This article has an erratum available at: http://dx.doi.org/10.21037/mhealth-2023-01 the article has been update on 2023-03-14 at here.
Effectiveness of mHealth intervention on safe abortion knowledge and perceived barriers to safe abortion services among female sex workers in Vietnam
Highlight box
Key findings
• iConnect is the first integrated mobile app-based intervention to address the high risk of unsafe abortions among female sex workers (FSWs) in Vietnam.
• The intervention among FSWs showed significant improvements in the knowledge and behaviors related to safe abortion as well as a reduction in perceived barriers for access to safe abortion services.
What is known and what is new?
• mHealth-based interventions have been used to address health problems in diverse populations; however, iConnect is the first mHealth study to address the changes in FSWs’ knowledge and behaviors related to safe abortion information and services.
What is the implication, and what should change now?
• This study indicates that mHealth intervention is a feasible and effective approach for improving FSWs’ knowledge about safe abortion and access to available safe abortion services. Future research is needed to establish the efficacy of the intervention for scaling up in Vietnam and elsewhere.
Introduction
Female sex workers (FSWs) experience physical, sexual and emotional violence at work (1-4) and are at high risk of human immunodeficiency virus (HIV), sexually transmitted infections (STIs) and unintended pregnancy (5,6). While risks of HIV and other STIs have long been recognized (7,8), unintended pregnancy and unsafe abortion have received less attention among FSWs (9). Abortion is common in low- and middle-income countries (LMICs) and the majority of abortions was resulted from unintended pregnancies (9). FSWs experience higher risks of unintended pregnancy due to a high frequency of intercourses and a high number of sexual partners (10). A systematic review in LMICs found that unintended pregnancy incidence among FSWs range from 7.2 to 59.6 per 100 person-years (11). Studies in Asia documented that prevalence of self-reported abortion among FSWs in the past one-year ranges from 15.5% in Bangladesh (12), 26% in Laos to 28% in Cambodia (13). In particularly, as high as 44% of FSWs reported ever had an abortion in China (14).
Given higher risks for unintended pregnancies and abortion, FSWs need comprehensive and accessible sexual and reproductive health (SRH) services including antennal care, safe abortion and post abortion care. A study in India and Kenya found that 93.7% of FSWs in India visited a health facility for a termination of an unwanted pregnancy (15). In the same study, 34.4% of FSWs in Kenya sought medical care after forced sex (15). However, FSWs do not have access to adequate SRH services and safe abortion in many regions in LMICs, especially where abortion is illegal. A systematic review of SRH programs for FSWs in Africa found a limited scope of SRH services in both the private and public sectors. While most of the 54 programs reviewed addressed HIV/STIs, no program offered termination of pregnancy services and post abortion care (16). Limited access to contraceptives (14,17) and sexual violence (1-3) can result in unintended pregnancy and abortion, making access to antennal care, safe abortion and post-abortion care an essential SRH need for FSWs. Many FSWs may not be able to use commonly available contraceptive methods such as condoms because they have limited autonomy to negotiate with male clients (17-20). However, there have been limited effective interventions to address unintended pregnancies and unsafe abortion as part of SRH services for FSWs in LMICs.
In Vietnam, abortion is legal up to 22 gestational weeks. With about 40% of all pregnancies ending in abortion each year (21), Vietnam has the second-highest abortion rate in the world and ranks first in Asia (22,23). The abortion rate in Vietnam is equal to 2.5 abortions per woman per lifetime, indicating a high frequency of repeat abortion (24). Despite commercial sex work is illegal and highly stigmatized in Vietnam (25), FSWs constitute a growing population with an estimated 300,000 FSWs in the country (26). Vietnamese FSWs generally live and work in unsafe environments with limited access to healthcare and social services. Sexual exploitation and gender-based violence are common among those women (27). Although safe abortion services are legally available, the illegality of sex work, stigma against sex work, lack of service information, as well as perceived discrimination from healthcare service providers severely hinder FSW’s access to safe abortion services (27-29). Previous research and interventions in Vietnam have primarily focused on prevention and treatment of HIV/STIs, few studies have addressed SRH needs, especially contraceptive use and unsafe abortions among FSWs.
Mobile health (mHealth) is characterized as the use of mobile technologies to improve access to health information and health service delivery. Over the past decade, with the widespread use of mobile and wireless technologies and the rapid expansion of smartphone ownership, mHealth has been increasingly used to deliver health interventions and promotions in LMICs (30-33). mHealth is recognized as a promising and cost-effective strategy to reach and serve stigmatized and hard-to-reach populations including FSWs (32,33). The use of mHealth may help overcome most of the socio-cultural barriers and reduce individuals’ discomfort and reticence to disclose risk behaviors and identity to service providers, particularly for marginalized populations (34-36). It can further guide prevention delivery and health decision-making in a confidential, less stigmatizing, and convenient manner (33,37,38). mHealth-based interventions have been used to address health problems in diverse populations such as improving SRH knowledge among young adolescents (33), increasing HIV self-testing among men who have sex with men (34), promoting access to family planning services (35) and increasing anti-retroviral treatment (ART) initiation and adherence among HIV positive FSWs (36). However, there is a paucity of studies on the use of mHealth for promoting SRH and contraception knowledge, preventing unintended pregnancy and improving access to safe abortion among FSWs (37).
