A feasibility pilot using a mobile personal health assistant (PHA) app to assist stroke patient and caregiver communication after hospital discharge
Introduction
Mobile health has grown exponentially over the past several years (1,2) due to the rapid adoption of smart phones and smart devices and higher mobile network speeds. Globally, mobile devices are interconnecting humans from previously disparate regions of the world. Such interconnectedness allows an unprecedented ability for improved communication for health, smart phone applications (apps) for monitoring and diagnosing disease, and improved communication between patients and health care providers (3).
Acute stroke presents several unique challenges for patients and health care providers. First, due to their deficits, stroke patients can have difficulty communicating, manipulating with dexterity, and learning about important medications and warning signs. Additionally, they incur burden on caretakers and family members and are more likely to have decreased health literacy (4,5). These issues, as well as patient satisfaction, factor into hospital readmission (6,7). Acute stroke care is critical, but poststroke/posthospital care including rehabilitation, medication and medication compliance, lifestyle and behavioral changes, and strict follow-up with pertinent health care providers is as important to a patient’s overall outcome
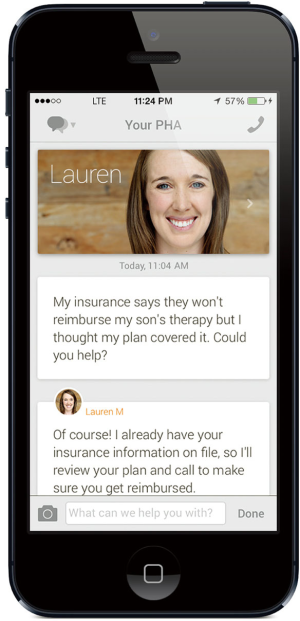
This acquired disability presents an opportunity to use mobile health as a tool to help posthospital stroke care. Remote Health Services with financial backing from our institution developed the intervention app. The app provided a personal health assistant (PHA) to keep in communication with the patient and help organize medication compliance, comply with follow-up instructions, navigate health insurance issues, conduct appointment scheduling, and communicate the patients’ questions to health care providers and nurses. The PHA was a human employee of Remote Health Services, usually with some background in health care. They were available 24 h a day, 7 days a week, and were able to be contacted by texting or voice through the PHA app.
Our study examined ischemic stroke patients who used the PHA app, and we hypothesized that the PHA would improve postdischarge satisfaction and decrease rehospitalization for patients recovering from stroke.
Methods
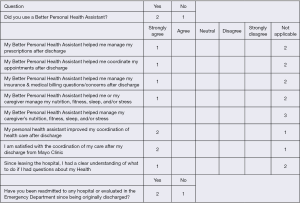
The study was approved by the Mayo Clinic institutional review board. All patients underwent formal consent, and if they unable due to stroke deficits, their caregiver or legal authorized representative was approached for written consent in the study. We aimed to study a consecutive series of acute stroke patients at our tertiary comprehensive stroke center. All patients received standard of care stroke discharge instructions and institutional educational materials as well as 30 days of free PHA service though the app (Figure 1). Patients were called 30 days after hospital discharge and administered a survey asking how well the app helped the patient and their caregiver in a variety of domains (Figure 2). The initial study design was a prospective, observational randomized study in which 30 patients who were hospitalized for acute stroke or transient ischemic attack (TIA) were to be randomized by block randomization into a control or interventional arm.
Patients were screened over a 3-month period in 2015. Initial screening was done by physicians, advanced registered nurse practitioners, or physician assistants in the admitting team, with full screening and consent completed by the research coordinator. Inclusion criteria included hospital admission for stroke (ischemic or hemorrhagic) or TIA and age 18 years or older. Additionally, the patient or caregiver was required to have owned a suitable smartphone device with the ability to download the American Heart Association/American Stroke Association “Spot a Stroke F.A.S.T” app. Essentially, this allowed an assessment of whether the patient had sufficient dexterity and cognition to utilize the intervention app. Patients were excluded if any of these criteria were not met, if they were discharged to a palliative care or hospice environment, or if they refused participation.
Results
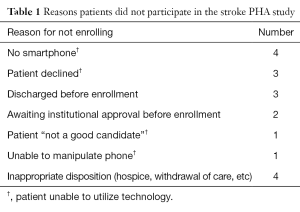
We screened 21 patients and enrolled 3 patients during the study period. Two of the 3 patients used the app (the third did not use it while in rehab). Of the 2 patients who used the app, the response was favorable, though many survey questions were designated “not applicable” by the patients. Both patients who used the app presented to the emergency department within 30 days. One was discharged, and the other was readmitted (Figure 2). The study was prematurely terminated due to lack of further venture capital funding for Remote Health Services. This led to termination of the study before switching to the block design control arm which would receive the AHA FAST app. Therefore, this study only investigated the PHA app. Among the 18 patients who were screened but did not participate, 9 did not participate due to an inability to utilize the technology (Table 1).
