
Applying the behaviour change wheel to assess the theoretical underpinning of a novel smartphone application to increase physical activity in adults with spinal cord injuries
Highlight box
Key findings
• Accessercise may be a practical intervention for adults with spinal cord injuries (SCI), offering users the capability, opportunity, and motivation to undertake physical activity and reduce sedentary behaviours with high behaviour change potential.
What is known and what is new?
• Limited studies have concentrated on mHealth interventions to encourage physical activity in people with SCI. Thus, this study adds to a growing body of literature suggesting that Accessercise has the potential to improve physical activity within and outside of the UK, reducing the burden on healthcare services and staff, offering an alternative mHealth intervention that could reach disadvantaged adults with SCI.
What is the implication, and what should change now?
• The app could be easily targeted at harder-to-reach groups if promoted broadly, such as in rehabilitation, community, leisure centres, and workplaces. Consequently, in the next phase of the research, the effectiveness of Accessercise to facilitate the desired behaviour change should be assessed, such as via a randomised control trial.
Introduction
It is well-documented that individuals with spinal cord injury (SCI), which can be caused by damage to the structure and function of the spinal cord resulting in sensory, motor, and autonomic dysfunction below the site of injury (1), undertake lower levels of physical activity compared to the general population (2). According to Martin Ginis and colleagues (3), individuals with SCI should undertake at least 20 minutes of moderate-to-vigorous aerobic activity alongside strength training exercises twice weekly. It has been estimated that only 50% of people with SCI undertake any form of physical activity (e.g., pushing, transferring) (4), which has likely reduced further due to restrictions imposed by the coronavirus disease 2019 (COVID-19) pandemic (5). Indeed, during the pandemic, individuals with SCI faced numerous additional barriers to accessing physical activity; they could not attend leisure facilities due to prolonged closures, as well as restricted access to health services and specialised professionals that provide training in appropriate home-based exercises (5). These COVID-19 related barriers add to several barriers to physical activity that have been consistently reported in the literature, including lack of sufficient transportation (6,7) and fewer opportunities to undertake appropriate physical activities (8). Therefore, interventions that simultaneously address multiple barriers to physical activity unique to people with SCI are urgently needed (9).
Reduced physical activity levels can lead to an increased risk of secondary health complications, including worsening physiological and psychosocial health among those with SCI (10). This can negatively impact quality of life and participation in activities of daily living in this population (11,12). Regular physical activity is one behaviour that can assist individuals with SCI in managing and overcoming challenges, such as preventing poorer health outcomes (13). For example, participation in regular physical activity can improve physical fitness (e.g., cardiovascular endurance, muscle strength, body composition) and cardiometabolic health (e.g., obesity, hypertension, diabetes) (14,15). On this basis, given the low rates of physical activity and the risks of additional health complications among people with SCI, it is imperative to encourage participation in and offer sufficient access to physical activity (16).
In a recent systematic review and meta-analysis, physical activity interventions for people with physical disabilities had a small-to-medium effect on improving physical activity (17). Most physical activity interventions for people with SCI have been delivered in person (18,19) or over the telephone (20). For example, Ma and colleagues (19) demonstrated that, using a co-created behavioural intervention, physical activity can be increased in people with SCI when delivered in-person within the home and/or community. While in-person interventions are effective in increasing physical activity, COVID-19 restrictions resulted in mobility constraints, closure, and reductions in the capacities of exercise facilities (21,22), which presented a unique and unprecedented barrier. However, due to the significant access to digital technologies (e.g., computers, tablets, mobile phones) (23), there has been a proliferation of physical activity interventions that can be exclusively delivered remotely via mobile (or smartphone) technologies, which falls within the remit of mobile-enabled healthcare (mHealth). For instance, tele-exercise, defined as interventions that offer physical training and are provided remotely, such as weightlifting and stretching (24), are deemed a promising area of technology that may encourage sustainable physical activity participation in people with SCI (25,26).
mHealth interventions, such as smartphone applications (or apps), can support individuals to perform physical activities remotely in their own homes (27), reducing identified barriers to physical activity, including those resulting from the COVID-19 pandemic. For example, providing an intervention through an app can relieve transportation and built environmental barriers to access, which are significant for people with SCI (6). Moreover, the advanced processing power of smartphones makes them a practical approach for transmitting, tracking, and monitoring data on health-related outcomes (27). Given that smartphones are ubiquitous, it is estimated that there are now 3.5 billion users worldwide (28), mHealth interventions appear to be a favourable tool to support physical activity in people with SCI (29). Nevertheless, limited studies have concentrated on mHealth interventions to encourage physical activity in adults with SCI (30,31).
In addition to accessible modes of delivery, a further consideration in the development and evaluation of physical activity interventions in people with physical disabilities, including SCI, is that they should be underpinned by appropriate health behaviour change theory (17,32). Moreover, when designing and evaluating behaviour change interventions, key frameworks emphasise the significance of applying theory to inform intervention design (33,34). As a result, this approach can assist in ensuring that an intervention meets the needs of the end-users and is more likely to result in long-term behaviour change (35). Ensuring that complex health interventions are underpinned by appropriate theory is vital because behaviour change is notoriously challenging to initiate and requires sustained efforts (36,37). One reason is that behaviours are habitual, normative, and preventive (38). Habitual behaviours are often performed in stable situations or contexts (39) and are challenging to alter, as they are undertaken automatically without much thinking (40). Normative behaviours are based on powerful forces of traditional and social approval, and preventive behaviours commonly miss a salient immediate outcome (41). Therefore, given that behaviour change is extremely challenging to achieve, it is contended that behaviour change theories are imperative to design and evaluate such interventions (42,43).
Numerous theories of behaviour change exist, such as the health belief model (44,45), transtheoretical (stages of change) model (46-48), social cognitive theory (49-51), theory of reasoned action (52), and the theory of planned behaviour (TPB) (53,54). However, these theories focus on behavioural analysis of health-related issues and have been challenged for not sufficiently explaining variations in complex behaviour (55). In addition, these models have been criticised for concentrating on a relatively small number of constructs and neglecting more contextual and conscious processes (56). Additionally, it has been argued that these theories can only assist in predicting behaviour (57) and do not help to understand how behaviour change happens (58). More recently, the behaviour change wheel (BCW) (59,60) has been designed to overcome the limitations of previous behaviour change theories (61). The BCW is different from traditional theories because it considers the role of context, an aspect of behaviour which has been under-investigated in the past (62). Furthermore, the BCW has successfully informed interventions in numerous health contexts and has been reported to be advantageous in altering target health behaviours (63,64).
