingual staff; IQR, interquartile range.
Table 4
| Characteristic | Non-QBS Spanish typical LOE provider (n=478) | QBS-Spanish typical LOE provider (n=21) | P value |
|---|---|---|---|
| Number of LOE encounters, median (IQR) | 2 (1 to 4) | 1 (1 to 2) | 0.0043 |
| Percent of provider telehealth that was LOE encounters, median (IQR) | 4 (2 to 9) | 10 (4 to 17) | 0.0093 |
| LOE encounter time, minutes, mean (95% CI) | 38 (35 to 41) | 40 (23 to 56) | 0.8474 |
*, typical LOE providers includes only those providers with at least one but less than 10 LOE telehealth encounters. LOE, language other than English; QBS, qualified bilingual staff; IQR, interquartile range; CI, confidence interval.
Qualitative results
We conducted 25 qualitative interviews with clinical staff (n=13) and parents (n=12). Table 5 displays characteristics of participating clinical staff. Table 6 displays characteristics of parent participants and their children. Common themes identified across both clinical staff and parent interviews were: (I) technology barriers affect access to and quality of telehealth care; (II) clinical staff and parents are uncertain about the future role of telehealth for patients/families who communicate in LOE; (III) the well-known impact of language barriers on in-person healthcare access and quality for patients who communicate in LOE is also evident in telehealth. Table 7 displays example quotes for each theme.
Table 5
| Characteristic | Total n=13 |
|---|---|
| Woman, n [%] | 12 [92] |
| Role, n [%] | |
| Physician/advanced practice provider | 10 [77] |
| Other clinical staff | 3 [23] |
| Specialty, n [%] | |
| Adolescent/family planning | 1 [8] |
| Medical subspecialty | 8 [62] |
| Primary care | 3 [23] |
| Surgical subspecialty | 1 [8] |
| Experience with in-person care for patients that communicate in LOE, rating scale: 1 (low) to 10 (high), median (IQR) | 8 (8 to 10) |
LOE, language other than English; IQR, interquartile range.
Table 6
| Characteristic | Total n=12 |
|---|---|
| Parent age, years, mean ± SD | 42±5 |
| Parent education, n [%] | |
| Less than high school | 10 [83] |
| High school or above | 2 [17] |
| Parent years in US, mean ± SD | 21±6 |
| Annual family income, n [%] | |
| <$20,000 | 3 [25] |
| $20,000–$40,000 | 5 [42] |
| >$40,000 | 3 [25] |
| Did not report/unknown | 1 [8] |
| Parent reported English proficiency, n [%] | |
| Very well | – |
| Well | 1 [8] |
| Not well/not at all | 11 [92] |
| Parent confidence filling out forms* (health literacy marker), n [%] | |
| Extremely/quite a bit confident (likely adequate health literacy) | 7 [58] |
| Somewhat/little bit confident (likely limited health literacy) | 5 [42] |
| Child health insurance, n [%] | |
| Medicaid | 11 [92] |
| Children’s health insurance program | 1 [8] |
*, Sarkar et al. (20). SD, standard deviation.
Table 7
| Theme 1: technology barriers |
| Quote 1: It’s not because there haven’t been a couple of families who speak English who have had troubles, but it is far, far less, and it seems like the ability to troubleshoot or to get quick support, or something has been better for families who have spoken English. |
| Quote 2: The other thing that came out was that many of our non-English-speaking families declined to use (the patient portal). So, they may not be hooked up through (the patient portal). So we really got a huge glimpse of the disparity between our English-speaking patients and our non-English-speaking patients and their ability and prep of even being able to access telehealth services at baseline. |
| Quote 3: I think that the use of technology proficiency is probably for some non-English-speaking families is much more challenging, and they’re just not nearly as familiar sometimes with using the technical platform that we use. So, we found many times the family can’t get onto the application, and then we might spend 45 minutes ourselves trying to provide technical support to the family. So, then when we finally get to the visit, it’s like you only have 15 minutes left. And so, either that puts you behind for the next patient or you have to reschedule the family, which it oftentimes is again another whole deal. |
| Quote 4: And the medical assistants have been really helpful in trying to do tech checks, or call them, but I would say there’s a good percentage of our providers who are ending up calling the patient, because it just makes the visit very hard. And so, I don’t think that’s necessarily a bad thing, because I can do a great visit on the phone, but I know that that’s still a barrier for some people, if they really need to see a patient. |
| Quote 5: So, we actually ran into a lot of issues like, okay, we figured out how to put in an interpreter, but the family doesn’t have good internet or they don’t have a phone that can do the tech. So, we really heard more of families’ inability to have the technology in the home in place to support a video/audio telehealth visit. |
| Quote 6: The lag in the video, the lag in the audio, if you’re using an interpreter, I think that makes it even more challenging because sometimes it’s just more confusing. Sometimes I’m not sure exactly; did the interpreter hear me right? Did the family hear the interpreter? Sometimes not being sure about what’s going on. |
