Towards research-tested smartphone applications for preventing breast cancer
Worldwide, about 521,907 deaths occur from breast cancer each year (1,2). In the U.S., breast cancer accounts for more cancer deaths in women than any site other than lung cancer. An estimated 40,450 deaths from breast cancer will occur in 2016 (1). Breast cancer is the most commonly diagnosed invasive cancer in the U.S. for women of all racial and ethnic groups, with an estimated 246,660 new cases diagnosed in 2016 (1).
A variety of risk factors for breast cancer have been well-established by epidemiologic studies including race, ethnicity, family history of cancer, and genetic traits, as well as modifiable exposures such as increased alcohol consumption, physical inactivity, obesity after menopause, exogenous hormones, and certain female reproductive factors (1,2). Efforts to prevent breast cancer and other chronic illnesses have focused on promoting physical activity, healthy diet and nutrition, and avoidance of excessive alcohol consumption (3-5).
About 58% of adults in the U.S. owned a smartphone in 2013 and the percentage is projected to surpass 90% by 2020 (6,7). Smartphone applications (apps) offer a low-cost and effective strategy for breast cancer prevention in women through behavioral change. This includes educational and behavioral interventions for weight management, healthy eating (low calorie diet with adequate consumption of whole grains, fruit, and non-starchy vegetables and decreased saturated fat, red meat, processed meat, added sugars, and refined grains), limiting alcohol intake, physical activity, breastfeeding, and avoidance of carcinogenic exposures such as combined estrogen and progestin hormones and cigarette smoking. However, there are currently no research-tested smartphone apps for breast cancer prevention that are suitable for women with varying levels of health literacy and eHealth literacy.
In this perspective, we consider modifiable risk factors for breast cancer in women in relation to the development of smartphone apps to promote healthy behaviors associated with breast cancer-risk reduction. First, we provide a summary of breast cancer risk factors that are modifiable through behavioral change including their corresponding relative risk. Second, we discuss scientific issues related to the development of smartphone apps for the primary prevention of breast cancer and offer suggestions for further research in this area. Smartphone apps for preventing breast cancer should ideally be tailored for women at different life stages (e.g., young women, women who are post-menopausal, and older women). Topics such as breastfeeding and oral contraceptives are appropriate for younger women. Topics such as weight management, physical activity, the need to avoid cigarette smoking, and dispelling breast cancer myths are appropriate for women of all ages. As women age, topics such as hormone replacement therapy or comorbid health conditions become more important to address.
Modifiable risk factors for breast cancer
Results from the Women’s Health Initiative randomized trial and epidemiologic studies indicate that hormone replacement therapy after menopause increases breast cancer risk (8-10). Use of a regimen that includes both estrogen and progesterone has been associated with a higher risk of breast cancer than the use of estrogen alone (11). Parity and older age at first full-term pregnancy may influence breast cancer risk through long-term effects on sex hormone levels or by other biological mechanisms. Breast feeding reduces a woman’s risk of breast cancer and is an important modifiable preventive behavior (12,13). Longer duration of breast feeding has been associated with a greater reduction in breast cancer risk.
The high prevalence of obesity in the U.S. population is a serious threat to women’s health because of causal linkages between obesity and cancer of the breast, colon, and other sites, and other adverse health consequences (14,15). Nutrition, physical activity, and energy balance are important determinants of weight loss and maintenance of healthy weight. However, approximately 35% of adults in the U.S. are obese (16). Based on data from the 2013 Behavioral Risk Factor Surveillance Survey (BRFSS), only half of U.S. adults (50.2%) met guidelines for physical activity and an additional 11.7% only partially met the guidelines (Yoo et al., unpublished). Women are less likely than men to meet guidelines for physical activity (48.6% vs. 52.5%). Evidence from epidemiologic studies indicates that high levels of physical activity reduce breast cancer risk in women. The possible biological mechanisms include the influences of physical activity on body composition, insulin resistance, and circulating levels of sex steroid hormones (17). Eating non-starchy vegetables may also lower the risk of some breast cancers. A pooled analysis of data from 20 epidemiologic studies found that eating vegetables (comparing the highest vs. lowest vegetable intake) lowered the risk of estrogen receptor-negative breast cancers (18). Eating fruit may also lower breast cancer risk. A meta-analysis of data from 15 studies found that eating fruit (comparing the highest vs. lowest fruit intake) lowered the risk of breast cancer (19).