Specifically, the BCW synthesises 19 theoretical frameworks of behaviour change (59,60) identified in academic literature and arrived at by a consensus of behavioural theorists (65). At the core of the wheel is the capability, opportunity, motivation, and behaviour (COM-B) model (59,66), which postulates that changing behaviour is reliant upon three components: physical and psychological capability, physical and social opportunity, and reflective and automatic motivation (67,68). A mid ring on the BCW incorporates nine intervention functions (69,70), and the outer ring comprises seven policy options (71,72), which can support the delivery of the intervention functions (73). The BCW links influences on behaviour identified by the COM-B to potential intervention functions and policy categories (64).
On this basis, the overall aim of the current study was to assess the theoretical underpinning of a novel mHealth intervention that aims to improve physical activity in people with SCI, namely, the Accessercise (https://join.accessercise.com) smartphone fitness app. Specifically, using the BCW, we identify the “active ingredients” of the app, focusing on how and why this mHealth intervention could effectively improve physical activity (i.e., the target behaviour) in people with SCI, as well as how its capacity for behaviour change could be enhanced further.
Methods
Study design
The study mapped a novel smartphone fitness app, Accessercise, to an integrative theoretical framework of behavioural change, namely, the BCW. A team with clinical and research expertise in SCI, physical activity, and behaviour change was employed. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). As the study did not involve human participants due to the nature of the research design (i.e., secondary data), ethical approval was not required.
Intervention being evaluated
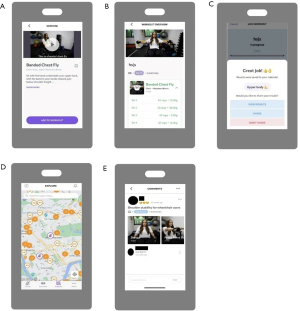
Accessercise, founded in 2021, is a novel fitness and healthy living smartphone app created specifically for people with disabilities. Accessercise aims to get people with disabilities fit, strong and healthy, offering users with several primary functions. Furthermore, Accessercise is asynchronous, allowing users to perform physical activity in numerous settings (e.g., gym, home, park) at their own pace and at a convenient time. First, the Accessercise application features a video library tailored to participants’ needs and impairments to help illustrate suitable exercises that are demonstrated by a role model with the same impairment (Figure 1A). Second, the app offers a track progress function where users can log workouts, track progress, and meet or exceed their goals (Figure 1B,1C, respectively). Third, an explore section exists where users can search a directory of fitness facilities ranked for accessibility (Figure 1D). Fourth, a social hub where users can connect with others, share their progress with followers and groups and be part of a diverse, supportive, and passionate community (Figure 1E). The overarching focus of this app is to offer educational knowledge, tracking abilities and behavioural prompts to increase physical activity among its users (namely, people with physical disabilities). The app was founded by Britain’s world champion Para-Powerlifter, Ali Jawad, multiple world champion sailor, Sam Brearey, and Financial Times top ranked European lawyer and AEQUO founding partner, Yulia Kyrpa.
Evaluation of behaviour change
To systematically evaluate the mechanisms of action (or active ingredients) of the Accessercise app that enable the target behaviour change (i.e., improved physical activity), the BCW was chosen as the underpinning theoretical approach.
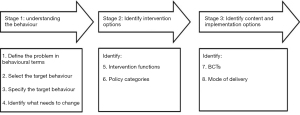
When developing and evaluating health behaviour change interventions using the BCW, Michie and colleagues (60) recommend that three stages, divided into eight steps, are adhered to (Figure 2). The first stage (steps 1-4) involves understanding the behaviour to be influenced and incorporates the COM-B model (74,75). The second stage (steps 5 and 6) identifies the intervention options (76,77), and the third stage (steps 7 and 8) identifies the content and implementation options (75,78). All stages and steps are summarised in-depth within corresponding sub-sections of the Results. For each step, the research team met to discuss their individual findings before reaching a group consensus.
Results
Stage 1: understanding the behaviour
This first stage involved understanding the problem to address in behavioural terms, specifically, “what the behaviour is”, “who is performing the behaviour”, and “what behaviours are required for behaviour change” These were all identified through the four-step process outlined below.
Step 1: define the problem in behavioural terms
To identify problems associated with physical activity in adults with SCI, a prospectively registered systematic review assessed the effectiveness of behaviour change interventions in this context (32). In addition, the literature regarding the barriers and facilitators to physical activity in this population was also reviewed (79,80). This information was used to define the problem as: how to improve physical activity in adults with SCI to meet recommended guidelines (at least 20 minutes of moderate to vigorous intensity-aerobic activity alongside strength training exercises twice per week) leading to reduced sedentary behaviours (Table S1).
It was identified that adults with SCI experienced problems with physical activity in a range of contexts, including at home, at the gym or outside. Thus, the location (or context) of the problem was defined. While healthcare professionals can guide behaviour change, it is the individual with SCI that needs to be actively involved in performing the behaviours required to meet recommended physical activity guidelines.
Step 2: select the target behaviour
The research team generated a list of 13 candidate behaviours relevant to the problem identified in step 1 that could bring about the desired outcome (i.e., improving physical activity to meet recommended guidelines, resulting in reduced sedentary behaviours) (Table S2). These behaviours were derived from literature outlining the barriers and facilitators to physical activity experienced by adults with SCI (Figure 3). These included lack of time (81), limited transportation, negative attitudes (6), motivation (82), and lack of accessibility to the affected population and trained professionals (83). The target behaviours were then prioritised by considering the following factors: (I) potential impact of changing the behaviour; (II) likelihood of shifting behaviours; (III) spillover or impact of change on other behaviours; and (IV) ease of measuring or monitoring the behaviour (Table S3). For each of these factors, the research team rated each as very promising, promising, unpromising but worth considering, or unacceptable as a behaviour to be targeted.

Several candidate behaviours were identified as promising or very promising across all four factors, including goal setting, increased self-confidence, changing beliefs about capabilities, increasing understanding of the amount or type of physical activity needed to achieve health benefits, improving the knowledge or awareness of physical activity opportunities or resources available, providing community support networks, planning strategies to overcome adverse effects, and overcoming negative past experiences.
Step 3: specify the target behaviour
The target behaviours were further specified by detailing who needed to perform the behaviour, when, where, how often, and with whom (Table S4). Specifically, the target behaviours should be directed at the individual with SCI enabling them to undertake physical activity independently.
Step 4: identify what needs to change
The COM-B model was used to identify what needs to change in the individual and/or environment to accomplish the desired changes in behaviour. This step was centred on the research expertise of the research team, as well as findings from appropriate literature (17).
Altogether, we identified that behavioural changes are required across all COM-B components for the target behaviour to occur (Table S5).