| Quote 7: System wide the initial barrier was that there wasn’t a great way to add an interpreter into a telehealth visit. That was the huge barrier in the beginning. It’s still not wildly convenient, but it’s much, much easier. And, that truly was the biggest system-wide barrier that we were facing that I see benefit from. |
| Quote 8: So, maybe something in the last month or two has changed. When we had the tech-check individuals calling the families ahead, that was really helpful. But then they took those, I think they redeployed those individuals back to whatever they did before |
| Quote 9: We as a clinic, we just identify. If a family asks for a tech check they may during the time of setup or if they just haven’t had a telehealth before we automatically will call, reach out to them, and as I stated, two of my MAs are bilingual. So, that really helps connecting with the family before the visit and letting them know we’re here. We’re ready to support you. We know how to interact with you. We know how to talk to you. You can talk to us. You can ask your questions. |
| Quote 10: Sí, es que nunca había activado, nunca había activado MyChart, entonces no sabía que yo ya tenía un password que ellos me habían programado, pero como yo no me lo sabía, ellos fueron muy amables y me ayudaron con un nuevo password y fue todo muy excelente.Yes, it was never activated, I had never activated MyChart, so I didn’t know that I already had a password that they had programmed for me, but since I didn’t know it, they were very kind and helped me with a new password and it was all very excellent. |
| Quote 11: La primera consulta sí me fue complicado un poco conectarme para la cita y ya en la última ya no, pues ya con la práctica ya sé cómo.The first consultation was a bit difficult for me to connect for the appointment and in the last one no longer because, with the practice, I already know how. |
| Quote 12: A veces siento como que mi internet está un poco lento y no le entiendo bien al que me está traduciendo.Sometimes I feel like my internet is a little slow, and I don’t understand the person who is translating |
| Quote 13: A veces la conexión fallaba un poquito por el problema de que todos están en la escuela usando el internet.Sometimes the connection failed a little bit because of the problem that everyone is in school using the internet. |
| Theme 2: future role of telehealth |
| Quote 14: I think it’s more convenient for a lot of (families). I think that it’s the weather’s bad, or. And even just seeing some families in their natural—the kids are in their more naturalistic environment. That has a double-edged sword to it sometimes because they can be misbehaving or whatnot. But I think there are a lot of families who do really like it, and I think that it’s a great option to help us do the best that we can. |
| Quote 15: Por el hecho de que no perdí tanto tiempo y por el hecho de que no salí y por el hecho de que era tiempo de nieve, ya estaba nevando y pues me quité la preocupación de saber que mi hija estaba enferma y que la que fue atendida.Due to the fact that I didn’t waste so much time, and due to the fact I didn’t go out, and due to the fact that it was snowing weather, it was already snowing, and well I took away the worry of knowing that my daughter was sick and that she was taken care of. |
| Quote 16: I would talk with the patient-What works best for you? What makes you most comfortable? What do you want to do? There are families that I’ve had who prefer, as long as they can come in person, they like to do that better. So, if that’s what their preference is then I’ll accommodate them… |
| Quote 17: If you didn’t do (the physical exam), they don’t feel like you did anything, so. So, I don’t think the western culture is like that. I think we’re perfectly fine with this style of interaction. But I think that there are other cultures in this world where when you are a medical provider, or a physician, or whatever, you’re a healer, and that your presence and your touch means something to the family. |
| Quote 18: I personally would rather see a patient in clinic. I know everybody’s different. Some people have really enjoyed telehealth. I feel like it’s somewhat adequate, but in some ways, with our kids, that sometimes, getting accurate weight checks, it doesn’t happen, even with the home scale. Sometimes you just can’t visualize what’s really going on. |
| Quote 19: Yo sé que en persona la van a atender mejor y la van a poder examinar mejor; pero ahorita como está lo del virus y no hay vacuna para ella todavía, yo sí prefiero que esté ella por videollamada.I know that in-person they will take better care of her and they will be able to examine her better; but right now as the virus is and there is no vaccine for her yet, I do prefer that she is on a video call. |
| Quote 20: Pues se parecen en que, si el doctor te diagnostica algo, pues te recetan, o sea, te hace las mismas preguntas que te haría en el consultorio, o sea, la única diferencia pues que no estás en persona, pero está bien.Well, they are similar in that, if the doctor diagnoses something, they prescribe you, that is, they ask you the same questions they would ask you at the doctor’s office, that is, the only difference is that you are not in person, but it is fine. |