Recent studies indicate that long-term, heavy cigarette smoking may also increase breast cancer risk, particularly among women who start smoking before their first pregnancy (1). Shift work with disruption of circadian rhythm has been associated with higher breast cancer risk (20). Modifiable risk factors for breast cancer that could be addressed in a smartphone app for preventing breast cancer in women are shown in (Table 1). Based upon attributable risks, about 30–35% of breast cancers could potentially be prevented by addressing obesity, physical inactivity, alcohol consumption, and HRT (29,30).
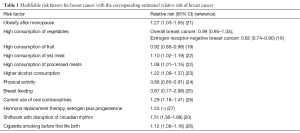
Full table
Discussion
In order to reduce breast cancer risk through the adoption and maintenance of healthy behaviors, multiple modifiable risk factors must be addressed as the increased risk associated with individual factors is modest. Established interventions for weight loss through healthy eating, caloric restriction, and physical activity, such as clinic-based interventions, one-on-one education, and small group education, are resource-intensive, which limits their widespread dissemination. Smartphone apps provide a useful and low-cost way to disseminate information to the general population about weight loss through health eating, physical activity, and other behaviors associated with reduced risk of breast cancer and other chronic illnesses. Common behavioral change techniques used in apps for health promotion include providing feedback, goal-setting, and self-monitoring (31). Although studies indicate that smartphone apps can be an effective intervention for smoking cessation, improving diet and nutrition, and encouraging physical activity (6,32,33), a breast cancer prevention app should ideally address multiple modifiable risk factors for breast cancer and be a part of overall healthy messages for promoting women’s health. However, it can be challenging to modify health behaviors, especially multiple behaviors at once. Culturally tailored cancer prevention apps are also needed for population subgroups. In addition, women who do not have a positive family history of breast cancer or a close friend who developed breast cancer may not see the need for modifying behaviors in order to reduce their risk of the disease. Therefore, it is likely that a variety of research-tested apps will be needed to meet the needs of all women.
Although many smartphone applications (apps) are available from major smartphone platforms (e.g., Android, iPhone, Windows phone) on breast cancer topics, few have been tested for acceptability or effectiveness (34,35). In addition, few of these apps are based on theories of health behavior change, most do not include evidence-based features such as self-monitoring and reinforcement, and existing apps often do not provide evidence-based recommendations for breast cancer risk reduction (32,34,36). Breast cancer apps commonly provide information about guidelines for the early detection of breast cancer. The U.S. Preventive Services Task Force (USPSTF) recommends screening mammography every two years as there is convincing evidence from randomized controlled trials that screening mammography reduces breast cancer mortality, with a greater absolute reduction for women aged 50 to 74 years than for younger women (37). For women who are aged 40 to 49 years (who are not at increased risk by virtue of a known genetic mutation) the USPSTF concludes that the decision to start regular, biennial screening mammography before the age of 50 years should be an individual one and take patient context into account, including the patient’s values regarding specific benefits and harms. The American Cancer Society (ACS) has also provided recommendations for breast cancer screening (38).
A further issue is that many existing breast cancer apps are designed for use by women who have been diagnosed with breast cancer and are concerned about treatment issues or how best to avoid recurrence of their illness. However, there is overlap between healthy behaviors recommended for the primary prevention of breast cancer and those for reducing a women’s risk of breast cancer recurrence or mortality.