Capability
Physical capability (e.g., physical skills, strength, or stamina) which, in this context, was improving physical abilities to undertake appropriate physical activities. Psychological capability (e.g., knowledge, psychological skills, strength, or mental stamina), which could include improving problem solving abilities, as well as making suitable decisions related to physical activity.
Opportunity
Physical opportunity (e.g., time, resources, locations, cues, and physical affordance), which could involve access to appropriate facilities, equipment, and resources to undertake physical activity. Social opportunity (e.g., interpersonal influences, social cues, and cultural norms), such as social support from family, friends, and the community to engage in physical activity.
Motivation
Automatic (e.g., emotion reactions, desires, impulses, drive states, and reflex responses), which could involve the completion of weekly or monthly diaries to monitor performance and set goals. Reflective (e.g., self-conscious intentions plans and evaluations), such as holding beliefs that undertaking physical activity is achievable and will result in positive outcomes.
Stage 2: identify intervention options
Step 5: intervention functions
Based on the findings from the COM-B analysis in step 4, step 5 involved using the BCW to identify the most relevant intervention functions for each of the candidate behaviours (84,85). To identify which of these intervention functions were most appropriate, the research team used the affordability, practicability, effectiveness, acceptability, side-effects or safety, and equity (APEASE) criteria. Based on these criteria and consensus among the research team, seven of the nine intervention functions (i.e., education, persuasion, incentivisation, coercion, training, modelling, and enablement) were selected as suitable intervention functions to facilitate physical activity in adults with SCI (Table S6). The remaining intervention functions of restriction and environmental restructuring were considered impractical in the current context.
Education and training were deemed the most suitable intervention functions to address physical (i.e., better physical skills) and psychological (i.e., better knowledge of physical activity and its benefits) capability. For physical opportunity, training (i.e., create more time for the intervention and have cues or prompts as practice reminders) was considered the most appropriate, whereas for social opportunity, modelling (i.e., increase social support from others with SCI, as well as friends and family) was viewed as most suitable. For reflective motivation (i.e., positive beliefs), education, persuasion, incentivisation, coercion, modelling, and enablement were considered the most appropriate functions. While for automatic motivation (i.e., establishing a routine or habit), coercion, training, modelling, and enablement were chosen.
Step 6: policy categories
Seven policy categories to help support and enact the intervention functions were considered, namely, communication/marketing, guidelines, fiscal measures, regulation, legislation, service provision, and environmental/social planning (Table S7). After applying the APEASE criteria and following discussions amongst the research team, two policy categories were deemed most appropriate in this context: communication/marketing (e.g., using verbal, electronic communication, or flyers to create awareness of the benefits of physical activity) and service provision (e.g., establishing physical activity in various contexts and communities).
Stage 3: identify content and implementation options
Step 7: behaviour change techniques (BCTs)
Step 7 required identifying the most appropriate BCTs that can best deliver the intervention functions (step 5) and policy categories (step 6) (see also Table 1). First, the most frequently used BCTs were derived from the BCT Taxonomy v1 (BCTTv1), in which 93 BCTs are organised into 16 groupings (60). Second, the most relevant BCTs were considered in relation to the APEASE criteria. Third, after discussion with the research team, a final consensus on the included BCTs was undertaken (Table S8). Based on the intervention functions selected in step 5 (i.e., education, persuasion, incentivisation, coercion, training, modelling, enablement), the appropriate BCTs identified were goal setting (behaviour, outcome), action planning, review behaviour and outcome goal(s), feedback on (outcomes of) behaviour, self-monitoring of (outcomes of) behaviour, social support (unspecified, practical), instruction on how to perform the behaviour, demonstration of the behaviour, behavioural practice rehearsal, generalisation of a target behaviour, graded tasks, credible source, material incentive and reward (behavioural), social reward, and body changes.
Table 1
| Behaviour change technique | Intervention function(s) | Description of intervention component used in Accessercise | Capability | Opportunity | Motivation | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Physical | Psychological | Social | Physical | Reflective | Automatic | ||||||||||||
| Skills | Knowledge | Memory, attention & decision process | Behavioral regulation | Social influences | Environmental context & resources | Beliefs about consequences | Optimism | Beliefs about capabilities | Goals | Reinforcement | |||||||
| Goal setting (behaviour) | Enablement | Accessercise allows users to set goals to reduce their sedentary behaviours (e.g., build muscle, increase strength, flexibility, cardio) | * | * | |||||||||||||
| Goal setting (outcome) | Enablement | Monitoring of targets during and after using the Accessercise application | * | ||||||||||||||
| Action planning | Enablement | Users are encouraged to pre-schedule new workouts when first using Accessercise in a set context with a specific intensity, duration, and frequency | * | * | |||||||||||||
| Review behaviour goal(s) | Enablement | After completing a workout on Accessercise, behaviour goals can be reviewed by written feedback provided on the app | * | * | * | * | * | ||||||||||
| Review outcome goals | Enablement | Post-workouts, users can review their performance, allowing for opportunities to self-monitor progress | * | * | * | * | * | ||||||||||
| Feedback on behaviour | Education, persuasion, incentivisation, coercion, training | After completing workouts on Accessercise, users can access their performance (e.g., completed reps, sets) | * | * | * | * | |||||||||||
| Self-monitoring of behaviour | Education, Incentivization, coercion, training, enablement | Goal setting and monitoring are available to users during the Accessercise app | * | * | * | * | * | ||||||||||
| Self-monitoring of outcomes of behaviour | Education, incentivisation, coercion, training, enablement | Users could monitor their progress and receive a results form after completing each workout session on Accessercise | * | * | * | * | * | ||||||||||
| Feedback on outcomes of behaviour | Education, persuasion, incentivisation, coercion, training | Users are provided feedback after completing each workout on Accessercise, such as the number of repetitions/sets achieved | * | * | * | * | |||||||||||
| Social support (unspecified) | Enablement | Users are urged to use the self-health group feature on the Accessercise app by sharing their progress with other link-minded individuals | * | ||||||||||||||
| Social support (practical) | Enablement | The Accessercise app allows users to search a directory of fitness facilities ranked for accessibility | * | ||||||||||||||
| Instruction on how to perform the behaviour | Training | Accessercise provides written explanations and step-by-step instructions on how to undertake the exercises | * | * | |||||||||||||
| Demonstration of the behaviour | Training, modelling | Pre-recorded videos demonstrating the exercises are available on Accessercise when completing workouts | * | * | * | * | * | ||||||||||
| Behavioural practice rehearsal | Training | Users are offered the chance to practice the exercises in the real world (e.g., home, gym outside) when selecting workouts on Accessercise | * | * | * | * | |||||||||||
| Generalisation of a target behaviour | Enablement | An opportunity to participate at home, at the gym or outside are offered to all users when selecting a workout on Accessercise | * | * | * | * | |||||||||||
| Graded tasks | Enablement | Users have an option on Accessercise of increasing the intensity/frequency of the workouts | * | ||||||||||||||
| Credible source | Persuasion | Videos of each exercise are performed by a specialist living with the same disability, who explains the best and most appropriate method to undertaking the exercises | * | * | |||||||||||||
| Material incentive (behaviour) | Incentivisation | The users are offered the chance to purchase discounted products in the Accessercise web shop post-workouts | * | * | |||||||||||||
| Material reward (behaviour) | Incentivisation | An option to purchase discounted sports clothing, equipment, and accessories is available on the Accessercise web shop post-workout | * | * | |||||||||||||
| Social reward | Incentivisation | Once user’s complete workouts they are praised with a ‘great job’ message | * | * | |||||||||||||
| Restructuring the physical environment | Enablement, environmental restructuring | Users on Accessercise are allowed to change the physical environment by having the option to participate at home, outside or at the gym | * | * | * | * | * | ||||||||||
| Body changes | Enablement | All Accessercise users are encouraged to undertake strength training exercises as part of the intervention | * | * | * | * | * | ||||||||||
*, indicate that the behaviour change technique is included within the app.