| Quote 21: Pues, en persona, pues, ya a él lo ven, ¿cómo decir? Lo ven, este, es mejor…Porque lo están viendo, están viendo, pongamos, si no tiene moretones, o su respiración.Well, in person, well, they can check him, how can I say it? They check him, it’s better…Because they’re checking him, they’re looking at him, let’s say, to see if he doesn’t have any bruises, or his breathing. |
| Quote 22: Pues sabe que las veces que hemos ido en persona, los intérpretes que están ahí, obvio que le interpretan a uno mejor y está en persona, así que en esa parte pues obvio, sí está mejor en persona.Well, you know that the times we’ve been there in person, the interpreters who are there, they interpret someone better and it’s in person, so in that part, obviously, it’s better in person. |
| Quote 23: (Me sentí) pues rara, porque la doctora no la va a estar revisando ni tocando el área que le duele, así que ya cuando la doctora la revisó y le dijo: “okay, ¿todavía te duele el estómago?” “Sí”, “¿en dónde?”. Y dijo: “tu mamá tiene que tocarte, haz presión en la parte alrededor de su ombligo, que es el área donde le duele”, y pues quería estar segura que le estaba haciendo correcto yo como ella quería, así que sí pregunté si lo estaba haciendo bien; ella dijo que sí.Well, (I felt) strange, because the doctor’s not going to be checking her or touching the area that hurts, so when the doctor checked her and said, “okay, do you still have a stomachache?” “Yes”, “where?”. And she said, “Your mom has to touch you, put pressure on the part around her navel, which is the area where it hurts.” And I wanted to be sure that I was doing it right as she wanted, so I did ask if I was doing it right; she said yes. |
| Theme 3: language barriers in healthcare |
| Quote 24: And so—especially in our line of work, but in anything—in terms of explaining things, I think we do—whether we like it or not—when we’re speaking through interpreters, we kind of leave a lot out, just because they’re like, “Well, I’m supposed to just talk in short sentences.” And so, it limits your ability to really communicate and establish a rapport with a patient, and limits their understanding a lot. |
| Quote 25: Esto entiendo que tiene mucha importancia el traductor porque a veces uno como hispano habla mucho, entonces el traductor te pide, siempre nos dicen que hablemos en frases cortas y algo claro. Y pues uno empieza a hablar, hablar y a hablar, y es difícil para los traductores; entonces, tal vez si fueran un poco más pacientes con las personas.I understand that the translator is very important because sometimes as Hispanics we talk a lot, then the translator asks you, they always tell us to speak in short and clear sentences. And so you start to talk, talk and talk, and it’s difficult for the translators; so maybe if they were a little more patient with people. |
| Quote 26: Es mejor cuando va a algún intérprete en persona, que cuando usan la tecnología para interpretar. De hecho, hasta cuando voy, que tengo que ir al hospital es complicado con los mismos intérpretes cuando usan la tablet. A veces los mismos intérpretes no dicen lo que yo estoy diciendo, como que cambian palabras y la doctora no puede entender bien lo que yo estoy diciendo; otras veces se corta mucho el sonido o no escuchan y tenemos que volver a repetir lo que decimos.It’s better when you go to an interpreter in person than when you use technology to interpret. In fact, even when I go, that I have to go to the hospital, it’s complicated with the same interpreters when they use the tablet. Sometimes, the same interpreters do not say what I am saying, as they change words and the doctor cannot understand well what I am saying; other times the sound is cut a lot or they do not hear me and we have to repeat what we say. |
| Quote 27: I think that’s why I like working with the (in-person staff) interpreters I know so well, because they’re so good. They know exactly what I’m saying, and they can interpret it very well…and I don’t feel—like with (telephone interpretation), I feel like I just have to say kind of short sentences that are very factual and have no real vagueness or grayness about it, that medicine in our conversations usually do. |
| Quote 28: I mean, ideally, we’d have extra time, but we’ve never been able to—we’ve always said we wanted extra time for non-English speakers, but we’ve never figured out a workflow way to make that happen. Again, because I just sorta see anybody that gets referred, so we don’t know who’s gonna be non-English-speaking and who’s not. |
| Quote 29: Because, I think it’s both a technology hurdle and a language barrier. And, the technology hurdle already seems so big for our providers and then you add the language barrier and it just seems like, oh, this is insurmountable. I can’t get past it. |
| Quote 30: And I just think for some of my families, just trusting medical providers and the medical system is hard anyway, and I think layering in this extra layer of technology between you and your healthcare provider just creates more issues related to trust. |