Smartphone apps for preventing breast cancer should ideally be tailored for women at different life stages (for example, young women, women who are post-menopausal, and older women). Topics such as breastfeeding and oral contraceptives are appropriate for younger women. Topics such as weight management, physical activity, the need to avoid cigarette smoking, and dispelling breast cancer myths are appropriate for women of all ages. As women age, topics such as hormone replacement therapy or comorbid health conditions become more important to address through apps intended for patients or health care providers. A smartphone app for breast cancer prevention may not be suitable for women with certain chronic health conditions. For example, people who have a history of myocardial infarction, angina, coronary artery bypass graft surgery, coronary angioplasty, or congestive heart failure should consult with their own physician before engaging in any physical activity regimen. Similarly, diabetic individuals should receive advice about diet and nutrition from a health care provider such as a physician or registered dietician.
Health promotion apps should be grounded in a behavioral theory or framework such as social cognitive theory (39). Elements of social cognitive theory include goal setting, self-assessment (e.g., food intake, food and beverage composition, and caloric intake), self-monitoring (e.g., minutes of physical activity per day), and reinforcement of positive behaviors. Self-monitoring is strongly associated with behavior change (40). By including educational information about modifiable causes of breast cancer (e.g., the potential benefits of weight loss through healthy eating, caloric restriction, limiting alcohol intake, and physical activity), an app intervention could also incorporate elements of the Health Belief Model (HBM) (41). The HBM posits that a person’s beliefs about a health concern such as breast cancer, their perceived benefits of an action (e.g., adopting a healthy diet, engaging in physical activity, breast feeding) and barriers to action, and self-efficacy explain engagement in health promoting behavior (41). The HBM suggests that a stimulus or cue to action must be present to trigger health-promoting behavior. A smartphone app can provide triggers to promote healthy behaviors. For example, they can enable users to record minutes of physical activity per day in order to receive instant feedback on their energy expenditure. To increase self-efficacy, an app can provide information about practical steps that can be taken to maintain health such as healthy recipes and menu suggestions. Apps can also allow users to set a weight loss goal and to self-monitor daily energy intake toward achieving that goal and serve as a cue for action.
Dietary guidelines are available that were developed jointly by the U.S. Department of Agriculture (USDA) and the Department of Health and Human Services (HHS) (42). In addition, information about healthy eating can be based upon: (I) the ACS guidelines on nutrition and physical activity for cancer prevention (5), which were associated with a 22% lower risk of breast cancer in an analysis of data from the Women’s Health Initiative (43); and (II) the World Cancer Research Fund/American Institute for Cancer Research nutrition-related recommendations for cancer prevention (3), which were associated with a 51% reduction in risk of breast cancer in epidemiologic studies (4). Apps can also utilize information and graphics from the USDA’s ChooseMyPlate program which provides practical information to help consumers build healthier diets with user-friendly nutrition information (44). Physical activity guidelines are available that were developed by HHS and ACS. The 2008 Physical Activity Guidelines for Americans emphasize that all adults should avoid inactivity (45). Some physical activity is better than none, and adults who participate in any amount of physical activity gain some health benefits. For substantial health benefits, adults should do at least 150 min (2 h and 30 min) a week of moderate-intensity, or 75 min (1 h and 15 min) a week of vigorous-intensity aerobic physical activity, or an equivalent combination of moderate- and vigorous-intensity aerobic activity. Aerobic activity should be performed in episodes of at least 10 min, and preferably, it should be spread throughout the week (45). Apps can include health messages about the importance of routine physical activity for weight management and the potential health benefits.
Smartphone apps for breast cancer prevention should be suitable for people with varying levels of health literacy. Cancer prevention messages are often written at advanced reading levels for individuals with marginal literacy skills (46). For mobile apps to be useful for encouraging healthy behaviors in diverse populations, they must be suitable for people with varying levels of health literacy and eHealth literacy (47-50).
Future developments in smartphone apps for breast cancer prevention should include apps that are tailored for specific cultural, racial, and ethnic groups. Substantial disparities occur in breast cancer incidence and survival. In the U.S., age-standardized breast cancer incidence rates are higher among non-Hispanic white women than non-Hispanic black women, Asian and Pacific Islander, American Indian and Alaska Native, or Hispanic women, although black women have a higher breast cancer mortality rate than women from other racial groups (1). Black-white differences in survival persist even after accounting for disease stage and tumor characteristics (51). Since 1975, the 5-year relative survival rate for breast cancer has increased for both African American and white women (1). However, there remains a substantial racial difference (1). This disparity in breast cancer survival is due to both later stage at diagnosis and poorer stage-specific survival among African American women (1). In the U.S., black race and Hispanic ethnicity have been associated with later stage at breast cancer diagnosis.