Full table
Discussion
Mobile health is revolutionizing the world due to widely available high-speed internet and cellular communication networks. This provides significant advantages to patients over having to drive to physical appointments. To our knowledge, this is the first study that utilized a PHA app to examine poststroke discharge patient satisfaction and readmission rates through a mobile app. Further, we found that poststroke patients had a variety of reasons for not enrolling in the study, including inability to manipulate the device, no access to a smartphone, other study design impediments, or declination to enroll (Table 1). This is critical information for future study design. About half of the patients were excluded because they were unable to use the technology in some way, including stroke deficits. This provides important insights about the unique nature of stroke as a disease, which can make communication difficult from a motor and dexterity standpoint or a verbal (dominant hemisphere language) neurological standpoint. Both patients who did use the app were very pleased with their coordination of care and delivery of information on behalf of themselves and their caregivers. Both patients who did use the app presented to the emergency department within 30 days, and 1 of them was readmitted for stroke. This study demonstrates that a PHA app on a mobile phone may be a viable option for some, but not all, stroke patients and can improve patient discharge, education, and coordination satisfaction.
The major limitation of this study is the small final sample size of the pilot. However, the study revealed that stroke patients have a low consent/enrollment rate for smartphone and app technology, which is an important finding for future mobile health app studies. Further, the small sample size makes it difficult to make overall conclusions about the use of a PHA through the app for standard clinical practice. However, among the limited data we saw a preliminary high patient satisfaction rate. Another limitation was that the study was ended prematurely due to termination of funding. However, given the rapid development of mobile health research, such as the Apple Health Kit and nontraditional (i.e., non-NIH) funding, such as venture capital, this study highlights the importance of the tribulations of doing mobile health research until more traditional funding (NIH) is provided. Given the emergence of apps and other technology, venture funding has become a reality for some smaller start-up companies, such as Remote Health Services.
Conclusions
Mobile health is a rapidly growing area of future health care. However, it poses unique challenges for conducting research due to rapid changes in technology and nontraditional modes of research funding. Mobile health challenges also include concerns about protected patient information (i.e., PHI, security, HIPAA compliance, and FDA medical device classification). We also found this challenges standard institutional review board approval processes because apps are not typically reviewed as typical research “devices”. Such research challenges are likely to be encountered by other academic centers. Finally, patient compliance, willingness, and ability to participate remain future metric for future mobile health study success. As medical providers and app developers, we should also approach the patient-centered vantage point during app development. Age and low socioeconomic status are also important risk factors for stroke and unfortunately risk factors for not having access to or using smartphone and mobile health technology. Future larger studies are critical in determining whether mobile health apps and PHAs can help patients with chronic illnesses, such as stroke.
Acknowledgements
Remote Health Services provided the personal health assistant at no cost to the patient or health care provider.
Footnote
Conflicts of Interest: A Dole and P Maler: Employed at Remote Health Services; the other authors have no conflicts of interest to declare.
References
- The complicated, evolving world of MHealth. Healthcare Global. 2015. Accessed 2016 July 6. Available online: http://www.healthcareglobal.com/technology/1870/INFOGRAPHIC-The-Complicated,-Evolving-World-of-mHealth
- National Ambulatory Medical Care Survey: 2010 Summary Tables. Centers for Disease Control and Prevention. 2010. Accessed 2016 Apr 15. Available online: http://www.cdc.gov/nchs/data/ahcd/namcs_summary/2010_namcs_web_tables.pdf
- Steinhubl SR, Muse ED, Topol EJ. Can mobile health technologies transform health care? JAMA 2013;310:2395-6. [Crossref] [PubMed]
- Sanders K, Schnepel L, Smotherman C, et al. Assessing the impact of health literacy on education retention of stroke patients. Prev Chronic Dis 2014;11:E55. [Crossref] [PubMed]
- Atteih S, Mellon L, Hall P, et al. Implications of stroke for caregiver outcomes: findings from the ASPIRE-S study. Int J Stroke 2015;10:918-23. [Crossref] [PubMed]
- Lichtman JH, Leifheit-Limson EC, Jones SB, et al. Preventable readmissions within 30 days of ischemic stroke among Medicare beneficiaries. Stroke 2013;44:3429-35. [Crossref] [PubMed]
- Asplund K, Jonsson F, Eriksson M, et al. Patient dissatisfaction with acute stroke care. Stroke 2009;40:3851-6. [Crossref] [PubMed]
Cite this article as: Siegel J, Edwards E, Mooney L, Smith C, Peel JB, Dole A, Maler P, Freeman WD. A feasibility pilot using a mobile personal health assistant (PHA) app to assist stroke patient and caregiver communication after hospital discharge. mHealth 2016;2:31.