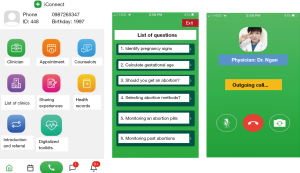
In recent years, Vietnam has experienced the exponential growth of widespread access to high-speed Internet and mobile phones, particularly smartphones. In 2021, Vietnam had 61.3 million smartphone users which was among the top 10 countries with the highest number of smartphone users globally (38) and had one of the highest numbers of smartphone users in Asia (39). On average, a Vietnamese person spent approximately 6.5 hours using the Internet per day in 2021 (39). Funded by Grand Challenges Canada, between December 2019 and December 2021, Center for Promotion of Advancement of Society (CPAS), Vietnam developed and piloted a mobile app, entitled: ‘iConnect’ to promote SRH, contraception knowledge, and to address unsafe abortion among FSWs in Hanoi, Vietnam. iConnect was designed as a virtual platform to enable women to access SRH providers and peer support as an alternative to traditional venue-based approaches. iConnect used interactive short messaging services (SMS) enhanced by tele-counseling to reach and deliver SRH education to FSWs focusing on preventing unwanted pregnancy, safe abortion, and stigma reduction, and connecting women to safe abortion services. The app also contains digital counseling tools for clinic providers to assess medical eligibility of abortion seekers, provide professional advice and schedule clinic visits. If found to be effective, the use of mHealth for safe abortion could be scaled up to complement and enhance the existing SRH services for FSWs in Vietnam and other LMICs.
The primary purpose of this paper is to (I) examine prevalence of unwanted pregnancy and abortion among FSWs, and (II) evaluate the feasibility and effectiveness of iConnect intervention through changes in knowledge and behaviors on safe abortion as well as changes in perceived barriers to safe abortion services among FSWs in Hanoi, Vietnam.
Methods
Study design and setting
A quasi-experimental, single group pretest-posttest study was conducted among 251 FSWs in Hanoi, Vietnam. Hanoi, the capital of Vietnam, is the second largest city in Vietnam with an estimated 2,000 FSWs (40). FSWs eligible for participation in the intervention included: (I) self-identifying as women; (II) at least 18 years old; (III) reporting having unprotected vaginal or anal sex with a male client in the previous month; (IV) being able to read text messages in Vietnamese; and (V) possessing a personal smart mobile phone with access to wifi.
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Institutional Review Board of the Institute for Social Development Studies, Hanoi, Vietnam. Verbal informed consent in Vietnamese was obtained from all FSWs in the study.
Procedures
We recruited FSWs in 3 rounds started in January 2021 using online based-driven respondent sampling method. Each round consisting of 3 waives started with 2 peer educators-each of whom enrolled 3 FSWs (F0). Each of 6 F0 FSWs were asked to recruit other 18 FSWs (F1), who were then asked to enroll 54 FSWs (F2), who in turn were asked to recruit another 162 FSWs (F3). This sampling strategy was intended to enroll 234 FSWs in each round, totaling 702 FSWs in 3 rounds. Since not all F1, F2, and F3 FSWs were able to recruit all 3 FSWs as planned, the final sample consisted of 512 FSWs who agreed to participate in the study. In each round, the recruitment was completed in 2 weeks, then the enrolled women participated in the intervention for 12 weeks.
Data collection
Questionnaire-based phone interviews were administered to the first 284 out of a total of 512 FSWs at the time of enrollment (pre-test), of whom 251 (88%) were interviewed at 3-month follow-up. Thirty-three (12%) participants were lost to follow up or withdrew. At the follow up interview, participants were asked to complete an individual exit interview regarding their experiences with the intervention and iConnect mobile app (Figure 1).
The intervention
iConnect used an integrated mobile app-based intervention approach that aimed to address unsafe abortion among FSWs in Vietnam. The iConnect app was designed as an interactive platform to enable women to access safe abortion information and connect women with peer support and reliable and quality safe abortion services. The iConnect app was consisted of three interconnected systems (Figure 1). Communication system facilitates communication between women and peer educators and service providers through text messages, remind alerts, chat boxes, video call, clinic visit scheduling, providing convenient access to safe abortion education and counseling. Digitalized toolkit includes interactive decision aid tools and safe abortion manuals to provide knowledge on signs of pregnancy, safe abortion methods, and support decision making related to pregnancy termination and post abortion follow up, prevention and early detection of abortion complications. Client record system serves as an electronic health record that allows service providers to document women’s abortion histories, reasons for clinic visits, actual services usage, clinical summary of diagnoses, counseling, and/or treatment associated with each virtual or in person clinic visit. Three app versions were specifically designed for FSWs, peer educators, and health care service providers (doctors and counselors). The iConnect app facilitated intervention delivery through the following integrated components:
- Automated educational SMS: women who installed the iConnect app received a series of 117 automated educational messages on safe abortion with two messages sent daily. These messages focused on access to safe abortion is a women’s right, common questions and answers on safe abortion, signs and symptoms of pregnancy, access to safe abortion services, abortion methods, home-based post abortion care, consequences of unsafe abortion and contraceptive use after abortion.