| Quote 31: I would say that most of our patients who are non-English speaking did not get plugged in to telehealth…we certainly, like those Spanish-speaking providers, when they shifted to telehealth certainly saw their Spanish-speaking patients in telehealth. |
Theme 1: technology barriers
Clinical staff talked at length about technology barriers negatively impacting LOE telehealth encounters (Table 7, Quote 1). Telehealth access was limited by use of the patient portal as the access point as many families were often not enrolled in or facile using the portal (Quote 2). While there were frequent descriptions of significant efforts to enable video telehealth (Quote 3), conversion to a phone encounter when these efforts were unsuccessful was also described (Quote 4). Clinical staff reported limited access to devices, internet connections with insufficient bandwidth to support video and limited technology literacy compromised telehealth quality (Quote 5). They reported audio or video lag made communication via interpreters especially challenging (Quote 6). Clinical staff reported changing workflows for using an interpreter during telehealth were frustrating, but that eventual integration into the telehealth platform positively affected LOE telehealth encounters (Quote 7). Clinical staff positively viewed family access to central technological support (referred to as a “tech-check”). Some clinical staff expressed concern that centralized resources dedicated to supporting families with technology barriers were being scaled back, while others reported that their clinical area had implemented workflows to support families when needed (Quotes 8,9).
Families reported similar technology challenges. Many reported that they were unfamiliar with the patient portal and needed support to access telehealth (Quote 10), though a few reported no difficulty. Families reported positive experiences with the technology support for telehealth and often reported that for subsequent encounters they did not need support (Quote 11). Some families reported technical support was provided by clinical staff and others reported an English-speaking teenager in the household who helped. Most families reported using their phone to access telehealth, and some described concerns about the internet connection or technologic delays with the interpretation (Quotes 12,13). While clinical staff described negative experiences at length and expressed significant frustration, families did not express the same level of frustration, and technology barriers did not figure as prominently in their perceptions of telehealth care.
Theme 2: future role of telehealth
Both clinical staff and parents endorsed telehealth as a necessary response to the COVID-19 pandemic and cited advantages such as avoiding travel in adverse weather and decreased transportation and time burden for appointments (Quotes 14, 15). Clinical staff reported they envisioned telehealth would likely become a routine part of care, but that families should be allowed to choose the appointment modality (Quote 16). Some noted that families’ cultural perceptions may decrease willingness to continue telehealth (Quote 17). Some clinical staff expressed a personal preference for in-person care (Quote 18). Many parents reported they would prefer not to continue telehealth after the pandemic improved (Quote 19), though many did report an overall positive experience with telehealth (Quote 20). Most parents expressed a preference for in-person care as they felt in-person appointments allowed for a more thorough exam and assessment of their children and that interpretation was better (Quote 21, 22). Some parents did report that for appointments that were more frequent and for which the physical exam was less important (e.g., mental health therapy) that they were more willing to continue telehealth. One concern that influenced parents’ willingness to continue telehealth was their role in the physical exam, specifically supporting virtual physical exam maneuvers that could change clinical decision-making (Quote 23).
Theme 3: language barriers in healthcare
Well-known barriers to care for patients who communicate in LOE were evident in clinical staff and family interviews. Participants reported challenges when communicating via an interpreter and that this compromised communication quality (Quotes 24, 25). Both clinical staff and families expressed a preference for in-person interpreters to mitigate negative impacts of interpreter-mediated communication (Quotes 26, 27). Some families and clinical staff discussed experiences of long wait times for interpreters. Many clinical staff reported LOE encounters took longer, and this could disrupt the flow of a clinic day (Quote 28). A few clinical staff reported that the concomitant challenges of telehealth and language barriers were overwhelming and worried this could further patient/family mistrust in healthcare (Quotes 29, 30). Some clinical staff interviews included discussions of how bilingual providers often had a distinct role in care of patients who communicate in LOE (Quote 31). Families reported positive experiences with bilingual providers when available.