The Accessercise app included BCTs associated with education by offering feedback on behaviour, training through instructional videos, and modelling by demonstrating the behaviour. To build on these functions, the Accessercise app developers could include progressive (or graded) videos of the behaviour, incorporating differentiation from easy to more complex exercises so that users can be challenged throughout their workouts if needed, which may result in longer-term adherence. Additionally, as some users may be inexperienced with physical activity, online consultation and live chat services may help educate some users with the plethora of queries regarding different exercises and workout plans. Regarding persuasion, incentivisation, coercion and enablement, Accessercise aims to develop the ability to problem solve and make decisions related to physical activity. These functions are encouraged by regular goal setting (i.e., SMART targets), self-monitoring strategies, and offering weekly and monthly diaries to monitor the progression of physical activity. The app developers could develop these functions further by pairing them with, for example, tracking monitors to view heart rate, time spent exercising, and distance covered to help users monitor their performance over time.
Step 8: mode of delivery
In this eighth and final step, the most applicable mode(s) of delivery for the chosen BCTs are identified using the APEASE criteria (Table S9).
Most delivery modes were not suitable on the grounds of high costs for development and service provision (i.e., affordability). The mode of delivery that was viewed as most suitable was digital media (e.g., Internet or mobile phone app) since this mode would be low cost, allow for the identified BCTs to be effectively delivered (i.e., practicability), and would be both acceptable to and reach the intended recipients (i.e., equity) of the intervention.
Behaviour change potential
The app behaviour change scale (ABACUS) (86) was used to review the behaviour change potential of the Accessercise app. The ABACUS comprises 21 items that examine potential behaviour change in relation to knowledge and information (five items), goals and planning (three items), feedback and monitoring (seven items), and actions (six items) (87). A total score out of 21 is calculated by summing each item score, with a higher score indicative of greater confidence in behaviour change potential. Accessercise was independently reviewed and scored by JAH and DWM, with any disagreements discussed amongst all authors.
Overall, Accessercise includes 16 of the 21 items on the scale, indicating a high number of BCTs embedded in the app and suggesting ‘strong confidence’ in behaviour change potential. See Table 2 for examples of app features linked to each item on the scale. To potentially improve behaviour change potential, the app could incorporate the following “missing” items: (I) including information on the consequences of continuing and/or discontinuing behaviour, (II) providing users reminders and prompts, encouraging positive habit formation, (III) allowing opportunities to export data onto social media channels and asking users about their willingness to change behaviour, (IV) incorporating graded tasks, and (V) notifying users via a text message on a selected day/time that they are likely to exercise.
Table 2
| Scales: item number and question | Definition | Included in app? | Example from Accessercise app |
|---|---|---|---|
| Knowledge and information | |||
| Does the app have the ability to customise and personalise some features? | Elements of the app can be personalised through specific tools or functions that are specific to the individual using the app | Yes | Users select their impairment type and can create a workout plan based on their impairment and exercise needs |
| Was the app created with expertise and/or does the app provide information that is consistent with national guidelines? | This would be found in the about section or generally in the app | Yes | Two sporting world champions founded Accessercise; an advisory group with physical disabilities helped throughout the development phase |
| Does the app ask for baseline information? | This includes BMI, weight, smoking rate, exercise, or drinking behaviours | Yes | When signing up for Accessercise, users are asked about their impairment, current exercise habits and whether they require assistance |
| Does the app provide instruction on how to perform the behaviour | This app is clear in telling the person how to perform a behaviour or preparatory behaviours, either verbally, through video, or in written form | Yes | Videos and written instructions are provided to lead users through each exercise |
| Does the app provide information about the consequences of continuing and/or discontinuing behaviour? | The app gives the user information about the consequences of behaviours in general, this includes information about the relationship between the behaviour and its possible or likely consequences in the general case. This information can be general or personalised | No | N/A |
| Goals and planning | |||
| Does the app ask for willingness for behaviour change? | Is there a feature during setup where you describe how ready you are for behaviour change? | No | N/A |
| Does the app allow for the setting of goals? | The person is encouraged to make a behavioural resolution. The person is encouraged to set a general goal that can be achieved by behavioural means | Yes | Users can set their own goals when designing their workouts |
| Does the app have the ability to review goals, update and change when necessary? | Involves a review or analysis of the extent to which previously set behavioural goals (regardless of short or long) were achieved | Yes | Users can revise or adjust their goals by editing the selected workout on the app |
| Feedback and monitoring | |||
| Does the app give the user the ability to quickly and easily understand the difference between current action and future goals? | Allows user to see how they are tracking against a goal and to see the difference between what they want to do and what they are currently doing | Yes | There is a calendar function where users can see what their goal is and update as necessary |
| Does the app have the ability to allow the user to easily self-monitor behaviour? | The app allows for a regular monitoring of the activity | Yes | Users can set their own goals (i.e., build muscle, get toned) when designing their workouts |
| Does the app have the ability to share behaviours with others (including social media or forums) and/or allow for social comparison? | The app allows the person to share his or her behaviours on social media or in forums. This could also include a buddy system or leaderboard | Yes | Users can share their progress with other users on the social hub by commenting on their workout and adding an emoji based on their mood |
| Does the app have the ability to give the user feedback—either from a person or automatically? | The app is able to provide the person with feedback, comments, or data about their own recorded behaviour. This might be automatic or could be personal | Yes | Users can review feedback after each workout, which can be viewed on the calendar |
| Does the app have the ability to export data from app? | The app allows for the export of information and progress to an external user | No | N/A |
| Does the app provide a material or social reward or incentive? | App provides rewards for attempts at achieving a behavioural goal | Yes | The app allows users to purchase discounted sportswear and accessories from the online store |
| Does the app provide general encouragement? | The app provides general encouragement and positive reinforcement on actions leading to the goal | Yes | Users are praised with positive feedback such as ‘good job!’ on completion of workouts |
| Actions | |||
| Does the app have reminders and/or prompts or cues for activity? | The app prompts the user to engage in the activity. The app has the ability to give notifications or reminders to cue the behaviour | No | N/A |
| Does the app encourage positive habit formation? | The app prompts explicit rehearsal and repetition of the behaviour—not just tracking or logging | No | N/A |
| Does the app allow or encourage for practice or rehearsal, in addition to daily activities? | App does not have a lock on activities or a number that you cannot exceed daily | Yes | Users can undertake as many exercises/workouts as they deem necessary daily |
| Does the app provide opportunity to plan for barriers? | The app encourages the person to think about potential barriers and identify ways of overcoming them | Yes | Users can check the accessibility of local gyms using the ‘explore’ function |
| Does the app assist with or suggest restructuring the physical or social environment? | The app prompts the person to alter the environment in ways that it is more supportive of the target behaviour | Yes | The app encourages the personal to alter the environment through various environmental barriers (cost, transport, time) |
| Does the app assist with distraction or avoidance? | The app gives suggestions and advice on how the person can avoid situations or distract themselves when trying to reach their goal | Yes | Users are provided with the forum (social) function where they can communicate with other users |
Total score (out of 21): 16. BMI, body mass index; N/A, not applicable.