- Virtual peer education counseling, support, and referral: a team of 14 peer educators and two peer group leaders were recruited from local FSWs peer networks. Peer educators received a two-day training course delivered by a public health physician. The training provided participants with basic knowledge on safe abortion and safe abortion counseling skills using the iConnect app. Peer educators were also given instructions to recruit women based on the respondent driven sampling method.
- Provision of quality safe abortion counseling and services: two-Hanoi based non-governmental organization (NGO) reproductive health clinics (Light and Marie Stopes) were contracted to provide friendly services to FSWs who were referred to by peer educators. Through the virtual clinic visits by FSWs, service providers actively provided professional and quality safe abortion education and counseling, corrected any misperceptions that FSWs may have, identified FSWs’ informational and service needs, and scheduled clinic appointments to provide quality safe abortion services for those who had unplanned pregnancy.
To encourage utilization of the iConnect app and prevent attrition, peer educators conducted regular virtual counseling and maintained frequent contact with FSWs through multiple mode of interactivities such as chat, phone, and text messages reminders. In addition, the back-end mobile app system was able to monitor the app utilization metrics (e.g., number of active app users, number of frequent users, number of interactions between women and peer educators and service providers). This tracking systems allowed a timely identification of women who uninstalled the app or had limited app utilization so that peer educators would make appropriate interventions (e.g., sending message reminders, making phone calls) to retain women or promote app utilization.
Measurements
Quantitative survey
The primary outcomes were the change in FSWs’ knowledge, attitudes and behaviors on safe abortion and perceived barriers to safe abortion services, measured at baseline and at 3 months following the intervention.
Participants were asked to provide demographic information including age, ethnicity, marital status and education, types of sex work (e.g., street-based or venue-based), and sex work duration, venues where sexual encounter with clients taking place. For histories of pregnancy and abortion, FSWs were asked if they have ever had a pregnancy. If yes, they were further asked how many abortions they had as results of the pregnancy.
- Knowledge of safe abortion methods and post-abortion care: single items assessed participant safe abortion knowledge regarding types of abortion methods, gestational age for medical and surgical abortion, gestational ages for home-based use of medical abortion, abortion complications, and signs and symptoms of infections as a result of abortion complications.
- Knowledge of contraceptive methods: participants were asked to list contraceptive methods they knew of. They were also asked a single question regarding how long after ovulation could someone get pregnant.
- Perceived barriers to safe abortion services: participants were asked to identify which barriers they face when seeking to safe abortion services such as not knowing where to find safe abortion clinics, inconvenient clinic hours, expensive service costs, lack of confidentiality, concerns of stigma and discrimination by service providers, etc.
- Knowledge on clinic facilities that provide abortion services: participants were asked to identify which facilities could provide safe abortion services (e.g., private gynecological clinics, gynecological hospitals, commune/ward health centers).
Post intervention qualitative interviews
After receiving the intervention, one focus group discussion (FGD) with six FSWs, one FGD with six peer educators and five in-depth interviews (IDIs) with FSWs were conducted by an experienced social scientist researcher. The FGD and IDI gathered information related to participants’ experience in using the ‘iConnect’ app, the support they received from peer educators, and services they received from the clinics.
Data analysis and statistical analysis
Quantitative data
Descriptive analysis was conducted to describe baseline demographic characteristics (i.e., age, education), and occupational characteristics (i.e., sex work duration, venue where sexual encounter was taking place and histories of pregnancy and abortion). Differences in key outcomes (i.e., knowledge and attitudes about safe abortion, knowledge on contraceptives and pregnancy) between baseline and 3-month follow-up were evaluated using non-parametric Wilcoxon signed rank test and McNemar’s tests. Statistical significance was set at P<0.05.
Qualitative data
FGD and IDI recordings were transcribed verbatim and entered into ATLAS.ti (41) for storage and analysis. Code categories were developed based on both the project research questions and other new issues that emerged from the interview text, creating complementarity, allowing for qualitative explanation of the quantitative data (42). Three project research staff coded the text and checked for reliability.
Results
Baseline characteristics
A total 284 participants were interviewed at the baseline enrolment. Participants’ average age was 28.8 ranging from 18–41 years old. Nearly 54% of participants had less than high education (Table 1). Most of the participants were unmarried or divorced. The majority of participants (63.5%) reported engaging in sex work from 1 to 5 years. Over 92% had sexual encounters with clients in guesthouses or hotels. Over 90% and 93% reported having experienced at least one pregnancy and at least one abortion respectively. The number of abortions ranged from 0–13 times with over 24% having three or more abortions. Most FSWs could list three contraceptive methods with the most common being contraceptive pills and condoms.