Discussion
In this study, we found patients with families who communicate in LOE were underrepresented among telehealth encounters over 16-months from April 2020 to July 2021, compared with their representation among health system patient volume in 2019. We also found that LOE telehealth encounters were concentrated among few providers. Our qualitative inquiry demonstrated that technology barriers were an important contributor to disparate telehealth use. Technology barriers included potentially modifiable barriers at the health system level, such as the interface for telehealth access, and barriers at the family level that may be more difficult to overcome, such as high-speed internet access and digital literacy. The telehealth use disparities that we identified and the role of technology barriers are consistent with other studies (1,2,21). Our finding that the majority of LOE telehealth encounters were conducted by few providers, however, suggests particular attributes of the providers and/or the clinics where they work facilitate telehealth success with families who communicate in LOE and offers additional potential interventions to promote telehealth equity. Our qualitative results suggest that promoting telehealth equity should incorporate flexibility for families to choose the appointment modality, while at the same time ensuring that telehealth improvement activities address technology barriers and the unique ways culture and language impact telehealth. Our study also underscores the persistent need for broad attention to healthcare equity for patients who communicate in LOE as challenges in providing telehealth reflected general healthcare disparities for these patients.
Our study and others demonstrate the critical role of addressing technology barriers to reduce telehealth disparities. The healthcare digital divide for patients who communicate in LOE was well-described pre-pandemic, thus pandemic telehealth disparities are not surprising (22-24). As in our healthcare system, video telehealth is often offered through the patient portal. Patient portal enrollment and use is lower among populations who are racial/ethnic minorities, low-income or communicate in LOE, so portal-based telehealth processes may marginalize them (24-26). Interventions to close gaps in patient portal use have had limited success as their design often did not account for the diversity of patients served by healthcare systems (27). Patient portals are uncommonly available in non-English languages and often require high levels of heath and digital literacy for optimal usability (22,26-29). Though the patient portal is available in Spanish in our system, both clinical staff and parents reported lack of enrollment in or difficulties using the patient portal for accessing telehealth as key barriers. Technological support was often effective in overcoming difficulties with the patient portal and families often learned from their experiences, reporting greater success at accessing subsequent telehealth appointments. Thus, having standardized processes and resource investment for providing technology support to patients who communicate in LOE, and a method for identifying first time telehealth users who are more likely to have difficulties, are critically important. There is also a need for healthcare information technology design that reflects the diversity of potential users. Finally, high-speed internet access is likely to remain inequitable for quite some time, though smartphone access is similar across populations (30). Thus, efforts to reduce bandwidth required for digital healthcare interactions and optimize experiences via mobile devices are also important.
Our data also demonstrate the need for provider and clinic-level interventions to improve telehealth equity for families communicating in LOE. Early challenging experiences with telehealth may have contributed to persistent disparate use of telehealth with patients/families who communicate in LOE due to negativity bias. Psychological research demonstrates that negative experiences often have a greater impact on subsequent behavior and emotions than positive ones (31). Our findings demonstrate that some providers and clinics were able to overcome negativity bias that may have been present. This is consistent with literature in organizational and implementation science that organizational context and individual characteristics are important in the adoption of new or evidence-based practices (32,33). Though in this study we had limited ability to systematically identify specific clinic or provider characteristics associated with greater adoption of telehealth with families who communicate in LOE, our data suggest that pre-existing expertise in the care of patients in LOE, such as being a bilingual provider, may have facilitated LOE telehealth encounters. Some clinical staff reported bilingual providers facilitated LOE telehealth encounters by volunteering to to conduct visits with Spanish-speaking families and families expressed they placed value on access to bilingual providers. The supply of bilingual providers, however, at our health system, and in health systems across the country, is far below the need (34,35). Thus, while bilingual providers may create a facilitative environment for the care of patients who communicate in LOE, reducing telehealth disparities for these patients requires a comprehensive approach to ensure bilingual providers are not unduly burdened and patients have access to all providers.
While this study was focused on telehealth disparities, our findings reflect common themes that contribute to healthcare disparities for patients who communicate in LOE. Clinical staff expressed the time that these encounters took as a significant barrier, with time required for interpretation as a key reason. Interestingly though, we found time for LOE encounters was similar or even less than English encounters. Also, among high LOE QBS-Spanish providers, however, mean encounter time was the greatest of all providers, even though these encounters would not have required interpreter-mediated communication. The literature supports the mismatch we found. Providers often perceive an increased time burden for LOE encounters, but when encounter time has been measured an increased time burden has not been consistently demonstrated, varies by interpretation modality, and may be confounded by medical and/or social complexity in addition to language barriers (36-38). Shorter or equivalent length of LOE telehealth encounters may, however, indicate worse communication quality. Though interpreter use has been consistently associated with improved patient safety and communication, interpreter mediated communication quality challenges identified in prior research include less question elicitation, briefer explanations and education on the diagnosis and treatment plan and less social conversations, which are important for trust and rapport building (39-41). Discrepancies in perceived and reported encounter time have important implications for widening acceptability and use of telehealth in LOE.