In conclusion, smartphone apps for preventing breast cancer should be tailored for women at different life stages (e.g., young women, women who are post-menopausal, and older women). Topics such as breastfeeding and oral contraceptives are appropriate for younger women. Topics such as weight management, physical activity, the need to avoid cigarette smoking, and dispelling breast cancer myths are appropriate for women of all ages. As women age, topics such as hormone replacement therapy or comorbid health conditions become more important to address. Apps designed to provide continuing education to health care providers may also be helpful. In order to reduce breast cancer risk through the adoption and maintenance of healthy behaviors, multiple modifiable risk factors must be addressed. A smartphone app for breast cancer prevention may not be suitable for all women, e.g., those with certain chronic health conditions. Apps for breast cancer prevention should be grounded in a behavioral theory or framework and should be suitable for people with varying levels of health literacy. Future developments in smartphone apps for breast cancer prevention should include apps that are tailored for specific cultural, racial, and ethnic groups.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Siegel RL, Miller KD, Jemal A. Cancer statistics 2016. CA Cancer J Clin 2016;66:7-30. [Crossref] [PubMed]
- Coughlin SS, Cypel Y. Epidemiology of breast cancer in women. In: Ahmad A, editor. Breast cancer metastasis and drug resistance: challenges and progress. New York: Springer Publishing; 2012.
- AICR. Food, nutrition, physical activity, and the prevention of cancer: a global perspective. Washington, DC: AICR, 2007.
- Harris HR, Bergkvist L, Wolk A. Adherence to the world cancer research fund/American institute for cancer research recommendations and breast cancer risk. Int J Cancer 2016;138:2657-64. [Crossref] [PubMed]
- Kushi LH, Doyle C, McCullough M, et al. American cancer society guidelines on nutrition and physical activity for cancer prevention: reducing the risk of cancer with healthy food choices and physical activity. CA Cancer J Clin 2012;62:30-67. [Crossref] [PubMed]
- Bricker JB, Mull KE, Kientz JA, et al. Randomized, controlled pilot trial of a smartphone app for smoking cessation using acceptance and commitment therapy. Drug Alcohol Depend 2014;143:87-94. [Crossref] [PubMed]
- Smith A. US smartphone ownership in 2015. Available online: http://www.pewinternet.org/2015/04/01/us-smartphone-use-in-2015/
- Chlebowski RT, Hendrix SL, Langer RD, et al. Influence of estrogen plus progestin on breast cancer and mammography in healthy postmenopausal women: the Women's Health Initiative Randomized Trial. JAMA 2003;289:3243-53. [Crossref] [PubMed]
- Reeves GK, Beral V, Green J, et al. Hormonal therapy for menopause and breast-cancer risk by histological type: a cohort study and meta-analysis. Lancet Oncol 2006;7:910-8. [Crossref] [PubMed]
- Calle EE, Feigelson HS, Hildebrand JS, et al. Postmenopausal hormone use and breast cancer associations differ by hormone regimen and histologic subtype. Cancer 2009;115:936-45. [Crossref] [PubMed]
- Chlebowski RT, Manson JE, Anderson GL, et al. Estrogen plus progestin and breast cancer incidence and mortality in the women's health initiative observational study. J Natl Cancer Inst 2013;105:526-35. [Crossref] [PubMed]
- American college of obstetricians and gynecologists committee on health care for underserved women. Breastfeeding in underserved women: increasing initiation and continuation of breastfeeding. Available online: http://www.acog.org/Resources-And-Publications/Committee-Opinions/Committee-on-Health-Care-for-Underserved-Women/Breastfeeding-in-Underserved-Women-Increasing-Initiation-and-Continuation-of-Breastfeeding
- Jones KM, Power ML, Queenan JT, et al. Racial and ethnic disparities in breastfeeding. Breastfeed Med 2015;10:186-96. [Crossref] [PubMed]