Table 1
| Characteristics | n (%) or mean [range] |
|---|---|
| Age (years), mean [range] | 28.8 [18–41] |
| <20 (18–19) | 10 (3.9) |
| 20–49 | 275 (96.1) |
| Education | |
| Under high school | 153 (53.9) |
| High school | 129 (45.4) |
| Above high school | 2 (0.7) |
| Ethnicity | |
| Kinh (majority) | 273 (96.1) |
| Other | 11 (3.9) |
| Marital status | |
| Unmarried | 162 (57.1) |
| Married | 18 (6.3) |
| Divorced | 104 (36.6) |
| Type of residence | |
| Owned a house/apart | 28 (9.9) |
| Rent | 256 (90.1) |
| Years of living in Hanoi, mean [range] | 5.3 [0–20] |
| Duration of sex work | |
| <1 year | 11 (3.9) |
| 1–5 years | 181 (63.7) |
| >5 years | 92 (32.4) |
| Venue of sex encounters with clients | |
| Guesthouses/hotels | 264 (93.0) |
| Sex workers’ houses | 6 (2.1) |
| Private places | 4 (1.4) |
| Clients’ houses | 10 (3.5) |
| Number of pregnancies, mean [range] | 2.6 [0–19] |
| Zero | 23 (9.7) |
| One | 53 (19.0) |
| Two | 69 (24.7) |
| Three and more | 130 (46.6) |
| Number of abortions, mean [range] | 1.9 [0–13] |
| Zero | 17 (6.9) |
| One | 109 (44.5) |
| Two | 59 (24.1) |
| Three and more | 60 (24.5) |
| Ever receiving professional* safe abortion counseling | |
| No | 100 (40.8) |
| Yes | 145 (59.2) |
*, from a licensed safe abortion specialist.
Improvements in safe abortion knowledge
Table 2 summarizes outcomes measured at baseline and at the 3-month follow-up surveys. Overall, there was a significant increase in abortion knowledge among the participants following the intervention. Specifically, FSWs’ knowledge of correct gestational ages (≤22 weeks) for medical abortion increased sharply from 78.9% at the baseline survey to 96.8% at the 3-month follow-up (P=0.001). Knowledge of correct gestational ages for medical abortion at the private clinic increased from 45.3% to 63.1% (P=0.001). Correct knowledge of using abortion pills on a gestational age (≤12 weeks) when medical abortion is allowed increased significantly from 51.2% to 71.7%% (P=0.001). Knowledge on understanding of consequences of unsafe abortion increased from 75.2% to 92.1% (P=0.001). However, there were no significant changes in knowledge on when to continue contraceptives after abortion (P=0.541).
Table 2
| Measurement | Baseline (%) | Follow up (%) | P value |
|---|---|---|---|
| FSWs correctly identified a gestational age for medical abortion/surgical abortion | 78.9 | 96.8 | 0.001 |
| FSWs correctly indicated a gestational age for medical abortion/surgical abortion at the private clinic | 45.3 | 63.1 | 0.001 |
| FSWs correctly indicated 2 types of abortion: medical and surgical abortion | 67.3 | 88.4 | 0.012 |
| FSWs correctly identified both public and private gynecological facilities providing abortion services | 38.6 | 56.6 | 0.001 |
| FSWs correctly identified knowledge on gestational age for abortion pills (≤12 weeks) | 51.2 | 71.7 | 0.001 |
| FSWs correctly reported knowledge on making safe abortion at home (≤7 weeks of gestational age) | 25.7 | 33.9 | 0.010 |
| FSWs correctly reported knowledge on at least one possible complication of abortion | 80.0 | 98.1 | 0.001 |
| FSWs correctly stated knowledge on when to continue contraceptives after abortion | 90.6 | 95.5 | 0.541 |
| FSWs correctly indicated that an abortion at home needs a medical professional providers’ consultation | 81.1 | 93.1 | 0.015 |
| FSWs correctly named at least one type of surgical abortion | 89.1 | 95.9 | 0.005 |
| FSWs received medical professional providers’ consultation on the last abortion | 62.8 | 68.3 | 0.245 |
| FSWs’ knowledge on consequences of unsafe abortion | 75.2 | 92.1 | 0.001 |
| FSWs reported perceived stigma and discrimination from healthcare providers | 36.5 | 27.8 | 0.036 |
| FSWs did not know where to find a safe abortion clinic | 18.2 | 8.9 | 0.042 |
| FSWs’ worry about the lack confidentiality | 23.3 | 15.5 | 0.035 |
FSW, female sex worker.
Reduction in perceived barriers to safe abortion services
As shown in Table 2, there were significant reductions in perceived barriers to safe abortion services (P<0.05): including concerns about stigma and discrimination from safe abortion service providers decreased from 36.5% to 27.8%; not knowing where to find a safe abortion clinic decreased from 18.2% to 8.9%; and worry about the lack of confidentiality decreased from 23.3% to 15.5%.