Discussion
The aim of the current study was to assess the behaviour change potential of a novel smartphone fitness app, Accessercise. Overall, our analysis suggests that an mHealth intervention may be a practical approach for adults with SCI, offering users the capability, opportunity, and motivation to undertake physical activity and reduce sedentary behaviours. Furthermore, Accessercise targets all functions of the COM-B model, including goal setting/action planning (capability), self-monitoring/feedback (opportunity) and reviewing goals (motivation). As a result, Accessercise has high behaviour change potential. This is further highlighted by our assessment using the ABACUS, devised-by McKay and colleagues (86). Critically, Lawrason and colleagues (31) stress that behaviour change interventions need to target one or more of these core components (i.e., capability, opportunity, motivation) to change behaviour.
The findings of the current study are promising, given that Accessercise was not initially developed using an underpinning theory. This is perhaps unsurprising, given that very few physical activity mHealth interventions are theory based (88), making it difficult to determine the specific intervention components that may be most effective in changing behaviour. Nevertheless, the method of “retrofitting” Accessercise to the BCW framework is appropriate, as it can help to identify the functions (or BCTs) that have been included in the app that can facilitate physical activity behaviour change. Therefore, the current study could be used by other researchers and/or app developers seeking to employ similar methods in the design and evaluation of future mHealth interventions, including those that aim to improve physical activity in adults with SCI.
Accessercise includes relevant BCTs that could help change behaviours, helping users with SCI to meet recommended physical activity guidelines and to overcome barriers [e.g., increased costs to participate, limited time/transportation (6,7,89)]. However, there is also a need to ensure that the app can reach disadvantaged groups and communities, including those with disabilities. Due to Accessercise being a novel mHealth app, many users may miss the chance to be signposted or even recognise what Accessercise can offer. For example, people with SCI may find using a smartphone challenging to use if they lack sufficient digital competence and/or access to a smartphone or the internet (90). Indeed, in the UK, 45% of people with disabilities regularly use a smartphone compared to 75% of people without disabilities (91). People with disabilities in the UK are also less likely than those without a disability to own computers, including a PC, laptop, and tablet (64% vs. 85%, respectively) (91). Future researchers could identify strategies to improve access to mHealth technologies. One way is by reducing social exclusion, marginalisation, and disability stigma through mainstreaming disability (92). When using mHealth and other assistive technologies, society often stigmatises users, making them feel vulnerable, self-conscious, and embarrassed. Knowledge about such issues could even support designers, developers, and people with disabilities, including those with SCI, in designing effective interventions with low product abandonment.
Limitations
We acknowledge several limitations concerning the current research. First, the development, evaluation, and implementation of mHealth apps can be time-consuming. As a result, technology and target group interests can quickly change and become outdated. In addition, the functionality, and features of Accessercise continue to expand, making it difficult to decide when best to evaluate the app’s behaviour change potential, as this may change over time. Second, even though the BCW can assist with designing interventions, it lacks a formal guide in translating BCTs. Consequently, translating BCTs into app features relies heavily on the expertise and creativity of the research team and/or app developers. Third, coding the BCTs from the app and completing the specified worksheets was time-consuming and labour-intensive. The time-and-resource-intensive nature of the BCW procedure could make it unfeasible for specific problems, organisations, and/or circumstances.
Conclusions
The current study reveals the value of using the BCW to systematically identify the potential mechanisms of action for improving physical activity levels in adults with SCI, as well as the potential of a novel smartphone fitness app, Accessercise, to change behaviour. Consequently, the effectiveness of Accessercise to facilitate the desired behaviour change should be assessed, such as via a randomised control trial. Such high-quality evidence would provide the foundation that could guide decisions concerning how to improve physical activity, as well as health more generally, in adults with SCI.
Acknowledgments
The authors would like to thank the founders of Accessercise, Sam Breary, Ali Jawad, and Yulia Kyrpa, for allowing the research team full access to the Accessercise application.
Funding: None.