- Dietz WH. The response of the US centers for disease control and prevention to the obesity epidemic. Annu Rev Public Health 2015;36:575-96. [Crossref] [PubMed]
- Sallis JF, Glanz K. Physical activity and food environments: solutions to the obesity epidemic. Milbank Q 2009;87:123-54. [Crossref] [PubMed]
- Johnson NB, Hayes LD, Brown K, et al. CDC National Health Report: leading causes of morbidity and mortality and associated behavioral risk and protective factors--United States, 2005-2013. MMWR Suppl 2014;63:3-27. [PubMed]
- Coughlin SS, Smith SA. The Insulin-like growth factor axis, adipokines, physical activity, and obesity in relation to breast cancer incidence and recurrence. Cancer Clin Oncol 2015;4:24-31. [Crossref] [PubMed]
- Jung S, Spiegelman D, Baglietto L, et al. Fruit and vegetable intake and risk of breast cancer by hormone receptor status. J Natl Cancer Inst 2013;105:219-36. [Crossref] [PubMed]
- Aune D, Chan DS, Vieira AR, et al. Fruits, vegetables and breast cancer risk: a systematic review and meta-analysis of prospective studies. Breast Cancer Res Treat 2012;134:479-93. [Crossref] [PubMed]
- Megdal SP, Kroenke CH, Laden F, et al. Night work and breast cancer risk: a systematic review and meta-analysis. Eur J Cancer 2005;41:2023-32. [Crossref] [PubMed]
- van den Brandt PA, Spiegelman D, Yaun SS, et al. Pooled analysis of prospective cohort studies on height, weight, and breast cancer risk. Am J Epidemiol 2000;152:514-27. [Crossref] [PubMed]
- Guo J, Wei W, Zhan L. Red and processed meat intake and risk of breast cancer: a meta-analysis of prospective studies. Breast Cancer Res Treat 2015;151:191-8. [Crossref] [PubMed]
- Key J, Hodgson S, Omar RZ, et al. Meta-analysis of studies of alcohol and breast cancer with consideration of the methodological issues. Cancer Causes Control 2006;17:759-70. [Crossref] [PubMed]
- Wu Y, Zhang D, Kang S. Physical activity and risk of breast cancer: a meta-analysis of prospective studies. Breast Cancer Res Treat 2013;137:869-82. [Crossref] [PubMed]
- Nelson HD, Zakher B, Cantor A, et al. Risk factors for breast cancer for women aged 40 to 49 years: a systematic review and meta-analysis. Ann Intern Med 2012;156:635-48. [Crossref] [PubMed]
- Collaborative group on hormonal factors in breast cancer. Breast cancer and hormonal contraceptives: collaborative reanalysis of individual data on 53 297 women with breast cancer and 100 239 women without breast cancer from 54 epidemiological studies. Lancet 1996;347:1713-27. [Crossref] [PubMed]
- Collaborative group on hormonal factors in breast cancer. Breast cancer and hormone replacement therapy: collaborative reanalysis of data from 51 epidemiological studies of 52,705 women with breast cancer and 108,411 women without breast cancer. Collaborative Group on Hormonal Factors in Breast Cancer. Lancet 1997;350:1047-59. [Crossref] [PubMed]
- Gaudet MM, Gapstur SM, Sun J, et al. Active smoking and breast cancer risk: original cohort data and meta-analysis. J Natl Cancer Inst 2013;105:515-25. [Crossref] [PubMed]
- Wilson LF, Page AN, Dunn NA, et al. Population attributable risk of modifiable risk factors associated with invasive breast cancer in women aged 45-69 years in Queensland, Australia. Maturitas 2013;76:370-6. [Crossref] [PubMed]
- Dartois L, Fagherazzi G, Baglietto L, et al. Proportion of premenopausal and postmenopausal breast cancers attributable to known risk factors: Estimates from the E3N-EPIC cohort. Int J Cancer 2016;138:2415-27. [Crossref] [PubMed]
- Azar KM, Lesser LI, Laing BY, et al. Mobile applications for weight management: theory-based content analysis. Am J Prev Med 2013;45:583-9. [Crossref] [PubMed]
- Coughlin SS, Whitehead M, Sheats JQ, et al. Smartphone applications for promoting healthy diet and nutrition: a literature review. Jacobs J Food Nutr 2015;2:021.