Intervention acceptability and user satisfaction with the iConnect app
On the 5-point Liker scale, 80% or more of the participants who attended post-test interviews gave score four or five, demonstrating their satisfaction with the iConnect app in terms of accessibility, usability, comprehensibility, helpfulness, and overall satisfaction (Table 3).
Table 3
| Questions | Mean score | % with the highest [5] score |
|---|---|---|
| The iConnect app provides a convenient access to safe abortion information and knowledge | 5 | 100 |
| The information provided by the iConnect app and automated text messages is easy to understand | 4.8 | 80 |
| The information provided by the iConnect app and automated text messages is helpful | 4.8 | 80 |
| The iConnect app is easy to use | 4.9 | 90 |
| How satisfied you are with the iConnect app | 4.9 | 90 |
Qualitative results
Improvement in participants’ knowledge was also reflected in qualitative data. Participants described the convenience of having the app to access to safe abortion knowledge when they had free time. Previously, they often looked for knowledge on issues related to health in general and abortion in particular from the print materials such as health promotion posters, leaflets or brochures. Ready access to information and knowledge made decision on safe abortion easier:
“… I think using the app is more convenient than health promotion leaflets and posters as those who are interested in reading the information can open the phone and read it right away. Whereas, it takes time for us to distribute leaflets and posters to the people and some of them do not read them immediately and left them elsewhere”. [Peer educator, age 23]
“…I really like this app because sometimes when I face a problem, I open the app and read the information on how to keep myself safe”. [Participant, age 25]
However, some participants suggested to improve the contents of the app as well as the chat features. One participant described difficulties in understand some jargons used in the messages, especially those related to medical knowledge, making it hard for FSWs to understand the whole meaning of the message.
“… I learned a lot of safe abortion knowledge from this program, but sometime I read some words that I do not understand the meaning. The language should be written in a more simple way for us to understand”. [Participant, age 25]
Knowledge gain
Several participants indicated that the messages taught them new and useful information, particularly messages on signs of pregnancy, safe abortion methods at home and at the clinics, post abortion safety, complications of abortion and contraceptive options.
“…I learnt new knowledge on how to have safe abortions and what to do when having bleeding. Oh, I also know how to prevent pregnancy safely now”. [Participant, age 23]
“… I read the information related to post abortion safety methods as this is applicable to my situation”. [Participant, age 23]
Some participants spoke of enhanced confidence as a result of using the app to get comprehensive information and knowledge about women’s abortion rights, safe abortions methods and manage abnormal signs after abortion rather than accessing other sources as they previously used such as using Google or asking friends.
“… the knowledge I gained from the app made me confident about choosing methods to prevent pregnancy and choosing safe abortion methods. I don’t have to do Google search or ask friends or parents to look for information concerning abortion anymore. I always hesitate to ask my friends about this.” [Participant, age 22]
Peer support
FSWs stated that the app facilitated conversation with other FSWs who had undergone similar experiences, via chat rooms. Some FSWs also introduced the app to other friends and interact with other FSWs in their social network.
“… I told my friends about the app, and some were very interested to know more…I then taught them to install and use the app and share the information on safe abortion and prevent unwanted pregnancies.” [Participant, age 23]
Intervention impact
When discussing the change that had occurred since the intervention, some FSWs described the benefits of using virtual counselling with healthcare providers, making it possible to communicate easily with healthcare providers and counselors.
“… I am still very young, and I always hesitate to visit clinics and talk directly with the healthcare providers about issues related to pregnancy and abortion because it is very inconvenient and embarrassed. So, I have used the app to get a virtual consultation with a doctor regarding my recent abortion. When using this app, I do not have to show my face to the counselors when we have a conversation”. [Participant, age 21]
Participants also described the benefits of app in terms of confidentiality and privacy.
“… previously when I have a question related to pregnancy, I often asked my friends, sisters, or relatives about it. But now I can find the information on the app, and I feel that I can keep it confidential and feel more comfortable”. [Participant, age 25]
“The app (iConnect) ensures privacy and confidentiality without telling my personal information. I do not feel hesitant when searching any sensitive information related to safe abortion. The app also allows fast access to doctors and get counseling without a need to travel to the clinic and meet doctors in person”. [Participant, age 22]
Discussion
This iConnect project is the first using an mHealth approach integrated with peer education to address a high risk of unsafe abortions among FSWs in Vietnam. With over 93% of FSWs who reported having at least one abortion, the project was a timely and novel response to the needs for safe abortion services among these vulnerable women. Capitalizing on the ubiquity of smartphones among the target population of FSWs, the intervention appeared to be highly feasible, accessible, and acceptable. Despite the lock down during the COVID-19 pandemic and a number of FSWs returned to their hometowns due to the short supply of clients in Hanoi, the project was still able to reach and maintain the intervention delivery to over 500 FSWs.