This study is not without limitations. Our automated EHR query could only identify encounters with a potential need for language accommodation. We could not distinguish how language barriers were addressed or if the encounter was actually conducted in English, despite having a LOE preference in the EHR. We also could not distinguish audio-only vs. video telehealth encounters. Only telehealth encounters scheduled as video encounters were included in the study. However, if the encounter was converted to audio-only after scheduling this would not have been identifiable in our data. Other research has shown that LOE telehealth encounters are more likely to be audio-only (3). It is unknown, however, if an audio-only encounter is inferior to video telehealth. Additionally, telehealth processes in our health system, including those specific to LOE telehealth, were iteratively improved in 2020 and early 2021 in response to lessons learned during COVID-19 pandemic-related telehealth expansion. The full effect of these improvements may not have been realized during the time period included in the study. Additionally, telehealth challenges are likely higher for LOE encounters compared with English encounters, but this study did not compare the experience of English and non-English-speaking families. Lastly, mostly women clinical staff members participated in our qualitative study. We believe this reflects the gender distribution in pediatric healthcare. For example, in our system 71% of medical staff (physicians, APPs) are women. In this study we did not examine if provider characteristics other than language (e.g., gender, race/ethnicity, age) were associated with LOE telehealth encounters, but this is of interest for future work.
Conclusions
Our study provides important information about telehealth with families who communicate in LOE. Our quantitative data demonstrate disparate use of telehealth with these families with LOE telehealth encounters concentrated among relatively few providers. The qualitative data provided additional information about key barriers that may have contributed to telehealth disparities and how particular providers and clinics navigated these barriers to provide telehealth in LOE. While ultimately families who communicate in LOE may not desire telehealth at the same rate as other populations, promoting equitable telehealth care still requires investment to address technology barriers and increase the readiness of providers and clinics to provide telehealth care in LOE. The relative success of some providers in LOE telehealth encounters indicates that there are likely feasible short-term changes that can be enacted within health systems to promote telehealth equity. At the same time, longer-term changes to improving usability and inclusivity of healthcare technology platforms and access to high-speed internet by all populations should be pursued.
Acknowledgments
Funding: This work was supported by institutional funds from the Children’s Hospital Colorado Clinical and Operational Effectiveness and Patient Safety Small Grants Program (Principal Investigators: Thompson/DeCamp). The funder had no direct involvement in the study design, collection, analysis and interpretation of data, the writing of the report, or the decision to submit the article for publication.
Footnote
Reporting Checklist: The authors have completed the STROBE and SRQR reporting checklists. Available at https://mhealth.amegroups.com/article/view/10.21037/mhealth-22-43/rc
Data Sharing Statement: Available at https://mhealth.amegroups.com/article/view/10.21037/mhealth-22-43/dss
Peer Review File: Available at https://mhealth.amegroups.com/article/view/10.21037/mhealth-22-43/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://mhealth.amegroups.com/article/view/10.21037/mhealth-22-43/coif). This project was funded by the Children’s Hospital Colorado Clinical and Operational Effectiveness and Patient Safety Small Grants Program (Principal Investigators: LRD/DAT). This funding provided salary support for CG and CP to fulfill their role in the proposed work. CO was supported to complete this work by the work by the NIH/ NCATS SPROUT-CTSA Collaborative Telehealth Network Grant, #U01TR002626. Effort on this project was provided in-kind by LRD, DAT, LW. DAT reports receiving an honoraria and reimbursement of travel costs in 2022 by Johns Hopkins All Children’s Hospital to teach pediatric residents as part of a curriculum on health equity in which she discussed the care of patients/families whose healthcare communication is in a language other than English. DAT also serves as the Associate Medical Director of the Children’s Hospital Colorado Research Institute and as part of her duties co-chairs the Diversity, Health Equity, and Inclusion in Research Committee for the Research Institute. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by Colorado Multiple Institutional Review Boards (IRB Organization #: IORG0000433, Panel A IRB#: IRB00000648, Panel B IRB#: IRB00000650, Panel C IRB#: IRB00000651, Panel D IRB#: IRB00002760, Panel S IRB#: IRB00006846) and individual consent for this retrospective quantitative analysis was waived. Interview participants completed an oral informed consent process via a waiver of documentation of informed consent.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Schenker RB, Laguna MC, Odisho AY, et al. Are We Reaching Everyone? A Cross-Sectional Study of Telehealth Inequity in the COVID-19 Pandemic in an Urban Academic Pediatric Primary Care Clinic. Clin Pediatr (Phila) 2022;61:26-33. [Crossref] [PubMed]
- Rodriguez JA, Saadi A, Schwamm LH, et al. Disparities In Telehealth Use Among California Patients With Limited English Proficiency. Health Aff (Millwood) 2021;40:487-95. [Crossref] [PubMed]
- Hsueh L, Huang J, Millman AK, et al. Disparities in Use of Video Telemedicine Among Patients With Limited English Proficiency During the COVID-19 Pandemic. JAMA Netw Open 2021;4:e2133129. [Crossref] [PubMed]
- Mann DM, Chen J, Chunara R, et al. COVID-19 transforms health care through telemedicine: Evidence from the field. J Am Med Inform Assoc 2020;27:1132-5. [Crossref] [PubMed]
- Demeke HB, Pao LZ, Clark H, et al. Telehealth Practice Among Health Centers During the COVID-19 Pandemic - United States, July 11-17, 2020. MMWR Morb Mortal Wkly Rep 2020;69:1902-5. [Crossref] [PubMed]
- Curfman A, McSwain SD, Chuo J, et al. Pediatric Telehealth in the COVID-19 Pandemic Era and Beyond. Pediatrics 2021;148:e2020047795. [Crossref] [PubMed]
- Flodgren G, Rachas A, Farmer AJ, et al. Interactive telemedicine: effects on professional practice and health care outcomes. Cochrane Database Syst Rev 2015;2015:CD002098. [Crossref] [PubMed]
- Albritton J, Ortiz A, Wines R, et al. Video Teleconferencing for Disease Prevention, Diagnosis, and Treatment: A Rapid Review. Ann Intern Med 2022;175:256-66. [Crossref] [PubMed]
- Jeminiwa R, Hohmann L, Qian J, et al. Impact of eHealth on medication adherence among patients with asthma: A systematic review and meta-analysis. Respir Med 2019;149:59-68. [Crossref] [PubMed]
- U.S Census Bureau. American Community Survey 1-year Estimates: Langauge Spoken at Home 2017. Available online: https://factfinder.census.gov/faces/tableservices/jsf/pages/productview.xhtml?pid=ACS_10_1YR_S1601&prodType=table
- AMN Healthcare Language Services. 2021 Healthcare World Index. Coppell, TX, USA: AMN Healthcare, Inc., 2021.
- Flores GCommittee On Pediatric Research. Technical report--racial and ethnic disparities in the health and health care of children. Pediatrics 2010;125:e979-e1020. [Crossref] [PubMed]
- Eneriz-Wiemer M, Sanders LM, Barr DA, et al. Parental limited English proficiency and health outcomes for children with special health care needs: a systematic review. Acad Pediatr 2014;14:128-36. [Crossref] [PubMed]
- López L, Tan-McGrory A, Horner G, et al. Eliminating disparities among Latinos with type 2 diabetes: Effective eHealth strategies. J Diabetes Complications 2016;30:554-60. [Crossref] [PubMed]
- Nouri SS, Avila-Garcia P, Cemballi AG, et al. Assessing Mobile Phone Digital Literacy and Engagement in User-Centered Design in a Diverse, Safety-Net Population: Mixed Methods Study. JMIR Mhealth Uhealth 2019;7:e14250. [Crossref] [PubMed]
-
Foundation for Statistical Computing - SocioCultural Research Consultants L. Dedoos Home Page Manhattan Beach, CA: SocioCultural Research Consultants, LLC., 2021. Available online: https://www.dedoose.com/.
- Patton MQ. Qualitative Research & Evaluation Methods. Third ed. United States of America: Sage Publications, Inc., 2002.