- Coughlin SS, Whitehead M, Sheats JQ, et al. A review of smartphone applications for promoting physical activity. Jacobs J Community Med 2016;2.
- Coughlin SS. Intervention approaches for addressing breast cancer disparities among african american women. Ann Transl Med Epidemiol 2014;1:1001. [PubMed]
- Coughlin SS, Jacobs M, Thind H, et al. On the need for research-tested smartphone applications for reducing exposures to known or suspected breast carcinogens in work and home environments. J Environ Health Sci 2015;1.
- Mobasheri MH, Johnston M, King D, et al. Smartphone breast applications - what's the evidence? Breast 2014;23:683-9. [Crossref] [PubMed]
- U.S. Preventive services task force. Final recommendation statement breast cancer screening, November 2016. Available online: http://www.uspreventiveservicestaskforce.org/Page/Document/RecommendationStatementFinal/breast-cancer-screening
- Smith RA, Manassaram-Baptiste D, Brooks D, et al. Cancer screening in the United States, 2015: a review of current American cancer society guidelines and current issues in cancer screening. CA Cancer J Clin 2015;65:30-54. [Crossref] [PubMed]
- Bandura A. Social foundations of thought and action: a social cognitive theory. Englewood Cliffs, NJ: Prentice-Hall, 1986: xiii 617.
- Burke LE, Wang J, Sevick MA. Self-monitoring in weight loss: a systematic review of the literature. J Am Diet Assoc 2011;111:92-102. [Crossref] [PubMed]
- Janz NK, Becker MH. The Health Belief Model: a decade later. Health Educ Q 1984;11:1-47. [Crossref] [PubMed]
- HHS 2015-2020 Dietary Guidelines for Americans. Available online: http://health.gov/dietaryguidelines/
- Thomson CA, McCullough ML, Wertheim BC, et al. Nutrition and physical activity cancer prevention guidelines, cancer risk, and mortality in the women's health initiative. Cancer Prev Res (Phila) 2014;7:42-53. [Crossref] [PubMed]
- USDA ChooseMyPlate. Available online: http://www.choosemyplate.gov/
- HHS 2008 Physical Activity Guidelines for Americans. Available online: http://health.gov/paguidelines/
- Friedman DB, Hoffman-Goetz L. Assessment of cultural sensitivity of cancer information in ethnic print media. J Health Commun 2006;11:425-47. [Crossref] [PubMed]
- Institute of Medicine. Health literacy: a prescription to end confusion. Washington, DC: National Academies Press, 2004.
- Norman CD, Skinner HA. eHealth literacy: essential skills for consumer health in a networked world. J Med Internet Res 2006;8:e9. [Crossref] [PubMed]
- Institute of medicine (US) roundtable on health literacy. Health literacy, eHealth, and communication: putting the consumer first: Workshop summary. Washington, DC: National Academies Press (US), 2009.
- Tennant B, Stellefson M, Dodd V, et al. eHealth literacy and Web 2.0 health information seeking behaviors among baby boomers and older adults. J Med Internet Res 2015;17:e70. [Crossref] [PubMed]
- Gerend MA, Pai M. Social determinants of Black-White disparities in breast cancer mortality: a review. Cancer Epidemiol Biomarkers Prev 2008;17:2913-23. [Crossref] [PubMed]
Cite this article as: Coughlin SS, Thind H, Liu B, Wilson LC. Towards research-tested smartphone applications for preventing breast cancer. mHealth 2016;2:26.