The results of both quantitative and qualitative assessments indicate that the intervention among FSWs showed significant improvements in women’s knowledge and behaviors about safe abortion. The reduction in perceived barriers faced by women when seeking safe abortion information and services was an important finding. In particular, the reductions in perceived stigma and discrimination from service providers might help promote women timely access to safe abortion services and prevent them from obtaining clandestine or unsafe abortion practices. The findings suggest that mHealth intervention may offer a promising strategy to bring safe abortion knowledge, to reduce perceived barriers as well as to improve access to safe abortion to a marginalized population of FSWs in Vietnam.
The project is a good example of smartphone-based intervention that integrated mobile technology with conventional peer-based education outreach. This integrated approach allowed peer educators maintain regular contact and delivery of education in a continuous fashion through multiple modes of interactivities (e.g., chat, call, text message), which otherwise is not feasible using conventional face-to-face communication. The use of digitalized education materials embedded in the iConnect app along with automated educational messages sent to women’s smartphones enabled women’s access to information at ‘anywhere and anytime’, reducing physical and psychological barriers associated with traditional face-to-face communication. Use of iConnect mobile app would have not only increased intensity and continuity of the intervention, but also would have enhanced the follow up and retention, minimizing attrition while optimizing the intervention impact, particularly for a highly mobile and hard- to- reach population like FSWs.
Additionally, the integrated mHealth approach utilized in the project appeared to be an effective tool that connects FSWs to available safe abortion services. Numerous studies have indicated that concerns about stigma and lack of privacy and confidentiality are key barriers preventing women from attending abortion clinics (43-45). The use of virtual confidential counseling has addressed these barriers by enabling women to access service providers at any time without a need to provide personal information or have face-to-face meetings at the clinics. Appointment scheduling followed by automated reminders and alerts were also effective in improving virtual clinic attendance.
Our study should be interpreted with caution in light of its limitations. This is a single-group, pre-post intervention design with no control group and therefore the study internal validity maybe affected, i.e., the changes in study outcomes may not be directly resulting from the intervention. As the study was conducted among FSWs in one city, the findings cannot be generalized to all FSWs in Vietnam. The study outcomes were based on self-report and therefore may suffer from recall and social desirability bias. Future research using a comparison group, randomized participants is needed to establish study impact and effectiveness. Finally, the qualitative method in this study involved a small sample size that was not sufficient to achieve data saturation for themes (46).
Conclusions
This study represents the first mobile app-based (iConnect) intervention among FSWs in Vietnam. The results indicate that the intervention significantly improved FSWs’ knowledge and behaviors on safe abortion and reduced their perceived barriers to available safe abortion services. These findings suggest that mHealth intervention is a feasible and effective approach for improving FSWs’ access to safe abortion services. However, it should be acknowledged that while improving access to safe abortion for FSWs is essential, it is a stopgap measure given the limited access of effective, safe, effective, affordable, and acceptable contraceptive care and services. This work must proceed in parallel with other efforts to improve access to SRH services that can help reduce unintended pregnancy among FSWs as well as promote reproductive justice and rights.
Acknowledgments
The authors acknowledge the valuable contributions of participants and the project investigators in Vietnam.
Funding: This work was supported by Grand Challenges Canada under Grant number PCT-OTP-1902-31681 OPTions Initiate: Mobile Connect- An integrated mHealth intervention to address unsafe abortion among female sex workers in Vietnam.
Footnote
Data Sharing Statement: Available at https://atm.amegroups.com/article/view/10.21037/mhealth-22-41/dss
Peer Review File: Available at https://mhealth.amegroups.com/article/view/10.21037/mhealth-22-41/prf
Conflicts of Interest: The authors have completed the ICMJE uniform disclosure form (available at https://mhealth.amegroups.com/article/view/10.21037/mhealth-22-41/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Institutional Review Board of the Institute for Social Development Studies, Hanoi, Vietnam. Verbal informed consent in Vietnamese was obtained from all FSWs in the study.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Semple SJ, Stockman JK, Pitpitan EV, et al. Prevalence and Correlates of Client-Perpetrated Violence against Female Sex Workers in 13 Mexican Cities. PLoS One 2015;10:e0143317. [Crossref] [PubMed]
- Kanayama Y, Yamada H, Yoshikawa K, et al. Mental Health Status of Female Sex Workers Exposed to Violence in Yangon, Myanmar. Asia Pac J Public Health 2022;34:354-61. [Crossref] [PubMed]
- Coetzee J, Gray GE, Jewkes R. Prevalence and patterns of victimization and polyvictimization among female sex workers in Soweto, a South African township: a cross-sectional, respondent-driven sampling study. Glob Health Action 2017;10:1403815. [Crossref] [PubMed]
- World Health Organization Regional Office for the Western Pacific. Sex work in Asia. 2001. Available online: https://apps.who.int/iris/handle/10665/207544, accessed 10/9/2022.