Footnote
Data Sharing Statement: Available at https://mhealth.amegroups.com/article/view/10.21037/mhealth-22-52/dss
Peer Review File: Available at https://mhealth.amegroups.com/article/view/10.21037/mhealth-22-52/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://mhealth.amegroups.com/article/view/10.21037/mhealth-22-52/coif) and report that Loughborough University and Accessercise Ltd. have a formal Research Collaboration Agreement, commencement date, 2nd August 2022.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). As the study did not involve human participants due to the nature of the research design (i.e., secondary data), ethical approval was not required.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Qi Y, Xie H, Shang Y, et al. Effects of 16-Form Wheelchair Tai Chi on the Autonomic Nervous System among Patients with Spinal Cord Injury. Evid Based Complement Alternat Med 2020;2020:6626603. [Crossref] [PubMed]
- Peterson MD, Berri M, Lin P, et al. Cardiovascular and metabolic morbidity following spinal cord injury. Spine J 2021;21:1520-7. [Crossref] [PubMed]
- Martin Ginis KA, van der Scheer JW, Latimer-Cheung AE, et al. Evidence-based scientific exercise guidelines for adults with spinal cord injury: an update and a new guideline. Spinal Cord 2018;56:308-21. [Crossref] [PubMed]
- Adriaansen JJ, Ruijs LE, van Koppenhagen CF, et al. Secondary health conditions and quality of life in persons living with spinal cord injury for at least ten years. J Rehabil Med 2016;48:853-60. [Crossref] [PubMed]
- Marco-Ahulló A, Montesinos-Magraner L, González LM, et al. Impact of COVID-19 on the self-reported physical activity of people with complete thoracic spinal cord injury full-time manual wheelchair users. J Spinal Cord Med 2022;45:755-9. [Crossref] [PubMed]
- Martin Ginis KA, Ma JK, Latimer-Cheung AE, et al. A systematic review of review articles addressing factors related to physical activity participation among children and adults with physical disabilities. Health Psychol Rev 2016;10:478-94. [Crossref] [PubMed]
- Lai BW, Rimmer JH, Yates A, et al. Critical factors influencing the decision to enroll in a physical activity intervention among a predominant group of adults with spinal cord injury: a grounded theory study. Spinal Cord 2021;59:17-25. [Crossref] [PubMed]
- Eerden S, Dekker R, Hettinga FJ. Maximal and submaximal aerobic tests for wheelchair-dependent persons with spinal cord injury: a systematic review to summarize and identify useful applications for clinical rehabilitation. Disabil Rehabil 2018;40:497-521. [Crossref] [PubMed]
- Bates LC, Conners R, Zieff G, et al. Physical activity and sedentary behavior in people with spinal cord injury: Mitigation strategies during COVID-19 on behalf of ACSM-EIM and HL-PIVOT. Disabil Health J 2022;15:101177. [Crossref] [PubMed]
- Mehta S, Ahrens J, Abu-Jurji Z, et al. Feasibility of a virtual service delivery model to support physical activity engagement during the COVID-19 pandemic for those with spinal cord injury. J Spinal Cord Med 2021;44:S256-65. [Crossref] [PubMed]
- Piatt JA, Nagata S, Zahl M, et al. Problematic secondary health conditions among adults with spinal cord injury and its impact on social participation and daily life. J Spinal Cord Med 2016;39:693-8. [Crossref] [PubMed]
- Westgren N, Levi R. Quality of life and traumatic spinal cord injury. Arch Phys Med Rehabil 1998;79:1433-9. [Crossref] [PubMed]
- Williams TL, Smith B, Papathomas A. Physical activity promotion for people with spinal cord injury: physiotherapists' beliefs and actions. Disabil Rehabil 2018;40:52-61. [Crossref] [PubMed]
- Hicks AL. Locomotor training in people with spinal cord injury: is this exercise? Spinal Cord 2021;59:9-16. [Crossref] [PubMed]
- van der Scheer JW, Martin Ginis KA, Ditor DS, et al. Effects of exercise on fitness and health of adults with spinal cord injury: A systematic review. Neurology 2017;89:736-45. [Crossref] [PubMed]
- Sliwinski MM, Akselrad G, Alla V, et al. Community exercise programing and its potential influence on quality of life and functional reach for individuals with spinal cord injury. J Spinal Cord Med 2020;43:358-63. [Crossref] [PubMed]
- Ma JK, Ginis KA. A meta-analysis of physical activity interventions in people with physical disabilities: content, characteristics, and effects on behaviour. Psychol Sport Exerc 2018;37:262-73. [Crossref]
- Nooijen CF, Stam HJ, Schoenmakers I, et al. Working mechanisms of a behavioural intervention promoting physical activity in persons with subacute spinal cord injury. J Rehabil Med 2016;48:583-8. [Crossref] [PubMed]
- Ma JK, West CR. Martin Ginis KA. The Effects of a Patient and Provider Co-Developed, Behavioral Physical Activity Intervention on Physical Activity, Psychosocial Predictors, and Fitness in Individuals with Spinal Cord Injury: A Randomized Controlled Trial. Sports Med 2019;49:1117-31. [Crossref] [PubMed]
- Latimer AE, Ginis KA, Arbour KP. The efficacy of an implementation intention intervention for promoting physical activity among individuals with spinal cord injury: A randomized controlled trial. Rehabil Psychol 2006;51:273. [Crossref]
- Jiménez-Pavón D, Carbonell-Baeza A, Lavie CJ. Physical exercise as therapy to fight against the mental and physical consequences of COVID-19 quarantine: Special focus in older people. Prog Cardiovasc Dis 2020;63:386-8. [Crossref] [PubMed]
- Lippi G, Henry BM, Sanchis-Gomar F. Physical inactivity and cardiovascular disease at the time of coronavirus disease 2019 (COVID-19). Eur J Prev Cardiol 2020;27:906-8. [Crossref] [PubMed]
- Jee H. Review of researches on smartphone applications for physical activity promotion in healthy adults. J Exerc Rehabil 2017;13:3-11. [Crossref] [PubMed]
- Lai B, Rimmer J, Barstow B, et al. Teleexercise for Persons With Spinal Cord Injury: A Mixed-Methods Feasibility Case Series. JMIR Rehabil Assist Technol 2016;3:e8. [Crossref] [PubMed]
- Chemtob K, Rocchi M, Arbour-Nicitopoulos K, et al. Using tele-health to enhance motivation, leisure time physical activity, and quality of life in adults with spinal cord injury: A self-determination theory-based pilot randomized control trial. Psychology of Sport and Exercise 2019;42:243-52. [Crossref]
- Costa RRG, Dorneles JR, Veloso JH, et al. Synchronous and asynchronous tele-exercise during the coronavirus disease 2019 pandemic: Comparisons of implementation and training load in individuals with spinal cord injury. J Telemed Telecare 2021; Epub ahead of print. [Crossref] [PubMed]
- Marco-Ahulló A, Montesinos-Magraner L, González LM, et al. Encouraging People with Spinal Cord Injury to Take Part in Physical Activity in the COVID-19 Epidemic through the mHealth ParaSportAPP. Healthcare (Basel) 2022;10:1069. [Crossref] [PubMed]
- Venugopal LS, Musbahi A, Shanmugam V, et al. A systematic review of smartphone apps for gastro-oesophageal reflux disease: the need for regulation and medical professional involvement. Mhealth 2021;7:56. [Crossref] [PubMed]
- Hoevenaars D, Holla JFM, Te Loo L, et al. Mobile App (WHEELS) to Promote a Healthy Lifestyle in Wheelchair Users With Spinal Cord Injury or Lower Limb Amputation: Usability and Feasibility Study. JMIR Form Res 2021;5:e24909. [Crossref] [PubMed]
- Liu T, Xie S, Wang Y, et al. Effects of App-Based Transitional Care on the Self-Efficacy and Quality of Life of Patients With Spinal Cord Injury in China: Randomized Controlled Trial. JMIR Mhealth Uhealth 2021;9:e22960. [Crossref] [PubMed]
- Lawrason SVC, Brown-Ganzert L, Campeau L, et al. mHealth Physical Activity Intervention for Individuals With Spinal Cord Injury: Planning and Development Processes. JMIR Form Res 2022;6:e34303. [Crossref] [PubMed]
- Canadian Society for Psychomotor Learning and Sport Psychology (SCAPPS) Conference. 2022 Oct 13-15. Montréal, Québec: Canada.