- Barbour RS. Checklists for improving rigour in qualitative research: a case of the tail wagging the dog? BMJ 2001;322:1115-7. [Crossref] [PubMed]
- Sarkar U, Schillinger D, López A, et al. Validation of self-reported health literacy questions among diverse English and Spanish-speaking populations. J Gen Intern Med 2011;26:265-71. [Crossref] [PubMed]
- Tan-McGrory A, Schwamm LH, Kirwan C, et al. Addressing virtual care disparities for patients with limited English proficiency. Am J Manag Care 2022;28:36-40. [Crossref] [PubMed]
- López L, Green AR, Tan-McGrory A, et al. Bridging the digital divide in health care: the role of health information technology in addressing racial and ethnic disparities. Jt Comm J Qual Patient Saf 2011;37:437-45. [Crossref] [PubMed]
- Din HN, McDaniels-Davidson C, Nodora J, et al. Profiles of a Health Information-Seeking Population and the Current Digital Divide: Cross-Sectional Analysis of the 2015-2016 California Health Interview Survey. J Med Internet Res 2019;21:e11931. [Crossref] [PubMed]
- Wang Y, Do DP, Wilson FA. Immigrants' Use of eHealth Services in the United States, National Health Interview Survey, 2011-2015. Public Health Rep 2018;133:677-84. [Crossref] [PubMed]
- Ketterer T, West DW, Sanders VP, et al. Correlates of patient portal enrollment and activation in primary care pediatrics. Acad Pediatr 2013;13:264-71. [Crossref] [PubMed]
- Irizarry T, DeVito Dabbs A, Curran CR. Patient Portals and Patient Engagement: A State of the Science Review. J Med Internet Res 2015;17:e148. [Crossref] [PubMed]
- Grossman LV, Masterson Creber RM, Benda NC, et al. Interventions to increase patient portal use in vulnerable populations: a systematic review. J Am Med Inform Assoc 2019;26:855-70. [Crossref] [PubMed]
- Casillas A, Perez-Aguilar G, Abhat A, et al. Su salud a la mano (your health at hand): patient perceptions about a bilingual patient portal in the Los Angeles safety net. J Am Med Inform Assoc 2019;26:1525-35. [Crossref] [PubMed]
- Flower KB, Wurzelmann S, Tucker C, et al. Spanish-Speaking Parents' Experiences Accessing Academic Medical Center Care: Barriers, Facilitators and Technology Use. Acad Pediatr 2021;21:793-801. [Crossref] [PubMed]
- Anderson-Lewis C, Darville G, Mercado RE, et al. mHealth Technology Use and Implications in Historically Underserved and Minority Populations in the United States: Systematic Literature Review. JMIR Mhealth Uhealth 2018;6:e128. [Crossref] [PubMed]
- Larsen R. The contributions of positive and negative affect to emotional well-being. Psihologijske Teme 2009;18:247-66.
- Aarons GA, Sommerfeld DH, Walrath-Greene CM. Evidence-based practice implementation: the impact of public versus private sector organization type on organizational support, provider attitudes, and adoption of evidence-based practice. Implement Sci 2009;4:83. [Crossref] [PubMed]
- Greenhalgh T, Robert G, Macfarlane F, et al. Diffusion of innovations in service organizations: systematic review and recommendations. Milbank Q 2004;82:581-629. [Crossref] [PubMed]
- Diamond LC, Mujawar I, Vickstrom E, et al. Supply and Demand: Association Between Non-English Language-Speaking First Year Resident Physicians and Areas of Need in the USA. J Gen Intern Med 2020;35:2289-95. [Crossref] [PubMed]
- Fernández A, Pérez-Stable EJ. ¿Doctor, habla español? Increasing the Supply and Quality of Language-Concordant Physicians for Spanish-Speaking Patients. J Gen Intern Med 2015;30:1394-6. [Crossref] [PubMed]
- Guerrero N, Small AL, Schwei RJ, et al. Informing physician strategies to overcome language barriers in encounters with pediatric patients. Patient Educ Couns 2018;101:653-8. [Crossref] [PubMed]
- Fox MT, Godage SK, Kim JM, et al. Moving From Knowledge to Action: Improving Safety and Quality of Care for Patients With Limited English Proficiency. Clin Pediatr (Phila) 2020;59:266-77. [Crossref] [PubMed]
- Grover A, Deakyne S, Bajaj L, et al. Comparison of throughput times for limited English proficiency patient visits in the emergency department between different interpreter modalities. J Immigr Minor Health 2012;14:602-7. [Crossref] [PubMed]
- Gutman CK, Cousins L, Gritton J, et al. Professional Interpreter Use and Discharge Communication in the Pediatric Emergency Department. Acad Pediatr 2018;18:935-43. [Crossref] [PubMed]
- Riggs E, Brown S, Szwarc J, et al. Teach-Back in Interpreter-Mediated Consultations: Reflections from a Case Study. Health Lit Res Pract 2021;5:e256-61. [Crossref] [PubMed]
- Kotovicz F, Getzin A, Vo T. Challenges of Refugee Health Care: Perspectives of Medical Interpreters, Case Managers, and Pharmacists. J Patient Cent Res Rev 2018;5:28-35. [Crossref] [PubMed]
Cite this article as: DeCamp LR, Williams L, Palmer C, Gorman C, Olson C, Thompson DA. Mixed methods evaluation of pediatric telehealth equity for patients/families who communicate in languages other than English. mHealth 2023;9:24.