- Jonas A, Patel SV, Katuta F, et al. HIV Prevalence, Risk Factors for Infection, and Uptake of Prevention, Testing, and Treatment among Female Sex Workers in Namibia. J Epidemiol Glob Health 2020;10:351-8. [Crossref] [PubMed]
- Manopaiboon C, Prybylski D, Subhachaturas W, et al. Unexpectedly high HIV prevalence among female sex workers in Bangkok, Thailand in a respondent-driven sampling survey. Int J STD AIDS 2013;24:34-8. [Crossref] [PubMed]
- Chen Y, Shen Z, Morano JP, et al. Bridging the epidemic: a comprehensive analysis of prevalence and correlates of HIV, hepatitis C, and syphilis, and infection among female sex workers in Guangxi Province, China. PLoS One 2015;10:e0115311. [Crossref] [PubMed]
- Page K, Stein E, Sansothy N, et al. Sex work and HIV in Cambodia: trajectories of risk and disease in two cohorts of high-risk young women in Phnom Penh, Cambodia. BMJ Open 2013;3:e003095. [Crossref] [PubMed]
- Sedgh G, Singh S, Hussain R. Intended and unintended pregnancies worldwide in 2012 and recent trends. Stud Fam Plann 2014;45:301-14. [Crossref] [PubMed]
- Scorgie F, Chersich MF, Ntaganira I, et al. Socio-demographic characteristics and behavioral risk factors of female sex workers in sub-saharan Africa: a systematic review. AIDS Behav 2012;16:920-33. [Crossref] [PubMed]
- Ampt FH, Willenberg L, Agius PA, et al. Incidence of unintended pregnancy among female sex workers in low-income and middle-income countries: a systematic review and meta-analysis. BMJ Open 2018;8:e021779. [Crossref] [PubMed]
- Wahed T, Alam A, Sultana S, et al. Sexual and reproductive health behaviors of female sex workers in Dhaka, Bangladesh. PLoS One 2017;12:e0174540. [Crossref] [PubMed]
- Morineau G, Neilsen G, Heng S, et al. Falling through the cracks: contraceptive needs of female sex workers in Cambodia and Laos. Contraception 2011;84:194-8. [Crossref] [PubMed]
- Lim MS, Zhang XD, Kennedy E, et al. Sexual and reproductive health knowledge, contraception uptake, and factors associated with unmet need for modern contraception among adolescent female sex workers in China. PLoS One 2015;10:e0115435. [Crossref] [PubMed]
- Lafort Y, Greener R, Roy A, et al. Sexual and reproductive health services utilization by female sex workers is context-specific: results from a cross-sectional survey in India, Kenya, Mozambique and South Africa. Reprod Health 2017;14:13. [Crossref] [PubMed]
- Dhana A, Luchters S, Moore L, et al. Systematic review of facility-based sexual and reproductive health services for female sex workers in Africa. Global Health 2014;10:46. [Crossref] [PubMed]
- Khan MR, Turner AN, Pettifor A, et al. Unmet need for contraception among sex workers in Madagascar. Contraception 2009;79:221-7. [Crossref] [PubMed]
- Weldegebreal R, Melaku YA, Alemayehu M, et al. Unintended pregnancy among female sex workers in Mekelle city, northern Ethiopia: a cross-sectional study. BMC Public Health 2015;15:40. [Crossref] [PubMed]
- Maher L, Mooney-Somers J, Phlong P, et al. Condom negotiation across different relationship types by young women engaged in sex work in Phnom Penh, Cambodia. Glob Public Health 2013;8:270-83. [Crossref] [PubMed]
- Nguyen N, Londeree J, Nguyen LH, et al. Reproductive autonomy and contraceptive use among women in Hanoi, Vietnam. Contracept X 2019;1:100011. [Crossref] [PubMed]
- Tuoi Tre News. Vietnam’s abortion rate among world’s highest as contraception fails. Available online: https://tuoitrenews.vn/news/society/20170927/vietnams-abortion-rate-among-worlds-highest-as-contraception-fails/41775.html, accessed 07/28/2022.
- World Population Review Abortion Rates by Country. Available online: https://worldpopulationreview.com/country-rankings/abortion-rates-by-country, accessed 8/25/2022.
- Maris Stop International. MSI Vietnam. Available online: https://www.msichoices.org/where-we-work/vietnam/, accessed 08/22/2022.
- Fllek-Gibson, D. Vietnam tackles high abortion rates. Available online: https://www.aljazeera.com/features/2014/8/28/vietnam-tackles-high-abortion-rates, accessed 07/27/2022.
- Goldsamt L A., Clatts M C., Yu G, Le B, Colby D J.. Human Trafficking and Emerging Sex Risk Environments in Vietnam: A Preliminary Profile of a Sex Work “Shared House”. J Hum Traffick 2017;3:107-115. [Crossref] [PubMed]
- CARE Australia. Empowering female sex workers in Vietnam. Available online: https://www.dfat.gov.au/aid/who-we-work-with/ngos/ancp/news/Pages/empowering-female-sex-workers-in-vietnam, accessed 07/12/2022.