- Collins LM, Baker TB, Mermelstein RJ, et al. The multiphase optimization strategy for engineering effective tobacco use interventions. Ann Behav Med 2011;41:208-26. [Crossref] [PubMed]
- Craig P, Dieppe P, Macintyre S, et al. Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ 2008;337:a1655. [Crossref] [PubMed]
- NICE. Behaviour change: digital and mobile health interventions. 2020. Available online: https://www.nice.co.uk/guidance/ng183
- Panter-Brick C, Clarke SE, Lomas H, et al. Culturally compelling strategies for behaviour change: a social ecology model and case study in malaria prevention. Soc Sci Med 2006;62:2810-25. [Crossref] [PubMed]
- Kwasnicka D, Dombrowski SU, White M, et al. Theoretical explanations for maintenance of behaviour change: a systematic review of behaviour theories. Health Psychol Rev 2016;10:277-96. [Crossref] [PubMed]
- Briscoe C, Aboud F. Behaviour change communication targeting four health behaviours in developing countries: a review of change techniques. Soc Sci Med 2012;75:612-21. [Crossref] [PubMed]
- Ouellette JA, Wood W. Habit and intention in everyday life: The multiple processes by which past behavior predicts future behavior. Psychol Bull 1998;124:54. [Crossref]
- Aboud FE, Singla DR. Challenges to changing health behaviours in developing countries: a critical overview. Soc Sci Med 2012;75:589-94. [Crossref] [PubMed]
- Agarwal A, Gupta D. Communication implications: Maternal health concerns of domestic women workers in urban clusters. CRITIQUE: An International Interdisciplinary Research Journal 2015;1:2454-19.
- Cowan LT, Van Wagenen SA, Brown BA, et al. Apps of steel: are exercise apps providing consumers with realistic expectations? A content analysis of exercise apps for presence of behavior change theory. Health Educ Behav 2013;40:133-9. [Crossref] [PubMed]
- Oinas-Kukkonen H, Harjumaa M. Persuasive systems design: Key issues, process model, and system features. Commun Assoc Inf Syst. 2009;24:28. [Crossref]
- Rosenstock IM. Why people use health services. Milbank Mem Fund Q 1966;44:94-127. [Crossref] [PubMed]
- Janz NK, Becker MH. The Health Belief Model: a decade later. Health Educ Q 1984;11:1-47. [Crossref] [PubMed]
- Prochaska, JO, DiClemente, CC. The transtheoretical approach: Crossing the traditional boundaries of therapy. Florence, KY, USA: Brooks/Cole, 1984.
- Prochaska, JO, DiClemente CC, Norcross JC. Handbook of eclectic psychotherapy. New York: Brunnel-Mazel, 1986.
- Prochaska, JO, DiClemente CC. The transtheoretical approach. New York: Basic Books, 1986.
- Bandura A. Self-efficacy toward a unifying theory of behavioral change. Psychol Rev 1977;84:191-215. [Crossref] [PubMed]
- Bandura A. Self-efficacy mechanism in human agency. Am Psychol 1982;37:122. [Crossref]
- Bandura A. Social foundations of thought and action: A social cognitive theory. Upper Saddle River, NJ, USA: Pearson, 1985.
- Ajzen I, Fishbein M. Understanding attitudes and predicting social behaviour. Old Tappan, NJ, USA: Prentice Hall, 1980.
- Ajzen I. Attitudes, personality, and behavior. Milton Keynes: Open University Press, 1988.
- Ajzen I. The theory of planned behavior. Organizational Behavior and Human Decision Processes 1991;50:179-211. [Crossref]
- Coulson NS, Ferguson MA, Henshaw H, et al. Applying theories of health behaviour and change to hearing health research: Time for a new approach. Int J Audiol 2016;55:S99-S104. [Crossref] [PubMed]
- Gallant AJ, Flowers P, Deakin K, et al. Barriers and enablers to influenza vaccination uptake in adults with chronic respiratory conditions: applying the behaviour change wheel to specify multi-levelled tailored intervention content. Psychol Health 2023;38:147-66. [Crossref] [PubMed]
- Kok G, Schaalma H, Ruiter RA, et al. Intervention mapping: protocol for applying health psychology theory to prevention programmes. J Health Psychol 2004;9:85-98. [Crossref] [PubMed]
- Brug J, Oenema A, Ferreira I. Theory, evidence and Intervention Mapping to improve behavior nutrition and physical activity interventions. Int J Behav Nutr Phys Act 2005;2:2. [Crossref] [PubMed]
- Michie S, van Stralen MM, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci 2011;6:42. [Crossref] [PubMed]
- Michie S, Atkins L, West R. The behaviour change wheel. A guide to designing interventions. Britain: Silverback Publishing, 2014.