- Minh TT, Nhan DT, West GR, et al. Sex workers in Vietnam: how many, how risky? AIDS Educ Prev 2004;16:389-404. [Crossref] [PubMed]
- Le G, Khuu N, Tieu VTT, et al. Population Size Estimation of Venue-Based Female Sex Workers in Ho Chi Minh City, Vietnam: Capture-Recapture Exercise. JMIR Public Health Surveill 2019;5:e10906. [Crossref] [PubMed]
- Do K, Minichiello V, Hussain R, et al. Sexual history taking in general practice: managing sexually transmitted infections for female sex workers by doctors and assistant doctors in Vietnam. Int J STD AIDS 2015;26:55-64. [Crossref] [PubMed]
- WHO. mHealth-new horizons for health through mobile technologies. Geneva, Switzerland, 2011. Report No.: 3. Available online: https://apps.who.int/iris/handle/10665/44607
- Free C, Phillips G, Watson L, et al. The effectiveness of mobile-health technologies to improve health care service delivery processes: a systematic review and meta-analysis. PLoS Med 2013;10:e1001363. [Crossref] [PubMed]
- Gurman TA, Rubin SE, Roess AA. Effectiveness of mHealth behavior change communication interventions in developing countries: a systematic review of the literature. J Health Commun 2012;17:82-104. [Crossref] [PubMed]
- Marcolino MS, Oliveira JAQ, D'Agostino M, et al. The Impact of mHealth Interventions: Systematic Review of Systematic Reviews. JMIR Mhealth Uhealth 2018;6:e23. [Crossref] [PubMed]
- Ko JS, Stafylis C, Klausner JD. Mobile health promotion of human immunodeficiency virus self-testing in the United States. Mhealth 2020;6:10. [Crossref] [PubMed]
- Smith C, Gold J, Ngo TD, et al. Mobile phone-based interventions for improving contraception use. Cochrane Database Syst Rev 2015;2015:CD011159. [Crossref] [PubMed]
- Aunon FM, Okada E, Wanje G, et al. Iterative Development of an mHealth Intervention to Support Antiretroviral Therapy Initiation and Adherence Among Female Sex Workers in Mombasa, Kenya. J Assoc Nurses AIDS Care 2020;31:145-56. [Crossref] [PubMed]
- Ampt FH, L'Engle K, Lim MSC, et al. A Mobile Phone-Based Sexual and Reproductive Health Intervention for Female Sex Workers in Kenya: Development and Qualitative Study. JMIR Mhealth Uhealth 2020;8:e15096. [Crossref] [PubMed]
- Vietnam Ministry of Information and Communications. Vietnam targets 85% smartphone usage by end of 2022. Available online: https://english.mic.gov.vn/Pages/TinTuc/153538/Vietnam-targets-85--smartphone-usage-by-end-of-2022.html (accessed November 16, 2022).
- Statista. Smartphone market in Vietnam - statistics & facts. 2022. Available online: https://www.statista.com/topics/9168/smartphone-market-in-vietnam/#topicOverview (accessed November 15, 2022).
- Vo, H. Hanoi publicizes sex workers’ hangouts. Available online: https://e.vnexpress.net/news/news/hanoi-publicizes-sex-workers-hangouts-3846192.html#:~:text=Hanoi%20launched%20a%20software%20to,engaging%20in%20commercial%20sex%20work (accessed November 30, 2022).
- Friese S. User’s manual for ATLAS.ti 6.0, ATLAS.ti Scientific Software Development. Berlin: GmbH, 2013.
- Schensul S. Using ethnography to build a survey instrument. CAM 1993;5:9. [Crossref]
- Wahed T, Alam A, Sultana S, et al. Barriers to sexual and reproductive healthcare services as experienced by female sex workers and service providers in Dhaka city, Bangladesh. PLoS One 2017;12:e0182249. [Crossref] [PubMed]
- Hubach RD, Zipfel R, Muñoz FA, et al. Barriers to sexual and reproductive care among cisgender, heterosexual and LGBTQIA + adolescents in the border region: provider and adolescent perspectives. Reprod Health 2022;19:93. [Crossref] [PubMed]
- Thongmixay S, Essink DR, Greeuw T, et al. Perceived barriers in accessing sexual and reproductive health services for youth in Lao People's Democratic Republic. PLoS One 2019;14:e0218296. [Crossref] [PubMed]
- Vasileiou K, Barnett J, Thorpe S, et al. Characterizing and justifying sample size sufficiency in interview-based studies: systematic analysis of qualitative health research over a 15-year period. BMC Med Res Methodol 2018;18:148. [Crossref] [PubMed]
Cite this article as: Ngo A, Nguyen VT, Phan H, Pham V, Ngo C, Nguyen L, Ha T. Effectiveness of mHealth intervention on safe abortion knowledge and perceived barriers to safe abortion services among female sex workers in Vietnam. mHealth 2023;9:3.