- Kwok BC, Wong WP, Remedios L. Improving centre-based group exercise participation of older adults using the behaviour change wheel. BMJ Open Qual 2021;10:e001078. [Crossref] [PubMed]
- Carroll GA, Groarke JM. The Importance of the Social Sciences in Reducing Tail Biting Prevalence in Pigs. Animals (Basel) 2019;9:591. [Crossref] [PubMed]
- Edwardson CL, Yates T, Biddle SJH, et al. Effectiveness of the Stand More AT (SMArT) Work intervention: cluster randomised controlled trial. BMJ 2018;363:k3870. [Crossref] [PubMed]
- Gould GS, Bar-Zeev Y, Bovill M, et al. Designing an implementation intervention with the Behaviour Change Wheel for health provider smoking cessation care for Australian Indigenous pregnant women. Implement Sci 2017;12:114. [Crossref] [PubMed]
- Tada Y, Jo SJ, Huang YH, et al. Uncovering the unmet needs among psoriasis patients in the Asia-Pacific region. J Dermatol 2021;48:1665-74. [Crossref] [PubMed]
- Walker RAJ, Colclough M, Limbert C, et al. Perceived barriers to, and benefits of physical activity among British military veterans that are wounded, injured, and/or sick: a Behaviour Change Wheel perspective. Disabil Rehabil 2022;44:901-9. [Crossref] [PubMed]
- Vasiliou VS, Dockray S, Dick S, et al. Reducing drug-use harms among higher education students: MyUSE contextual-behaviour change digital intervention development using the Behaviour Change Wheel. Harm Reduct J 2021;18:56. [Crossref] [PubMed]
- Koripalli M, Giruparajah M, Laur C, et al. Selecting an intervention to prevent ketoacidosis at diabetes diagnosis in children using a behavior change framework. Pediatr Diabetes 2022;23:406-10. [Crossref] [PubMed]
- Fahim C, Acai A, McConnell MM, et al. Use of the theoretical domains framework and behaviour change wheel to develop a novel intervention to improve the quality of multidisciplinary cancer conference decision-making. BMC Health Serv Res 2020;20:578. [Crossref] [PubMed]
- Greene C, Wilson J. The use of behaviour change theory for infection prevention and control practices in healthcare settings: A scoping review. J Infect Prev 2022;23:108-17. [Crossref] [PubMed]
- Handley MA, Harleman E, Gonzalez-Mendez E, et al. Applying the COM-B model to creation of an IT-enabled health coaching and resource linkage program for low-income Latina moms with recent gestational diabetes: the STAR MAMA program. Implement Sci 2016;11:73. [Crossref] [PubMed]
- Robb KA. The integrated screening action model (I-SAM): A theory-based approach to inform intervention development. Prev Med Rep 2021;23:101427. [Crossref] [PubMed]
- van Leeuwen LM, Pronk M, Merkus P, et al. Developing an intervention to implement an ICF-based e-intake tool in clinical otology and audiology practice. Int J Audiol 2020;59:282-300. [Crossref] [PubMed]
- Watkins K, Seubert L, Schneider CR, et al. Post hoc evaluation of a common-sense intervention for asthma management in community pharmacy. BMJ Open 2016;6:e012897. [Crossref] [PubMed]
- Ekberg K, Schuetz S, Timmer B, et al. Identifying barriers and facilitators to implementing family-centred care in adult audiology practices: a COM-B interview study exploring staff perspectives. Int J Audiol 2020;59:464-74. [Crossref] [PubMed]
- Murphy ME, Byrne M, Zarabzadeh A, et al. Development of a complex intervention to promote appropriate prescribing and medication intensification in poorly controlled type 2 diabetes mellitus in Irish general practice. Implement Sci 2017;12:115. [Crossref] [PubMed]
- Ribaut J, Leppla L, Teynor A, et al. Theory-driven development of a medication adherence intervention delivered by eHealth and transplant team in allogeneic stem cell transplantation: the SMILe implementation science project. BMC Health Serv Res 2020;20:827. [Crossref] [PubMed]
- McQuinn S, Belton S, Staines A, et al. Co-design of a school-based physical activity intervention for adolescent females in a disadvantaged community: insights from the Girls Active Project (GAP). BMC Public Health 2022;22:615. [Crossref] [PubMed]
- Vermaak C, Ferreira S, Terblanche E, et al. Physical activity promotion in persons with spinal cord injuries: Barriers and facilitators in low-resource communities. Afr J Disabil 2022;11:988. [Crossref] [PubMed]
- Hisham H, Rosley H, Manaf H, et al. Barriers and Facilitators to Physical Activity and Exercise Among Individuals with Spinal Cord Injury: A Systematic review. M J Med Health Sci 2022;18:2636-9346.
- Mcleod JC, Diana H, Hicks AL. Sprint interval training versus moderate-intensity continuous training during inpatient rehabilitation after spinal cord injury: a randomized trial. Spinal Cord 2020;58:106-15. [Crossref] [PubMed]
- Mashola MK, Mothabeng DJ. Associations between health behaviour, secondary health conditions and quality of life in people with spinal cord injury. Afr J Disabil 2019;8:463. [Crossref] [PubMed]
- Hwang EJ, Groves MD, Sanchez JN, et al. Barriers to Leisure-Time Physical Activities in Individuals with Spinal Cord Injury. Occup Ther Health Care 2016;30:215-30. [Crossref] [PubMed]
- Kolodko J, Schmidtke KA, Read D, et al. #LetsUnlitterUK: A demonstration and evaluation of the Behavior Change Wheel methodology. PLoS One 2021;16:e0259747. [Crossref] [PubMed]
- Clarke A, Paraskeva N, White P, et al. PEGASUS: the Design of an Intervention to Facilitate Shared Decision-making in Breast Reconstruction. J Cancer Educ 2021;36:508-18. [Crossref] [PubMed]
- McKay FH, Slykerman S, Dunn M. The App Behavior Change Scale: Creation of a Scale to Assess the Potential of Apps to Promote Behavior Change. JMIR Mhealth Uhealth 2019;7:e11130. [Crossref] [PubMed]
- AlSlaity A, Suruliraj B, Oyebode O, et al. Mobile Applications for Health and Wellness: A Systematic Review. Proc ACM Hum Comput Interact 2022;6:1-29. [Crossref]
- Rigot SK, Worobey LA, Boninger ML, et al. Changes in Internet Use Over Time Among Individuals with Traumatic Spinal Cord Injury. Arch Phys Med Rehabil 2022;103:832-839.e2. [Crossref] [PubMed]
- MacPherson MM, Cranston KD, Locke SR, et al. Using the behavior change wheel to develop text messages to promote diet and physical activity adherence following a diabetes prevention program. Transl Behav Med 2021;11:1585-95. [Crossref] [PubMed]
- Mageshwari S, Kuppusamy KS. Multimodal authentication approach for visually impaired in smartphone platforms. In: 2016 10th International Conference on Intelligent Systems and Control (ISCO). IEEE; 2016.
- Ofcom. Disabled users access to and use of communication devices and services research summary: All disabled people. 2019. Available online: https://www.ofcom.org.uk/__data/assets/pdf_file/0023/132962/Research-summary-all-disabilities.pdf
- Holloway C. Disability interaction (dix) a manifesto. Interactions 2019;26:44-9. [Crossref]
Cite this article as: Haley JA, Rhind DJA, Maidment DW. Applying the behaviour change wheel to assess the theoretical underpinning of a novel smartphone application to increase physical activity in adults with spinal cord injuries. mHealth 2023;9:10.


